Congenital heart disease (CHD), or congenital heart defects as the conditions are often described, affects 1% of live births each year, equivalent to up to 9 in every 1000 babies born in the UK (Knowles and Hunter, 2014). A recent study by Nisselrooj et al (2020) identified that CHD is frequently missed during prenatal screening, and this can impact on morbidity and mortality. In their study, over half of the diagnosed CHD cases were not detected prior to birth. Sometimes evidence of poor circulation is apparent during the newborn examination or later in the first few months of life. This includes mottling of the skin, blueish tinge around the lips, clubbing of the fingers and poor weight gain (Hinton and Ware, 2017).
Children who are diagnosed with a congenital heart defect may require several surgical procedures, numerous hospital admissions and many years of medication. On the other hand, however, some families may have little need for medical or nursing input. Many children with CHD will live with complications related to their condition, including learning difficulties (NHS website, 2018a). Sadly, the mortality rate for children with CHD is high, accounting for 12% of all child deaths (Knowles and Hunter, 2014).
CHD can be described as defects of the cardiac architecture that impact on blood flow and perfusion (Thiene and Frescura, 2010). Thiene and Frescura (2010) attempted to divide anomalies into five classifications, but they can also be more simply divided into acyanotic/non-cyanotic and cyanotic (Ghandi, 2016; Crawford, 2020) (Table 1).
| Classification | Description | Conditions | Cyanotic? |
|---|---|---|---|
| 1 | Increased pulmonary blood flow (septal defects without pulmonary obstruction and with left to right shunt) |
|
Acyanotic |
| 2 | Decreased pulmonary flow (septal defects with pulmonary obstruction and with right to left shunt) |
|
Cyanotic |
| 3 | Obstruction to blood flow and no septal defect (no shunt) |
|
Acyanotic |
| 4 | So severe as to be incompatible with postnatal blood circulation |
|
Cyanotic |
| 5 | Silent until adulthood |
|
Acyanotic |
Causes
The 20-week antenatal scan is the primary point at which the structures of the heart are examined. The heart is one of the first organs to be formed in utero. By 8 weeks' gestation, the heart's atria and ventricles are formed, and all major vessels are developed (Bhattacharya and Stubblefield, 2016). Often women are unaware they are pregnant in these initial weeks. Most causes of CHD remain unknown. However, exposure to certain pathogens within the first weeks of gestation is a known factor. For instance, infection with the rubella virus, also known as German measles, during pregnancy increases the risk of the foetus developing CHD. The risk of heart defects is higher if the mother has diabetes before pregnancy, or is diagnosed with diabetes in the first trimester. However, gestational diabetes is not a major risk factor (NHS website, 2018a). Phenylketonuria is a rare, inherited metabolic disorder that it affects how the mother processes a protein called phenylalanine, which is found in many foods. If the condition is unstable this can also cause CHD (NHS website, 2018a). Taking some medicines in the first trimester such as anti-epileptic medication, angiotensin-converting enzyme (ACE) inhibitors for high blood pressure and retinoic acids for acne treatment have all been identified as causes of CHD (National Heart, Lung and Blood Institute, 2020).
Findings from Sheridan et al's (2013) study of anomalies reported by the British Isles Network of Congenital Anomaly Registers confirmed that the offspring of consanguineous unions (eg between first cousins) have an increased risk of congenital anomalies. Within their study the risk of CHD was doubled in children who were conceived in a consanguineous union (Sheridan et al, 2013).
Poor socioeconomic background has been associated with increased risk of all congenital anomalies (Vrijheid et al, 2000). A few researchers have suggested that socioeconomic disadvantage and reduced access to diagnostic services result in an increased prevalence of CHD in certain population groups (Sadiq et al, 1995; Sheridan et al, 2013). A study by Knowles et al (2017)—the Born in Bradford study, involving 5350 infants born with CHD—identified an increased prevalence of CHD in black and Asian ethnic groups, particularly those of south Asian origin.
Normal heart function
An average adult has around 5 litres of blood, which is continuously pumped through the body by the heart. In neonates and children, the blood volume is calculated in mililitres per kilogram of body weight (ml/kg) (Howie, 2011).
The younger the child the more intravascular volume (blood) they have. Neonates and infants have more circulatory intravascular volume, they need more blood to meet their cardiovascular needs. The blood volume in older children is nearly the same as that in adults.
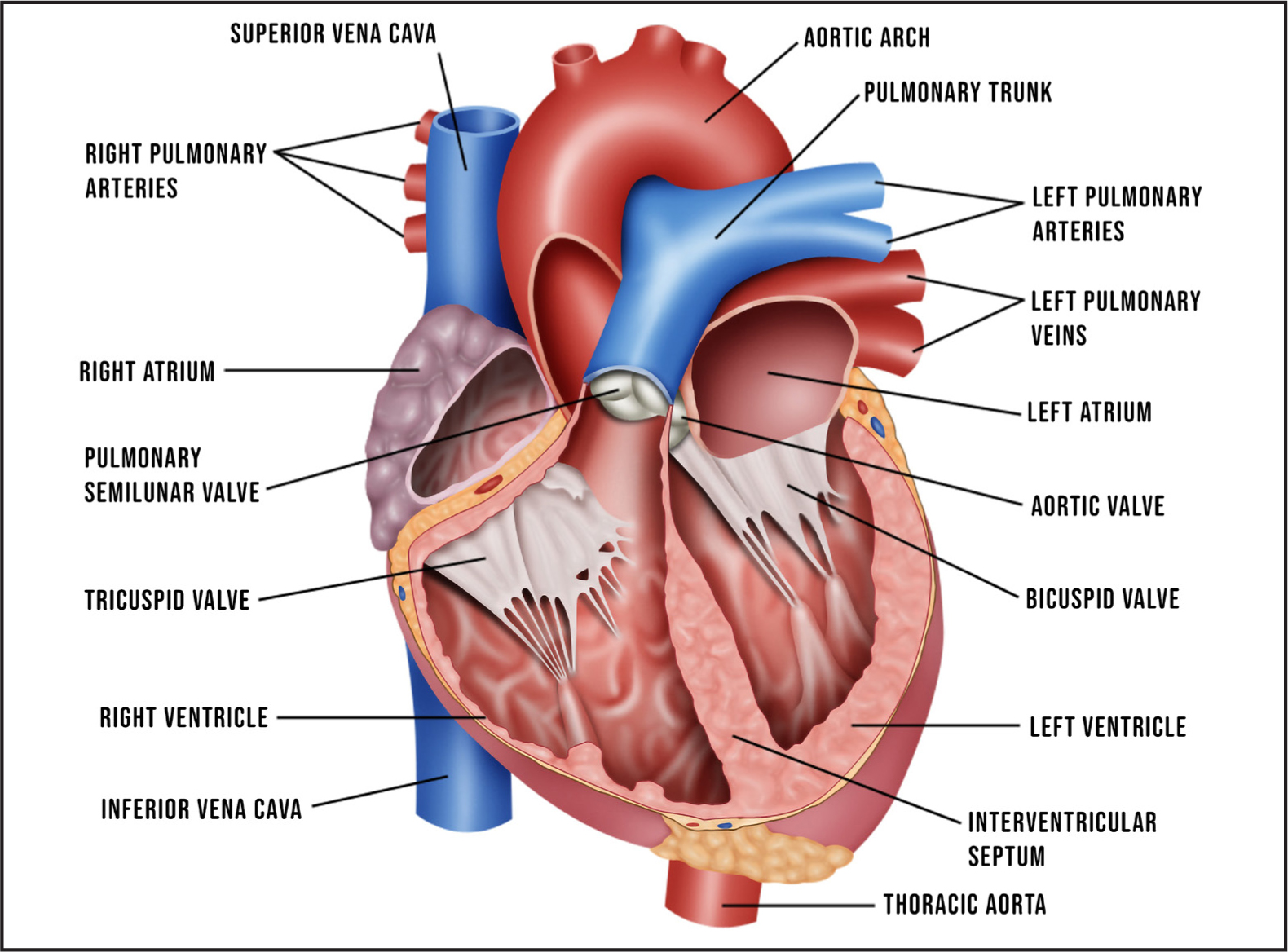
The right atrium (Figure 1) receives deoxygenated blood from the superior and inferior vena cava; it then contracts, the tricuspid valve opens and the blood flows into the right ventricle. Once the right ventricle is filled with blood, it then contracts, the blood goes to the pulmonary artery and through into the lungs to be oxygenated when gaseous exchange occurs. Once oxygenated, the blood returns to the heart via the pulmonary vein and into the left atrium. The left atrium contracts, the bicuspid valve opens and the blood flows into the left ventricle. Once filled it contracts, the aortic valve opens and blood is pumped to the aorta and then around the body. After oxygenated blood is used it returns to the heart and the cycle starts again.
Foetal circulation
The mother's placenta acts as the baby's lungs until the baby is born. The placenta takes in deoxygenated blood from the umbilical arteries; it is oxygenated from the mother's blood and then returned to the umbilical veins (Figure 2). The oxygenated blood moves through a shunt called the ductus venosus. Some of the blood goes to the liver, but it predominantly flows through the inferior vena cava and into the right atrium of the heart. Most of the blood flows across the left atrium via a shunt called the foraman ovale. From the left atrium, blood flows down to the left ventricle and is then pumped into the ascending aorta, which sends it to the brain, heart muscle and lower body. The deoxygenated blood, containing carbon dioxide and waste products, returns to the right atrium. From here, it bypasses the foetus's lungs and flows through the ductus arteriosus into the descending aorta and then returns to the placenta through the umbilical arteries.
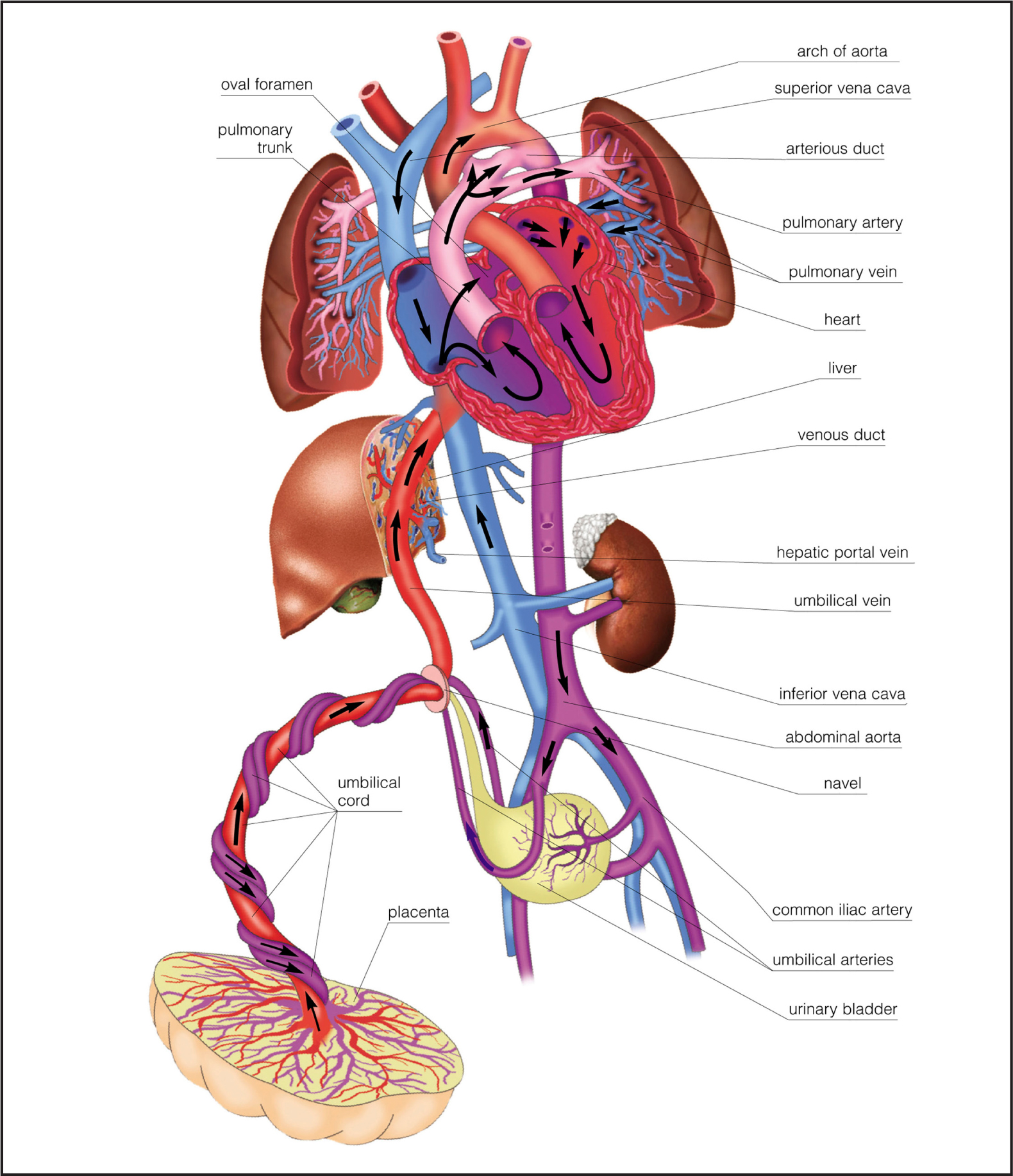
When the baby is born, the lungs start to function. As the umbilical cord is clamped the fetal circulation from the mother is stopped, the baby's lungs expand and the ductus arteriosus and foramen ovale begin to close. Now the baby's cardiopulmonary function commences.
Cardiac anomalies
Patent ductus arteriosus
Patent ductus arteriosus (PDA) is when a hole is left open after a baby is born. It means that the blood that was bypassing the circulation to the lungs in the womb is still doing this. This hole usually closes within a couple of days; depending on the size of the hole a PDA may not be picked up straight away. Indomethacin, ibuprofen and, more recently, paracetamol are used to medically close the PDA (MacLaren and Heuchan, 2017). If this is not successful or there is urgency then a surgical repair will be performed by catheterisation or a small metal clip around the hole, keeping it closed (American Heart Association, 2020).
Atrial and ventricular septal defect
Some children are born with a ‘hole in the heart’. The medical term for this is a septal defect. Most commonly there is a hole between the walls of the atrium chambers (atrial septal defect (ASD)) or ventricle chambers (ventricular septal defect (VSD)) (Great Ormond Street Hospital for Children, 2013; NHS website, 2018c; Royal Brompton and Harefield NHS Foundation Trust, 2021). These can close spontaneously or, in some cases, will require surgical repair (Mayo Clinic, 2019).
Pulmonary atresia
Pulmonary atresia with a VSD is a serious type of congenital heart condition (British Heart Foundation, 2016). There are two main abnormalities involved: the valve that allows blood to flow from the heart to the lungs, the pulmonary valve, is blocked and the baby also has a VSD. In utero the blood passes from the aorta to the pulmonary artery through the ductus arteriosus. For a baby with pulmonary atresia and a VSD to survive, the duct must stay open after birth. Some babies with severe forms of pulmonary atresia with a VSD will have a more complex abnormality; their pulmonary arteries are extremely underdeveloped and have multiple abnormal blood vessels (British Heart Foundation (BHF), 2016).
Transposition of the great arteries
Transposition of the great arteries occurs during foetal development in the first 8 weeks of pregnancy. It is when the pulmonary artery comes from the left ventricle instead of the right and the aorta originates from the right. The baby will require operation called arterial switch, where the pulmonary artery and aorta are switched into the correct ventricles (BHF, 2016; Children's Heart Federation, 2020).
Ebstein's anomaly
In this condition, the tricuspid valve (between the right atrium and right ventricle) is in the wrong position and the valve's flaps are the incorrect shape (Cincinnati Children's Hospital Medical Center, 2021). As a result, the valve does not function properly. Ebstein's anomaly can result in enlargement of the right atrium, and heart failure. The result is less deoxygenated blood getting into the lungs. Often there is also an atrial septal defect present, meaning there is mixing of oxygenated and deoxygenated blood as well as the ventricle being weak. Open-heart surgery is required to fix or replace the valve and repair the ASD (Cincinnati Children's Hospital Medical Center, 2021; National Institute for Health and Care Excellence (NICE), 2017)
Tetralogy of Fallot
This is the term used for a group of four defects together: VSD, overriding aorta, right ventricular hypertrophy and pulmonary valve stenosis. Eventually surgery is needed, usually with a stent and then further surgery to close the VSD and an attempt to normalise blood flow (Apitz et al, 2009; NHS website, 2018b)
Transplant and ventricular assist devices
Surgery to repair the defect is not always successful or an option for some children and a heart transplant may be the preferred treatment. While awaiting transplant children can be in hospital or at home depending on how well they are. Sometimes children may need to be on a device to support their heart called a ventricular assist device (VAD) such as a Berlin Heart or Heart Wave (Children's Heart Federation, 2020). These devices are used when the patient's heart becomes too weak to pump itself. They can be inserted into one side of the heart (usually the left ventricle, an LVAD) or both (BIVAD). The device consists of one or more chambers that sit outside the heart and blood is pumped by a driving unit, which is attached to the child (Great Ormond Street Hospital, 2020).

