The new coronavirus—officially known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—is a recently discovered coronavirus that causes the illness COVID-19 (World Health Organization (WHO), 2020a). Coronavirus is one of the major pathogens that primarily target the human respiratory system. Previous outbreaks of coronaviruses (CoVs) include the severe acute respiratory syndrome (SARS)-CoV and the Middle East respiratory syndrome (MERS)-CoV, which have been previously characterised as agents that are a great public health threat.
Origins
In late December 2019, a cluster of patients were admitted to hospitals in Wuhan, Hubei Province, China, with an initial diagnosis of pneumonia of an unknown aetiology. These patients were epidemiologically linked to a seafood and wet animal wholesale market in Wuhan (Bogoch et al, 2020; Lu et al, 2020). Early reports predicted the onset of a potential coronavirus outbreak (Rothan and Byrareddy, 2020).
Current statistics
At the time of writing, the UK currently has 19 522 confirmed cases (Table 1). The figures come from data published by Public Health England (PHE) (2020a), working with the Department for Health and Social Care and Health Protection Scotland. These data are kept under constant review.
| Confirmed UK cases: 19 522 | Deaths | |||
|---|---|---|---|---|
| England 16 487 | Scotland 1384 | Wales 1241 | Northern Ireland 410 | UK 1228 |
Reports suggest that there are currently 314 053 confirmed cases of COVID-19 worldwide, with 13 556 deaths and 95 874 recovered (Worldometer.info/coronavirus).
Signs and symptoms
Most people infected with the COVID-19 virus will experience a mild-to-moderate respiratory illness and recover without requiring special treatment. Older people and those with underlying medical problems, such as cardiovascular disease, diabetes mellitus, chronic respiratory diseases and cancer are more likely to develop a serious illness and are at risk of death (WHO, 2020a). Common symptoms are listed in Box 1.
Prevention
The best way to prevent and slow down transmission is to be well informed about the COVID-19 virus and how it is transmitted. WHO (2020a) recommend several steps for prevention (Box 2).
The virus is transmitted primarily through droplets of saliva or discharge from the nose when an infected person coughs or sneezes, so it is important that everyone also practices respiratory etiquette (for example, by coughing into a flexed elbow or tissue).
People with mild symptoms who are otherwise healthy should self-isolate and stay at home, especially if they have a fever above 37.8°C and a new or continuous cough (NHS website, 2020).
To protect other people, it is suggested that people do not go to their GP surgery, pharmacy or hospital, and that they should stay at home for 7 days if they live alone, or 14 days if they live with other people. The 14 days starts from the day the first person in the home started having symptoms. Other people in the household also need to self-isolate for 14 days. This is because it can take 14 days for symptoms to appear (NHS website, 2020).
If a person lives with someone who is 70 years or over, has a long-term health condition, is pregnant or has a weakened immune system, it is recommended that they try to find somewhere else for them to stay for 14 days (NHS website, 2020).
The NHS website (2020) contains useful information that can be recommended to patients, including about mental health during the coronavirus outbreak.
Some key facts about the WHO's actions on the coronavirus are set out in Box 3.
Social distancing
As advised by the UK Government (PHE, 2020), social distancing measures are steps people can take to reduce physical social interaction. This will help reduce the transmission of the coronavirus. The Government advises the following steps in relation to social distancing (PHE, 2020):
Clinical management and treatment of COVID-19
There have been concerns that the UK does not have enough intensive care beds to cope with the number of people who will fall ill, and that the country could end up in a similar situation to Italy (The Guardian, 2020). In Italy, hospitals have been overwhelmed with COVID-19 patients and doctors have reportedly been forced to discriminate between patients based crudely on age alone. The UK has about half the number of critical care beds per head of population as Italy and intensive care doctors here have been calling for central guidance on triage to be issued (Nuki, 2020).
Currently, there are no specific or approved vaccines or treatments for COVID-19. However, there are many ongoing clinical trials evaluating potential treatments. A phase 1 clinical trial evaluating an investigational vaccine designed to protect against COVID-19 has begun at Kaiser Permanente Washington Health Research Institute (KPWHRI) in Seattle, USA (National Institutes of Health (NIH), 2020). The National Institute of Allergy and Infectious Diseases (NIAID), part of the NIH, is funding the trial. KPWHRI is part of NIAID's Infectious Diseases Clinical Research Consortium. The open-label trial will enrol 45 healthy adult volunteers aged 18 to 55 years over approximately 6 weeks. The first participant received the investigational vaccine on 16 March 2020 (NIH, 2020). The vaccine is called mRNA-1273 and was developed by NIAID scientists and their collaborators at the biotechnology company Moderna Inc, based in Cambridge, Massachusetts. The Coalition for Epidemic Preparedness Innovations (CEPI) supported the manufacturing of the vaccine candidate for the phase 1 clinical trial.
Clinical management
Patients with a mild clinical presentation may not initially require hospitalisation. However, clinical signs and symptoms may worsen with progression to lower respiratory tract disease in the second week of illness; all patients should be monitored closely for any changes in their vital signs, oxygen saturations, respiratory rate, blood pressure, pulse, changes in consciousness and blood glucose levels (if appropriate) (Centres for Disease Control and Prevention (CDC), 2020). Clinical staff should use the National Early Warning Score (NEWS 2) to track a patient with COVID-19 and to note deterioration in the patient's condition (Royal College of Physicians (RCP), 2017).
The CDC (2020) recommends that corticosteroids should be avoided, because of the potential for prolonging viral replication as observed in MERS-CoV patients, unless indicated for other reasons such as an exacerbation of chronic obstructive pulmonary disease or for septic shock, according to the Surviving Sepsis guidelines for adults and children (Rhodes et al, 2017).
WHO clinical guidelines
In March 2020, the WHO published guidelines entitled ‘Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected’ (WHO, 2020b). This was the second edition (version 1.2) of this document, first published in 2019. This 2020 guideline stipulates the screening and triage process, and sets out the clinical syndromes associated with COVID-19, including mild illness, pneumonia, severe pneumonia, and acute respiratory distress syndrome (ARDS), sepsis and septic shock. Section 6 addresses the management of severe COVID-19: oxygen therapy and monitoring.
Management of severe COVID-19: oxygen therapy and monitoring
The WHO advises the following on this topic and includes several ‘remarks’ or notes about specific patients.
‘Give supplemental oxygen therapy immediately to patients with SARI and respiratory distress, hypoxaemia or shock and target >94%’.
Remarks for adults:
Adults with emergency signs (obstructed or absent breathing, severe respiratory distress, central cyanosis, shock, coma or convulsions) should receive airway management and oxygen therapy during resuscitation to target SpO2 greater than or equal to (≥) 94%. Initiate oxygen therapy at 5 L/min and titrate flow rates to reach target SpO2 ≥93% during resuscitation; or use a face mask with reservoir bag (at 10–15 L/min) if the patient is in a critical condition. Once the patient is stable, the target is greater than 90% SpO2 in non-pregnant adults and ≥92–95% in pregnant patients.
Remarks for children:
Children with emergency signs (obstructed or absent breathing, severe respiratory distress, central cyanosis, shock, coma or convulsions) should receive airway management and oxygen therapy during resuscitation to target SpO2 ≥94% otherwise, the target SpO2 is ≥90%. Use of nasal prongs or nasal cannula is preferred in young children, as it may be better tolerated.
Remark:
All areas where patients with SARI are cared for should be equipped with pulse oximeters, functioning oxygen systems and disposable, single-use, oxygen-delivering interfaces (nasal cannula, nasal prongs, simple face masks and masks with a reservoir bag).
‘Closely monitor patients with COVID-19 for signs of clinical deterioration, such as rapidly progressive respiratory failure and sepsis and respond immediately with supportive care interventions.’
Remark 1:
Patients hospitalised with COVID-19, require regular monitoring of vital signs and, where possible, utilisation of medical early warning scores (eg NEWS2) that facilitate early recognition and escalation of the deteriorating patient.
Remark 2:
Haematology and biochemistry laboratory testing, and ECG should be performed at admission and as clinically indicated to monitor for complications, such as acute liver injury, acute kidney injury, acute cardiac injury or shock. Application of timely, effective and safe supportive therapies is the cornerstone of therapy for patients that develop severe manifestations of COVID-19.
Remark 3:
For pregnant women—after resuscitation and stabilisation of the pregnant patient, then foetal wellbeing should be monitored.
‘Understand the patient's comorbid condition(s) to tailor the management of critical illness.’
Remark 1:
Determine which chronic therapies should be continued and which therapies should be stopped temporarily. Monitor for drug-drug interactions. Use conservative fluid management in patients with SARI when there is no evidence of shock.
Remark:
Patients with SARI should be treated cautiously with intravenous fluids, because aggressive fluid resuscitation may worsen oxygenation, especially in settings where there is limited availability of mechanical ventilation. This applies for care of children and adults.
Admission to critical care units
Those patients that are in worsening respiratory failure will need to be admitted to the critical care unit. Matthay et al (2020) recognise that, before endotracheal intubation, it is important to consider a trial of high-flow nasal oxygen for patients with moderately severe hypoxaemia. This procedure might avoid the need for intubation and mechanical ventilation because it provides high concentrations of humidified oxygen, low levels of positive end-expiratory pressure, and can facilitate the elimination of carbon dioxide. WHO guidelines support the use of high-flow nasal oxygen in some patients, but they urge close monitoring for clinical deterioration that could result in the need for emergent intubations because such procedures might increase the risk of infection to health-care workers.
NICE Guideline: COVID-19 rapid guideline: critical care
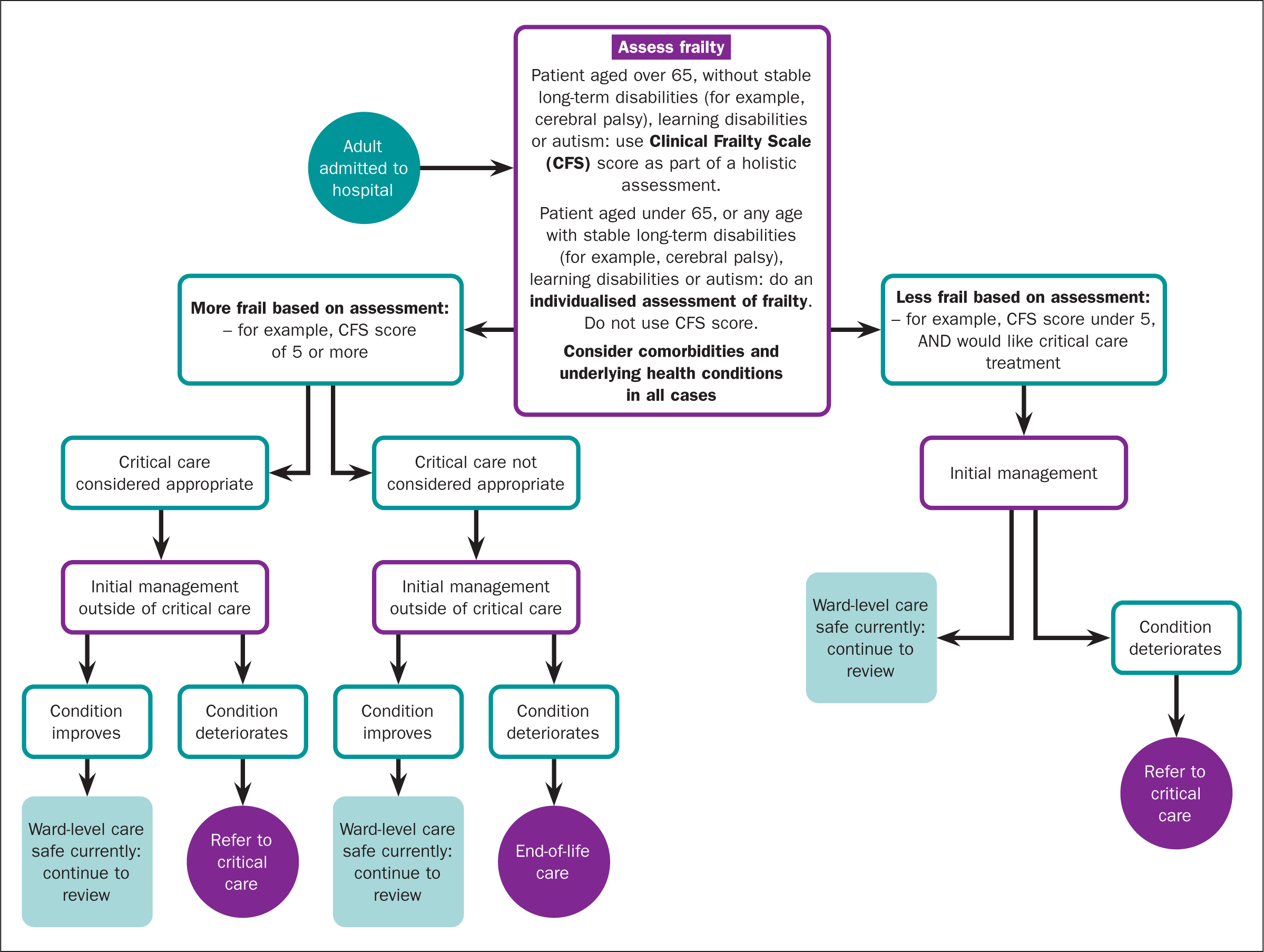
On 21 March 2020 official guidelines to help UK doctors and nurses know the best course of treatment for patients amid the coronavirus pandemic were published by the National Institute for Health and Care Excellence (NICE) (2020a; 2020b). It provides an algorithm to help doctors decide who should be admitted to critical care and who should not (NICE, 2020b). This guidance specifically focuses on the admission to hospital (NICE, 2020a), admission to critical care, starting, reviewing and stopping critical care treatment, clinical decision making and service organisation. It begins by asking clinicians to assess all adults for frailty, irrespective of age and COVID-19 status. Clinicians should consider comorbidities and underlying health conditions. The NICE guidance asks doctors to score patients aged 65+ without long-term stable disabilities on a nine-point Clinical Frailty Scale’ (CFS); those under 65 and with long-term stable disabilities should be assessed using an individualised assessment of frailty. The new guidelines stress that all patients admitted to hospital should still be assessed as usual for frailty ‘irrespective of COVID-19 status’ (NICE, 2020b). On the CFS, at one end of the scale, with a score of 1, are the ‘very fit’—people who are ‘robust, active, energetic and motivated’, and who ‘exercise regularly’. At the other end, with a score of 9, are the ‘terminally ill’. The NICE algorithm divides patients at a score of 5, the ‘mildly frail’. The COVID-19 rapid guideline can be seen in Figure 1.
Conclusion
It is important that, in these difficult times, nurses understand the symptoms of COVID-19, how to prevent its spread and are up-to-date on the guidance on critical care.

