The guideline Improving Supportive and Palliative Care For Adults With Cancer (National Institute for Health and Care Excellence (NICE), 2004) was produced with the aim of ensuring that people with cancer, along with their families and carers, were well informed, cared for and supported from before formal diagnosis and onward.
This guideline recommended that cancer clinical nurse specialists (CCNSs) should be trained to offer psychological assessment and intervention at an appropriate level (level 2) as part of their role. This training should include a taught component and ongoing clinical supervision from mental health specialists (usually clinical psychologists) to help the CCNSs develop and apply these skills. As a result, clinical psychologists working across the UK have developed training packages and established clinical supervision groups to support and guide CCNSs and other health professionals in the holistic care of their patients (Clark et al, 2015; Hession and Habenicht, 2020).
Clinical supervision in this context can help CCNSs and other health professionals to be better equipped to deal with the complex demands of working in cancer services (Mackereth et al, 2010). One aspect of clinical supervision is to facilitate a space where a CCNS can reflect on their engagement and relationship with a patient. Through paying attention to issues around the CCNS–patient interpersonal relationship, clinical supervision can help CCNSs address critical elements of their involvement in these supportive and therapeutic relationships with their patients (Hession and Habenicht, 2020).
With most patients, this can be relatively straightforward. However, there are always patients who challenge the CCNS's ability to maintain a supportive and therapeutic relationship. It is for clinical supervision of these ‘challenging’ relationships that the emotional boundary seesaw model was adapted from previous work (Hamilton, 2010) and developed further in 2015 (Lorentz, 2023).
Relationships with the patient
It is accepted within the psychological literature that people often establish ways of coping with the aim of moving themselves away from or lessening the intensity of strong or unbearable emotions (Pitceathly et al, 2011). Sometimes, these ways of coping are helpful and can contribute to a good relationship between the patient and the health professional. Other times, though, these ways of coping can be unhelpful and do not contribute to a good relationship.
Receiving a diagnosis of cancer and receiving treatment can be physically and psychologically onerous for cancer patients. If a patient feels worried and seeks to become more informed about their cancer and treatment, shares these fears and invests trust in the relationship with their CCNS and medical team, they are likely to experience better outcomes. If they feel worried, withdraw and avoid treatment or hospital appointments or are inconsistent or ambivalent about treatment plans and do not invest in the relationship with their medical team, they are less likely to experience good outcomes (Pitceathly et al, 2011).
Staff generally experience these latter patients as challenging because of the emotionality, disengagement or troubling interpersonal behaviours they display (Pitceathly et al, 2011). Patients who struggle to engage in supportive and therapeutic relationships with their CCNS experience greater cancer-related traumatic stress, lower emotional self-efficacy and less satisfaction with the support they receive, and tend to view these sources of support as aversive (Han et al, 2005).
Therefore, it is important to attend to these difficult relationships to ensure the patient gets as good an outcome as is possible. CCNSs also tend to bring challenging patients to clinical supervision because they are the patients with whom they are struggling to maintain a supportive and therapeutic relationship.
To help maintain a supportive and therapeutic relationship with challenging patients in a mental health setting, Hamilton (2010) built a generic boundary framework based on the work of Karpman (1968) and a document on professional boundaries in nursing produced in the USA (National Council of State Boards of Nursing, 1996). She developed this model using a quasi-grounded theory approach to help nurses make sense of everyday boundary activities to help with challenging patients.
This information was then conceptualised by Hamilton, using ideas from cognitive analytic therapy (Ryle and Kerr, 2002). The author has further adapted this model, again drawing on cognitive analytic therapy, to develop the emotional boundary seesaw model (Lorentz, 2023), to help understand what is happening in the supportive therapeutic relationship between CCNSs and cancer patients. This model has been used to support CCNSs in their clinical supervision with mainly clinical psychologists (Lalayiannis, 2019).
Managing the relationship with the patient
CCNSs are usually experienced nurses with a wide range of clinical and interpersonal skills, who have attended an advanced communication skills course before their level 2 psychological assessment and intervention skills training (NICE, 2004; Clark et al, 2015). These personal and professional qualities usually mean that CCNSs are generally compassionate, kind and competent practitioners who regularly go over and above to meet the care needs of their patients. This dynamic works well in the majority of their work. Patients experience helpful, compassionate and empathic support at a time when they most need it and are grateful. In return, CCNSs have anecdotally reported feeling job satisfaction in being able to provide this highly valued care and support.
However, with challenging patients, these same skills may still be met by anger, criticism and rejection from the patient (as described above). At this point, a CCNS is likely to experience a pull towards trying harder to meet the patients' needs and expectations in order to fix the relationship with the person. If this effort is met with further anger, criticism and rejection, the CCNS can experience being pushed away from the patient and may withdraw and hold the patient (understandably) at arm's length. This often increases the anger and criticism from the patient, who might say: ‘Why aren't you doing this for me any more? You used to!’ Often, the individual CCNS will share this experience with their colleagues, and this can lead to conflict or a split within the team between those who think the CCNS should offer more and those who feel that holding back is the more helpful strategy.
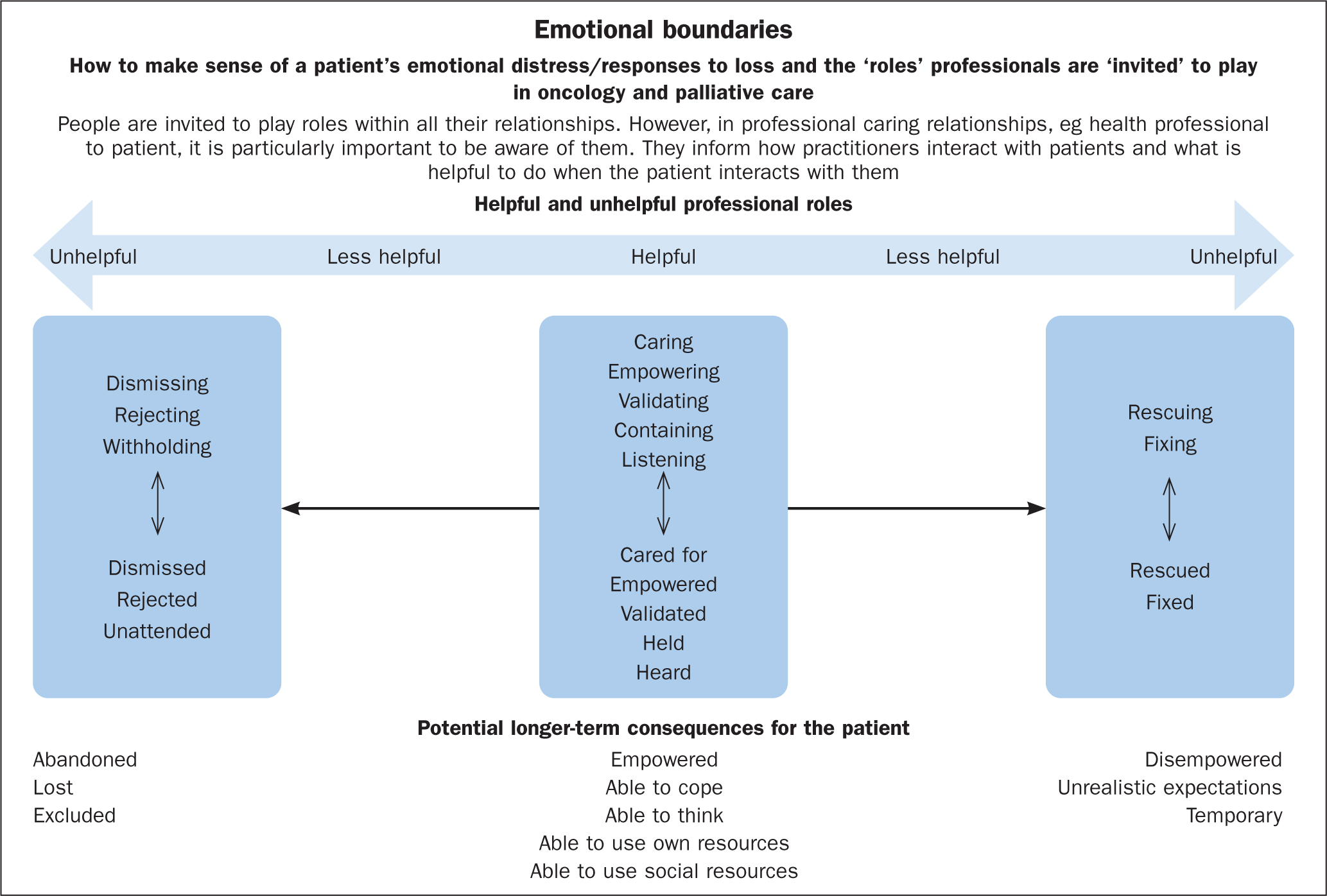
The emotional boundary seesaw model (Lorentz, 2023) (Figure 1) is a diagrammatic representation of this push-and-pull dynamic that is designed to help an individual CCNS or team in clinical supervision reflect on what is happening in this relationship and think about how to manage these emotional situations.
Emotional boundary seesaw model
In cognitive analytic therapy (Ryle and Kerr, 2002), we normalise and acknowledge that we are invited to play roles (the way we relate to others) within all our relationships, both personal and professional. However, in professional caring relationships – such as nurse to patient – the way in which we relate to the patient is important to acknowledge and to be aware of; this is because it helps us to understand what is happening in the relationship. If a rupture occurs within the relationship for any reason, this understanding can help practitioners understand how to repair this rupture in order to get the best outcomes they can for the patient (Figure 1).
At the centre or balance point of this adapted model are the helpful roles. The CCNS is caring, empowering, validating, containing and listens. In return, the patient feels cared for, empowered, validated, held and heard. The seesaw can start to tip in the relationship when the CCNS moves towards attempting to rescue or fix the patient, hoping that in return the patient will feel rescued or fixed. Moving towards rescuing or fixing can feel helpful initially, but there is always a point with challenging patients where there is a risk of the relationship inadvertently becoming disempowering, controlling or leading to unrealistic expectations. If the seesaw has tipped this far, the CCNS can experience a range of difficulties. The patient may demand extra care or the practitioner may find it hard to discharge the patient. The patient may express disappointment, frustration or anger because they perceive they are receiving lesser care or being rejected because their emotional needs are no longer being met. At this point, to repair the rupture in the relationship and to lead to the best possible outcome for the patient, it is important for the CCNS to notice and reflect on what has happened, either by themself or in clinical supervision. In this way, they can then notice that the seesaw has tipped too far, then negotiate and agree new boundaries with the patient to enable the CCNS to move back towards a more balanced position.
The seesaw can also start to tip the other way if the CCNS reacts to the patient's disappointment, frustration or anger with their own version of these feelings (‘I've given so much to them! Why are they turning on me?’). If this happens, the CCNS can risk moving past the balance point and towards dismissing, rejecting or withholding care and, in return, the patient is left feeling dismissed, rejected or not attended to. This can leave the patient feeling abandoned by the CCNS who was caring for them and disconnected from the wider system. This type of rupture has often been caused by the way the patient has related to the CCNS. However, to repair the rupture and lead to the best possible outcome for the patient, it is important for the CCNS to notice and reflect on what has happened (either by themself or in clinical supervision). Again, they can then notice that the seesaw has tipped too far, negotiate and agree new boundaries with the patient and move back towards a more balanced position.
Being in the in the balanced position enables the challenging patient to feel as empowered, able to cope, able to think, use their own resources and connect with social resources as is possible for them. Whereas, if the patient has felt rescued or fixed by the CCNS, this can have the unwanted side effects of being a temporary state, disempowering their self-efficacy towards engaging with their care and leaving them with unrealistic expectations of what others can do for them moving forwards. If the rescuing or fixing has not been experienced as helpful or has led to a rupture and the CCNS has unintentionally become dismissing, withholding and rejecting, the patient can be left feeling abandoned, lost or excluded from care.
This model enables us to recognise that this unintended consequence has occurred, not as a result of a lack of care from the CCNS but rather their desire to rescue or fix the relationship and their genuine attempt to repair it and create a positive outcome for the patient. The model allows practitioners to recognise that the most helpful approach is to notice what has happened in the relationship and to negotiate more appropriate boundaries, both emotionally and practically.
Conclusion
Clinical supervision is important in enabling and allowing the CCNS to maintain a supportive and therapeutic relationship with challenging patients. The emotional boundary seesaw model provides a useful tool to reflect on this CCNS–patient relationship, to identify when things are starting to tip into becoming unhelpful and to tip them back to being helpful again.
Rather than the CCNS trying harder and harder to fix the relationship by letting go of boundaries and tipping matters further, re-establishing boundaries allows the relationship to tip back towards a more helpful and balanced place without tipping too far and becoming unhelpful in a different way. In this more balanced position, the patient can feel appropriately supported and experience the best outcomes possible.
KEY POINTS
- Patients who struggle to engage in supportive and therapeutic relationships with their cancer clinical nurse specialist experience greater cancer-related traumatic stress, lower emotional self-efficacy and less satisfaction with the support they receive
- Looking after challenging patients often leads to disagreements or divisions within teams about the best way to care for them
- Working harder to meet the demands of challenging patients rarely results in repairing the relationship or improving their outcomes. Noticing what has happened and re-establishing boundaries allows the relationship to tip back towards a more helpful and balanced place
- Repairing ruptures in the relationship allows the patient to feel appropriately supported and experience the best outcomes possible
CPD reflective questions
- Can you think of a patient that you struggled to form a good relationship with or who you found ‘challenging’?
- Reflect on what happened when you have cared for a challenging patient. Did you find yourself responding to them in a different way to how you normally would? Was this helpful? If not, do you recognise yourself being pulled into crossing the emotional boundaries described in the article? Do you think re-establishing some boundaries within the relationship could have helped?
- When you have worked with patients who have ‘challenged’ you emotionally in the past, what has helped you to maintain a helpful relationship with them?


