The nervous system is an incredibly complex system of cells, tissues and organs that plays a vital role in the control and regulation of all bodily functions. When the nervous system is disrupted, it can lead to a variety of disorders which can impact on a person's quality of life.
Nervous system disorders, also known as neurological disorders, refer to a broad range of conditions that can affect various parts of the nervous system, including the brain, spinal cord and nerves. The incidence of these disorders can vary greatly depending on the specific condition and geographical location. According to the World Health Organization ((WHO), 2023a), neurological disorders are a major public health problem affecting millions of people worldwide. Moreover, neurological disorders are one of the leading causes of disability worldwide (Feigin et al, 2019). In the UK, neurological disorders are a common and significant health problem. Approximately one in six people living in England have one or more neurological disorders (Neurological Alliance, 2019), and neurological disorders were two of the top five leading causes of death in England and Wales (Office for National Statistics 2023) (Table 1).
Table 1. Leading causes of death in England and Wales, 2022
| Causes of death | n | % |
|---|---|---|
| Dementia and Alzheimer's disease | 65 967 | 11.4 |
| Ischaemic heart diseases | 59 356 | 10.3 |
| Chronic lower respiratory diseases | 29 815 | 5.2 |
| Cerebrovascular diseases | 29 274 | 5.1 |
| Malignant neoplasm of trachea, bronchus and lung | 28 571 | 5.0 |
The nervous system: an overview
The nervous system is a complex network of specialised cells called neurons, which transmit electrical and chemical signals throughout the body to communicate with and control other cells. It is divided into two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS) (Figure 1).

Neurons
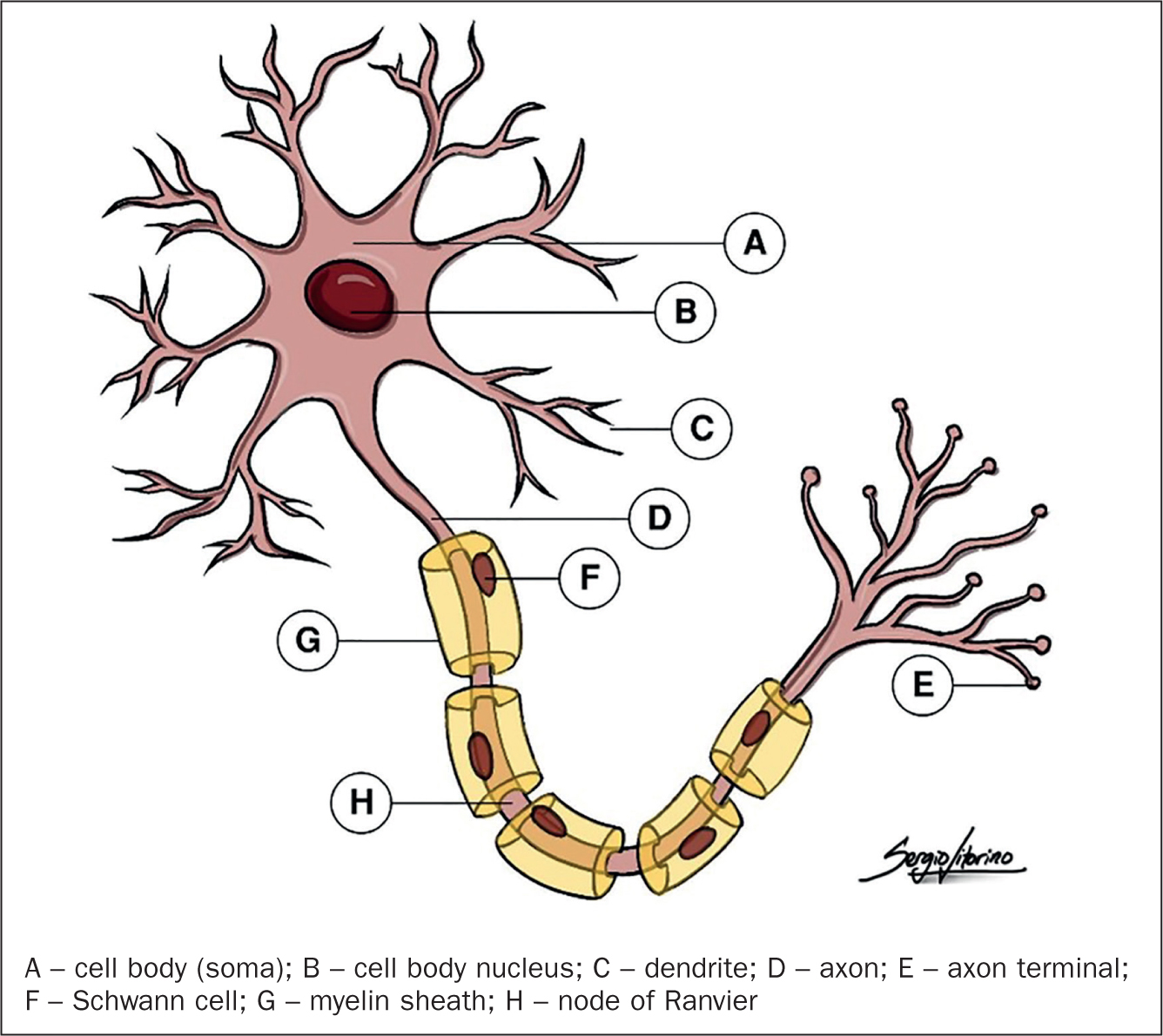
Neurons, also known as nerve cells, are the primary functional unit of the nervous system and are responsible for transmitting electrical and chemical signals throughout the body. The structure of a neuron consists of a cell body, dendrites, and an axon (Figure 2). The cell body contains the nucleus and other organelles that are responsible for the cell's metabolism. Dendrites are branched extensions that receive signals from other neurons or sensory cells. Axons are long, slender extensions of the cell body that transmit signals to other neurons or to muscles or glands.
Although the neurons are the cells responsible for transmitting information throughout the nervous system, glial cells play important roles in supporting and protecting neurons, and in maintaining the chemical environment of the nervous system. There are several types of glial cells, each of which has a specific set of functions and characteristics (Table 2). Their dysfunction has been implicated in a variety of neurological and psychiatric disorders (Kim et al, 2020; Martins-Macedo et al, 2021).
Table 2. Types, location, and major functions of glial cells
| Glial cell | Location | Major functions |
|---|---|---|
| Astrocytes | Central nervous system | Provide structural and metabolic support; participate in repair |
| Ependymal cells | Central nervous system, line central canal, and ventricles | Assist in the production and movement of cerebrospinal fluid |
| Microglia | Central nervous system | Participate in defence and immune responses |
| Oligodendrocytes | Central nervous system | Produce myelin and provide electrical insulation |
| Satellite cells | Peripheral nervous system, peripheral ganglia | Provide structural and metabolic support for cell bodies of neurons |
| Schwann cells | Peripheral nervous system, peripheral nerves | Produce myelin and provide electrical insulation |
Central nervous system
The CNS is made up of the brain and spinal cord and is responsible for receiving and interpreting information from the PNS and sending out appropriate signals to control bodily functions. It is protected by three layers of membranes, known as meninges, and is bathed in cerebrospinal fluid (CSF), which provides cushioning and support.
The brain is the control centre of the nervous system and is responsible for receiving, processing and transmitting sensory information from the body. It is protected by the skull and its structure comprises three main parts: the cerebrum, cerebellum, and brainstem. The cerebrum is the largest part of the brain and is responsible for conscious thought, movement, sensation, and perception. The cerebellum is involved in coordination, balance and muscle control, while the brainstem controls basic life functions such as breathing, heart rate and blood pressure (Waugh and Grant, 2022). In addition to its many functions, the brain has also a property called neuroplasticity, meaning it can change and adapt in response to new experiences and learning. Indeed, neuroplasticity is what allows the acquisition of new skills, recovery from injuries, and adaptation to changing environments throughout the lifespan (de Oliveira, 2020).
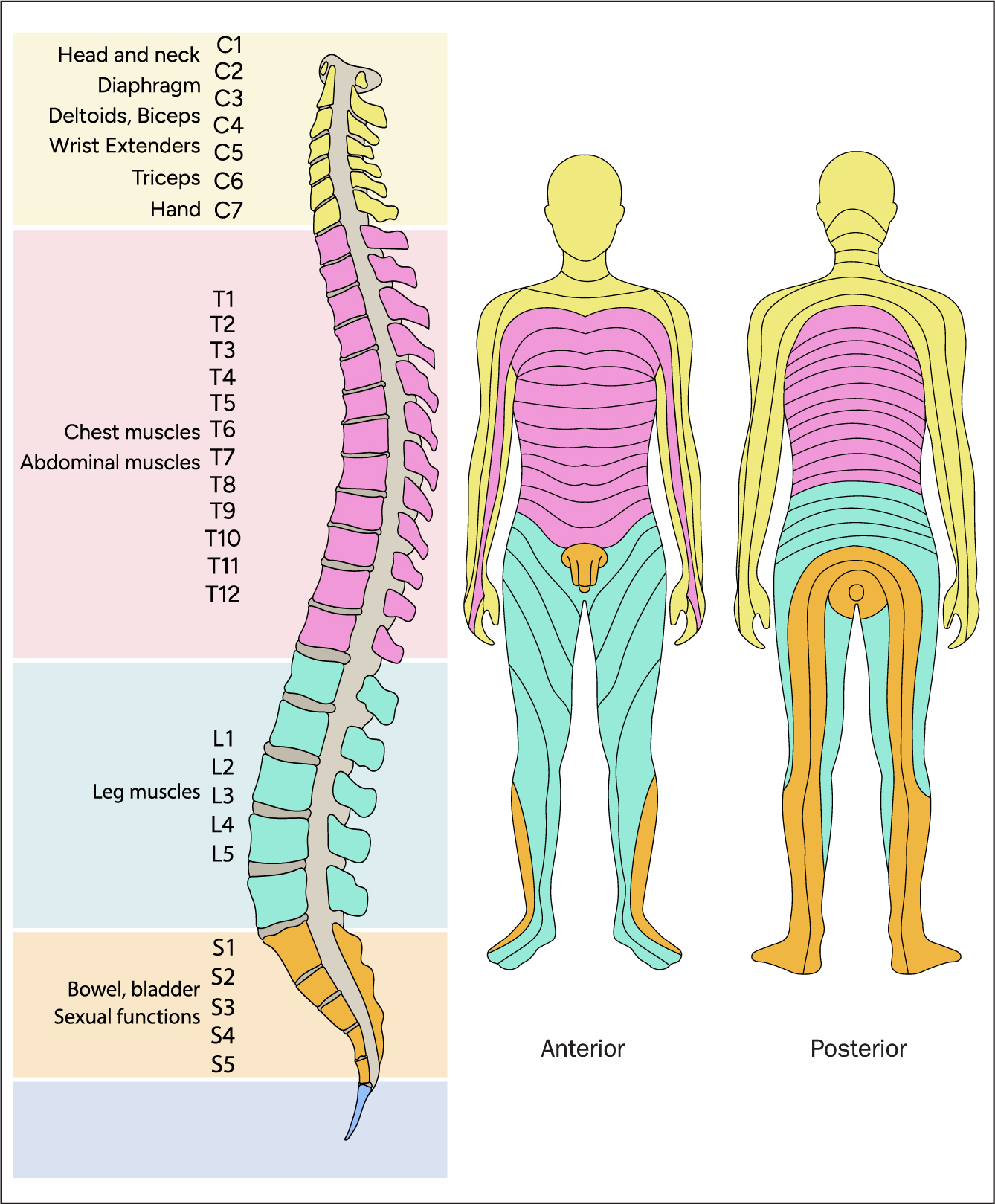
The spinal cord is a long, cylindrical bundle of nerve fibres that extends from the brainstem to the lower back. It acts as a pathway for signals travelling between the brain and the rest of the body and it is protected by the vertebrae of the spine. Different regions of the spinal cord correspond to specific zones of the body, allowing for precise control and coordination of movement and sensation. If a specific segment of the spinal cord is injured, it results in a corresponding loss of function or sensation in the specific area of the body that is served by that particular region of the spinal cord (Figure 3).
Peripheral nervous system
The PNS consists of all the nerves outside the CNS. These nerves are divided into two types: sensory nerves, which carry information from the sensory organs (such as the eyes and ears) to the CNS, and motor nerves, which carry signals from the CNS to the muscles and organs, causing them to move or perform their functions. Furthermore, the PNS is divided into two parts: the somatic nervous system and the autonomic nervous system. The somatic nervous system controls voluntary movements and sensory perception, while the autonomic nervous system controls many of the body's automatic functions, such as heart rate, digestion and respiration. The autonomic nervous system is further divided into the sympathetic and parasympathetic systems, which work together to maintain balance and regulate the body's response to different stimuli (Figure 1).
Assessment of the nervous system
Assessing the nervous system can be a complex process and can involve a range of tests and evaluations, depending on the specific concerns or symptoms that are present. For a comprehensive assessment of the structure, function, and ability of the nervous system to respond to stimuli, a multitude of methods is considered; the most common are as follows:
- Medical history: collecting data about previous medical conditions or injuries, any relevant family history, and current symptoms can help identify potential and/or active nervous system issues
- Physical examination: at a physical level, this should comprise an ABCDE assessment (Resuscitation Council UK, 2021), with a focus on cranial nerve examination, motor examination, sensory examination, and reflex examination (National Institute for Health and Care Excellence (NICE), 2023). An understanding of the sensory nerve connections from different areas of the skin through the spinal cord (Figure 3) can help identify a spinal cord injury
- Mental status examination: this involves evaluating a person's cognitive abilities, including memory, orientation, attention, language, and executive function. When assessing the patient's consciousness level, tools such as ACVPU (Table 3) and the Glasgow Coma Scale (https://www.glasgowcomascale.org/) should be considered
- Imaging tests: tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can provide images of the brain, spinal cord and nerves. These tests can help detect abnormalities, such as tumours, lesions or inflammation
- Electrophysiological tests: electroencephalogram (EEG) and electromyogram (EMG) are examples of tests that can measure the electrical activity of the nervous system. These tests are used to diagnose a variety of neuromuscular diseases, nerve injuries and nervous degenerative conditions
- Nerve conduction studies: these tests measure the speed and strength of nerve impulses. They can help diagnose conditions such as carpal tunnel syndrome, peripheral neuropathy, or nerve injuries
- Laboratory tests: blood and CSF tests can be used to detect certain neurological conditions, such as infections, autoimmune diseases or vitamin deficiencies.
Table 3. ACVPU assessment of level of consciousness, used in the National Early Warning Score 2
| A | Alert | The patient is awake |
| C | Acute Confusion | New onset of confusion, disorientation, delirium, or any new alteration to mentation |
| V | Voice | The patient requires a verbal stimulus to initiate a response |
| P | Pain | The patient requires a pain stimulus to initiate a response |
| U | Unresponsive | Unresponsive to all stimuli |
Disorders of the nervous system
Neurological disorders can be broadly classified into several categories based on their underlying causes, symptoms, and affected areas of the nervous system. The major categories of neurological disorder are listed and briefly described in Table 4; some examples of neurological disorder are also included for each category. The list demonstrates the range of possible disorders that can affect the nervous system is, all of them with great potential to affect a person's quality of life.
Table 4. Main categories of neurological disorders
| Category | Description | Examples |
|---|---|---|
| Structural | Affecting the structure of the brain or other parts of the nervous system | Tumours, aneurysms, malformations |
| Degenerative | Involving the progressive loss of nerve cells or other components of the nervous system | Alzheimer's disease, Parkinson's disease, Huntington's disease |
| Vascular | Affecting the blood vessels in the brain or other parts of the nervous system | Stroke, cerebral haemorrhage |
| Infectious | Caused by infections in the nervous system | Meningitis, encephalitis |
| Traumatic | Resulting from physical injuries to the brain or other parts of the nervous system | Concussion, spinal cord injury |
| Functional | Involving changes in the way the nervous system functions, without any apparent structural or biochemical abnormalities | Epilepsy, migraine, multiple sclerosis |
| Developmental | Arising during the development of the nervous system | Cerebral palsy, autism spectrum disorders, intellectual disability |
| Autoimmune | Resulting from an abnormal immune response that attacks the nervous system | Multiple sclerosis, myasthenia gravis |
| Metabolic | Affecting the metabolism of the nervous system | Tay-Sachs disease, phenylketonuria |
The five largest contributors to global neurological disability-adjusted life-years (DALYs: a measure of overall disease burden, expressed as the number of years lost as a result of ill-health, disability, or premature death) are stroke, migraine, Alzheimer's disease, meningitis and epilepsy (Feigin et al, 2019).
Stroke
A stroke is caused by interrupted blood supply to the brain – a blockage in a blood vessel (ischaemic stroke) or a ruptured vessel (haemorrhagic stroke). Risk factors for stroke include hypertension, smoking, diabetes, hypercholesterolaemia, atrial fibrillation, obesity, sedentariness, family history of stroke, age, sex and race (Saver and Hankey, 2020).
Signs and symptoms are sudden paraesthesia and/or paresis on one side of the body, dysarthria or aphasia, vision impairment in one or both eyes, confusion, dizziness, vertigo and severe headache. Diagnostic tests and investigations include brain imaging tests (CT or MRI scan), carotid ultrasound and angiogram.
Treatment for stroke involves (NICE, 2022a):
- Intravenous thrombolysis with alteplase within the first 4.5 hours of stroke symptoms for confirmed ischaemic stroke
- Thrombectomy if the patient meets the required criteria
- Anticoagulation with aspirin
- Statins (only if already receiving such treatment for other comorbidities) for ischaemic strokes
- Focus on haemostasis and reducing blood and intracranial pressures for haemorrhagic strokes.
Preventive measures involve managing underlying health conditions (eg, hypertension, diabetes), smoking cessation, regular physical exercise, maintaining a healthy weight, limiting alcohol consumption, and early detection and treatment of stroke symptoms (Bavikatte et al, 2021).
Migraine
The exact cause of migraine is not fully understood but might be related to changes in the levels of certain chemicals in the brain, including serotonin (Kilinc et al, 2017).
Triggers include hormonal changes (eg, oestrogen, progesterone), stress, changes in sleep patterns, and certain foods such as alcohol, aspartame sweetener, beans and other tyramine-containing foods, caffeine, cheeses and yoghurt, soups and foods containing monosodium glutamate, or processed meats containing sulphites (Silva-Néto et al, 2021).
Signs and symptoms vary from person to person but typically include a throbbing or pulsating headache, sensitivity to light and sound, nausea and vomiting, and auras (Weatherall, 2015; Digre, 2019).
Diagnosis comprises a thorough medical history and physical examination to rule out other possible causes of headaches. Brain imaging tests (MRI or CT scans) may be used for differential diagnosis, and the International Classification of Headache Disorders (ICHD) criteria (Headache Classification Committee of the International Headache Society, 2018).
Treatments for migraine include analgesics (eg, paracetamol and non-steroidal anti-inflammatory drugs), triptans and anti-emetics to manage the symptoms. Prophylactic medication (beta blockers or antidepressants) may also be prescribed (NICE, 2021). Patients will be advised on lifestyle changes (adequate sleep, stress reduction, healthy diet, trigger identification/avoidance, relaxation techniques) and other potential preventive measures include cognitive behavioural therapy and biofeedback, acupuncture (Urits et al, 2020; Bae et al, 2021; Ingvalsden et al, 2021).
Early diagnosis and prompt management of migraine is essential to avoid complications, such as status migrainosus or even stroke (Øie et al, 2020).
Alzheimer's disease
The most common type of dementia, Alzheimer's disease, involves a build-up of amyloid plaques and tau tangles in the brain (DeTure and Dickson, 2019). The exact causes are not fully understood but genetic, environmental and lifestyle factors may be involved (Dunn et al, 2019). Risk factors include age, family history, head injuries, hypertension, hypercholesterolaemia and diabetes (Litke et al, 2021).
Signs and symptoms are memory loss and confusion (this may be mild in the early stages), cognitive impairment (language difficulties, disorientation) and mood and behaviour changes. As the disease progresses, people with Alzheimer's disease will have difficulty with basic activities of daily living (eg, eating, bathing, dressing) (Pedroso et al, 2018).
Diagnosis involves a thorough medical history and cognitive function tests (Mini-Mental State Examination, Montreal Cognitive Assessment) (Wang et al, 2022), brain imaging tests (MRI or CT scans) and potentially positron emission tomography scans to detect abnormal protein deposits in the brain (Maschio and Ni, 2022) Treatment for Alzheimer's disease involves medications to manage memory loss and cognitive symptoms (eg, cholinesterase inhibitors), non-pharmacological interventions such as occupational therapy and speech therapy, and lifestyle modifications promoting physical exercise, healthy eating and social engagement (NICE, 2018; Bennett et al, 2019; Bhatti et al, 2020).
There is no cure yet available but clinical trials of drugs targeting amyloid plaques and tau tangles (Awasthi et al, 2022) and lifestyle interventions such as cognitive training and physical exercise (Kang et al, 2019; Liu et al, 2022) have shown promising early results to slow or stop the progression of the disease.
Meningitis
Bacterial meningitis (the most common form) is caused by bacteria such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae (in particular, type b or Hib) (Tsang, 2021; UK Health Security Agency, 2022); they can be spread through respiratory secretions, such as coughing and sneezing, or through direct contact with an infected person (WHO, 2023b).
Viral meningitis is caused by viruses including enteroviruses, herpes simplex virus and varicella zoster virus (Tavakolian et al, 2021); the responsible virus is usually spread through contact with contaminated faecal matter or respiratory secretions, or can be transmitted through insect bites (WHO, 2023b).
Symptoms of meningitis are fever, headache, stiff neck, nausea, vomiting, photophobia, confusion and seizures. Signs in infants and young children also include lethargy, poor feeding and irritability. In severe cases there may be seizures, loss of consciousness or coma (Lucas et al, 2014).
Investigations include a physical examination, blood tests (full blood count, C-reactive protein, procalcitonin, blood cultures), and a lumbar puncture for CSF analysis. Imaging studies may also be used.
Management of bacterial meningitis is immediate hospitalisation and treatment with intravenous antibiotics. Viral meningitis usually resolves on its own with supportive care. Supportive care for both types may include intravenous fluids, oxygen therapy, and medication for fever, seizures and pain (NICE, 2015). Prevention is through vaccination and good hygiene practices (Parikh et al, 2020; WHO, 2023b).
Epilepsy
Although epilepsy can affect people of all ages, races, and backgrounds, it is most commonly diagnosed in childhood or in people over the age of 65 years. Some people may only have one seizure in their lifetime, while others may experience multiple seizures a day (NHS, 2020).
Causes are not always clear, but can include brain injury, genetic factors, infections, tumours and other medical conditions. In some cases, it may be idiopathic (Şafak et al, 2020)
Seizures can be triggered by a variety of factors, including stress, lack of sleep, flashing lights (National Institute of Neurological Disorders and Stroke, 2023), and certain medications, such as antidepressants, diphenhydramine, tramadol and isoniazid (Chen et al, 2016). There may be sudden and temporary changes in behaviour, movement, sensation or emotion. A person with epilepsy may have convulsions and loss of consciousness, or there may be brief periods of staring, confusion or muscle jerking.
Investigations include an EEG, MRI and blood tests such as full blood count, urea and electrolytes, liver function tests, glucose and calcium (NICE, 2022b) to identify conditions that may be triggering the seizures (such as infections, iron deficiency, anaemia or diabetes).
One form of treatment is anti-seizure medications (eg, levetiracetam), which can help control the frequency and severity of seizures (NICE, 2022b). In some cases, surgery may be recommended to remove part of the brain responsible for the seizures. Other interventions include dietary changes such as a ketogenic diet, and lifestyle modifications to reduce seizure triggers (NICE, 2022b). Close collaboration between the patient and healthcare providers is key, to develop a personalised treatment plan (WHO, 2022).
Conclusion
Understanding the nervous system enables nurses to perform accurate assessments, identify early signs of neurological dysfunction, and intervene promptly. It empowers them to recognise potential complications, manage symptoms effectively, and provide appropriate support to patients and their families. Neurological conditions, such as stroke, can have profound effects on individuals' physical, cognitive and emotional wellbeing. By developing a comprehensive understanding of the nervous system and associated disorders, nurses can provide competent and compassionate care, tailored to each patient's unique needs. The second part of this discussion will build on this to consider patient assessment in more detail and emphasise the importance of facilitating patient self-management for improved outcomes.
KEY POINTS
- The nervous system plays an important role in coordinating bodily functions and responses, maintaining homeostasis and transmitting signals throughout the body
- Disorders of the nervous system, such as stroke, migraine, Alzheimer's disease, meningitis and epilepsy, can significantly impact on a person's quality of life and functionality
- Timely and comprehensive assessment of individuals with neurological disorders is essential to detect changes in symptoms, functional abilities and cognitive status, allowing for early intervention and improved outcomes
- Without prompt and accurate assessment, individuals with neurological disorder may experience delays in receiving appropriate care, leading to increased risk of complications and diminished quality of life
- Nurses must possess a comprehensive understanding of neurological disorders, their classifications, symptoms, treatment options and interventions to deliver effective, patient-centred care and support to individuals and their families
CPD reflective questions
- How is the nervous system and associated disorders assessed in your clinical area?
- How can you collaborate with other health professionals to ensure a comprehensive assessment of individuals with neurological disorders, considering the diverse range of symptoms and presentations associated with these conditions?
- How can you advocate for the integration of nursing assessment as a cornerstone in your clinical team's approach to managing individuals with neurological disorders, recognising its pivotal role in providing comprehensive and patient-centred care?


