Nurses have a vital role to play in mobile radiography as they provide care to patients before, during and after the diagnostic imaging examination. In recent years, the scope of practice of nurses in the UK and the Republic of Ireland has expanded to allow nurse consultants and advanced nurse practitioners to assess and refer patients for limited radiological examinations (Royal College of Nursing et al, 2008; Nursing and Midwifery Board of Ireland, 2020). This requires an understanding of imaging examinations.
Mobile radiography refers to the imaging of patients outside the radiology department using mobile X-ray equipment. These imaging examinations are commonly called ‘portable X-rays’ because of the early small portable X-ray units that were designed to be dismantled and assembled at the patient's location or bedside. Unfortunately, these portable X-ray units had a low power output, produced high radiation doses to the patients and produced poor-quality images. For these reasons, portable X-ray machines are no longer in use in medicine. However, the term ‘portable X-ray’ has persisted among health professionals and is often used in reference to mobile radiography.
Most hospitals are equipped with mobile X-ray units, which can be wheeled to the patient's bedside where transferring patient to the radiology department threatens to compromise their care. In other words, mobile radiography should be restricted to only those patients whose medical condition is such that it is impossible for them to be moved to the radiology department without seriously affecting their treatment and nursing care (Whitley et al, 2016). Such patients are commonly found in special care units such as intensive care units (ICUs), coronary care units, cardiac surgery units, special care baby units, accident and emergency department resuscitation units and post-anaesthesia care units (theatre recovery rooms). Mobile radiography is also carried out on unstable patients in hospital wards or other hospital locations, but these should be limited due to radiation protection restrictions. The walls of the special care units are mostly lead-lined or made of concrete to shield ionising radiation in a similar way to radiology departments, whereas general wards are not designed to this specification (Hart et al, 2002).
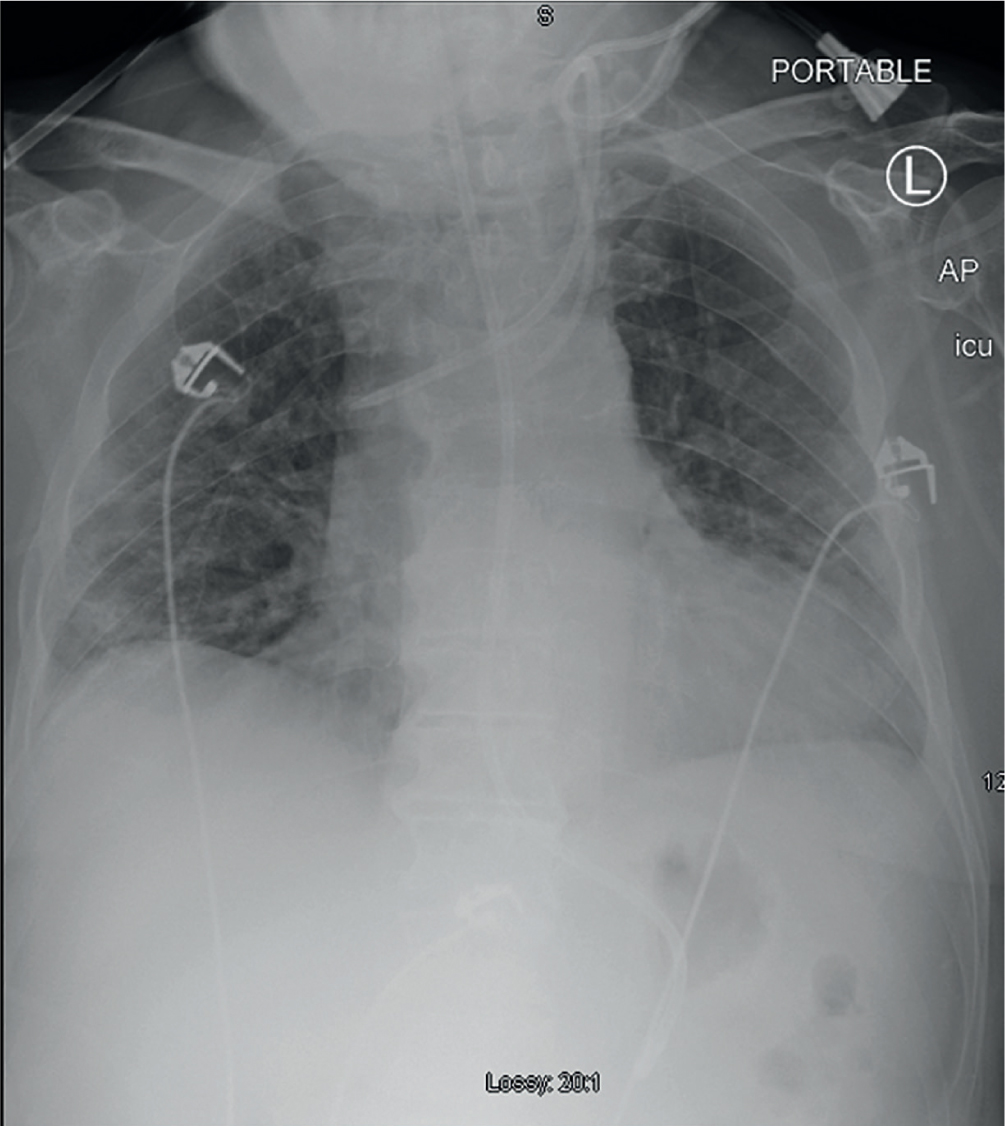
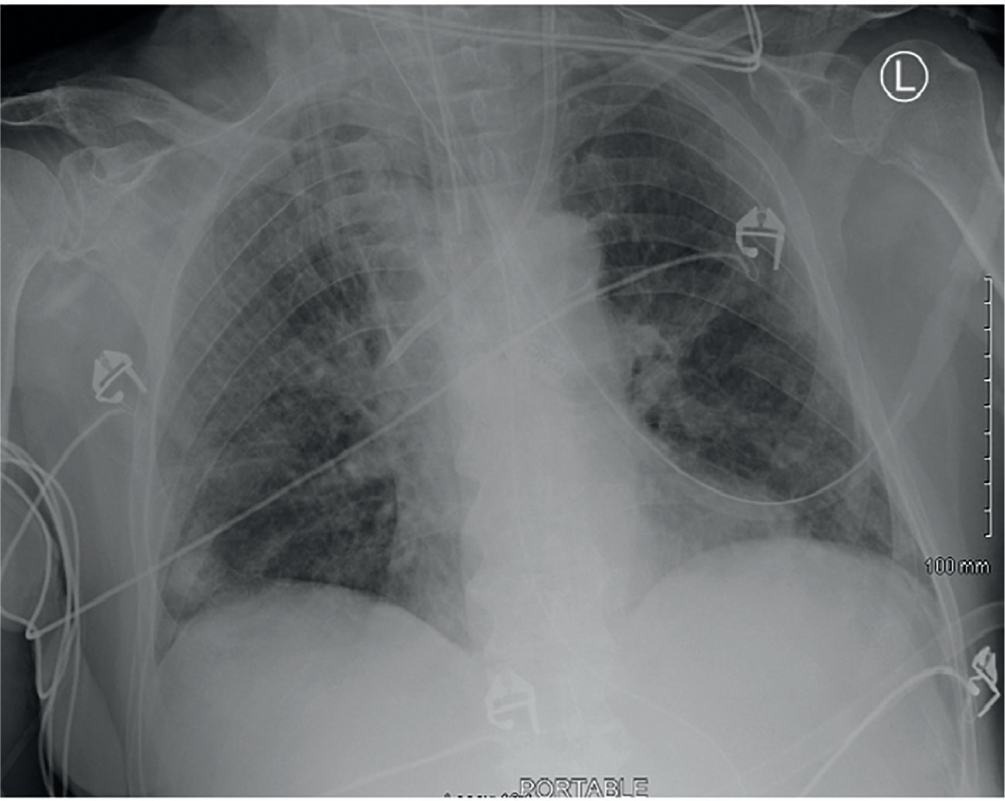
In the hospital setting, a common examination performed using a mobile X-ray unit is the chest X-ray. Other radiological examinations can also be performed, but the limitations of the mobile X-ray unit, such as low-quality images and radiation protection, should be taken into consideration. The most common indications for performing a portable X-ray are to check for positions of tracheostomies, nasogastric tubes (NGs), central lines or central venous catheters (CVCs), trauma injuries, pacemakers and other medical conditions of patients who require special care. Figure 1 and Figure 2 show portable X-ray radiographs (images).
Three health professionals are involved in mobile radiography: referring medical doctors, radiographers and nurses. The referring doctor or other professional will discusses what is required with the patient, if possible, and makes a request for a portable X-ray to the radiology department. The radiographer and nurse(s) communicate, position and immobilise the patient in order to perform an imaging examination. Radiographers are taught how to perform this role and educational literature is available from their perspective. However, there is scarcity of educational literature for nurses on this subject. This article provides information and aims to raise awareness among nurses at a time when the number of portable chest X-rays has increased globally, due to the current coronavirus pandemic. All critically ill COVID-19 patients require periodical portable chest X-rays to assess the severity and progression of any chest infection (Kooraki et al, 2020). Owing to the infection control measures for COVID-19 patients with chest infections, most of these patients are being X-rayed using mobile X-ray equipment on the wards or other locations.
Mobile X-ray equipment
Mobile X-ray equipment has a higher power output than the discarded portable X-ray equipment in order to perform various radiological examinations, is heavy and needs to be motorised to facilitate being pushed between locations (Griffiths and Holmes, 2009). Modern mobile X-ray machines use a high-powered rechargeable battery to generate the electrical power for X-ray exposure. This unit only requires access to a 13 amp power supply for battery recharging during storage (Whitley et al, 2016). Mobile X-ray equipment varies in design depending on the manufacturer and the intended use, with most units having extendible tube support and adjustable height to provide a good range of movement (Griffiths and Holmes, 2009). This makes it possible for the radiographer to adjust the focus-film distance or source-image distance and angulations of the X-ray beam. They are also a compact size to allow easy movement within small spaces, such as between patients' beds and in hospital cubicles.
Modern mobile X-ray equipment falls broadly into two types: analogue and digital, the broad distinction between the two being the difference in how the image is captured and processed. Analogue technology allows the taking of X-ray exposures on a computed radiography (CR) plate, which is then scanned with the CR reader away from the patient's bedside to produce a digital image. Digital radiography (DR) mobile X-ray units use a digital detector to produce an instant image following exposure. The image is available for viewing at the patient's bedside. In both methods, the final image can be printed or stored digitally on the picture archiving and communication system (PACS). A detailed discussion on the design, operationalisation of the mobile X-ray equipment and how the radiological examinations are performed are outside the scope of this article.
Justification of mobile radiography examinations
In the UK, the request and undertaking of portable X-rays should be in accordance with the Ionising Radiation (Medical Exposure) Regulations of 2017 (legislation.gov.uk, 2017). These regulations deal with the safe and effective use of ionising radiation in medicine. Mobile radiography uses X-radiation, which is harmful to the human body (International Commission on Radiation Protection, 2007; Ehrlich and Coakes, 2017). Therefore, all portable X-ray examinations should be justified. This means that the benefits to the patient undergoing an X-ray examination should outweigh the risks from ionising radiation (International Commission on Radiation Protection, 2007).
Therefore the referring doctor should state on the X-ray request form the clinical indication for the X-ray and why a mobile X-ray is the best option in the management of the patient. This responsibility is shared between the referring doctor and the radiographer involved in the X-ray examination. However, in mobile radiography, justification goes beyond the justification principle. Portable X-rays should be restricted to patients on life-support machines, or those with medical conditions where nursing care and treatment could be seriously affected if transported to the radiology department. Shortage of ward staff to bring the patient to the radiology department is not a justified reason for performing a portable X-ray. If the examination requested could be done in the radiology department with a better outcome, the radiographer should consult the referring doctor and nurse looking after the patient regarding the advisability of moving the patient (Ehrlich and Coakes, 2017). In other words, the referring doctor should always consent to any changes to the portable X-ray request.
Working relationships: referring medical doctor, radiographer and nurse
A good working relationship between the health professionals—referring doctor, radiographer and nurse—involved in mobile radiography is cardinal in acquiring quality diagnostic images. The referring doctor should make an X-ray request electronically through the radiology information system (RIS) or write a paper request for the portable X-ray. This should be communicated to the radiology department or in urgent cases by telephone, bleep system or sending of a completed paper X-ray request form. The radiographer should build a rapport with the nurses on arrival on the ward or unit and ask the nurse looking after the patient about the patient's condition (Ehrlich and Coakes, 2017). The radiographer should not move or disturb the patient before first asking the nurse about the patient's medical condition (Whitley et al, 2016). This is because the nurse responsible for the patient knows the condition and patient's needs. Nurses and supporting staff should also assist the radiographer in communicating with the patient and in positioning the X-ray plate or detector by lifting the patient.
At the end of the imaging examination, the nurse or referring doctor should be informed about when the X-ray is likely to be available on the PACS system or in hard copies. It should be stressed that a written X-ray request should be made before the imaging examination as the radiographer will need the created electronic request to undertake the exposure for digital radiography and process the CR plate for the analogue imaging system. Sometimes clinicians ask for an imaging examination before a written request is made due to a lack of understanding of the process.
Infection control during mobile radiography
The control of infection plays an important role in the management of all patients, especially those in special care units (Jones and Taylor, 2006; World Health Organization, 2020). During mobile radiography, the nurse looking after the patient has a responsibility to communicate any infection control measures to the radiographer and ensure that all control measures are adhered to, to prevent the spread of infection (Whitley et al, 2016). The mobile X-ray equipment, CR plate or digital detector and lead aprons are surfaces from which infection can spread. Thus, the nurse should ensure that the established local protocols on infection control are adhered to by all staff encountering the patient.
The mobile X-ray equipment used in special care units should ideally be dedicated units and kept on site (Whitley et al, 2016). Failing this, the mobile X-ray equipment should be cleaned with antiseptic solution before being wheeled into infection-controlled areas such as ICU (Whitley et al, 2016; Ehrlich and Coakes, 2017). All staff should adhere to the ‘Five moments of hand hygiene’ issued by the World Health Organization (2020). This infection control measure defines the key moments when health professionals, such as nurses and radiographers should perform hand hygiene: before touching a patient, before cleaning/aseptic procedures, after body fluid exposure/risk, after touching a patient and after touching a patient's surroundings. During mobile radiography, it is advisable to cover the CR plate or digital detector with a suitable cover such as a plastic to prevent contamination from body fluids. When dealing with patients with a known, highly contagious infection, such as COVID-19 or methicillin-resistant Staphylococcus aureus (MRSA), all clinical staff should wear appropriate personal protective equipment (PPE) (Whitley et al, 2016; Kooraki et al, 2020). After the imaging examination, all PPE should be taken off carefully and placed in the correct waste bins. Mobile X-ray equipment and lead aprons should also be cleaned with antiseptic solution.
Radiation protection during mobile radiography
Nurses' understanding and adherence to radiation protection control measures during mobile radiography is of paramount importance in protecting patients, themselves and members of the public visiting the ward/unit. However, some research studies have found limited awareness and non-adherence to radiation protection control measures among nurses during mobile radiography (Anim-Sampong et al, 2015; Luntsi et al, 2016; Azimi et al, 2018). This can be attributed to a lack of radiation protection awareness programmes for nurses working in clinical settings where ionising radiation is used, such as ICU and hospital wards. There are three practical methods of controlling the external radiation exposure during mobile radiography: time, distance and shielding.
Time
Minimising the exposure time of an individual reduces the dose from the radiation source (Whitley et al, 2016; Martin et al, 2019). In the context of this article, the radiation source is the X-ray tube of the mobile equipment. The control measure of time does not generally apply to mobile radiography. If there is a need for a nurse to stay with the patient during the exposure, a lead apron should be provided and rotation of nurses for patients requiring periodical mobile X-ray examinations should be in place. Rotation reduces the amount of exposure to each nurse (Jones and Taylor, 2006). However, nurses are rarely required to stay with the patient during the X-ray exposure in mobile radiography.
Distance
The dose of radiation decreases dramatically as the distance is increased from the source (Whitley et al, 2016; Martin et al, 2019). This is commonly called the inverse square law. Therefore, nurses and supporting staff should stand as far as possible from the X-ray mobile equipment and outside the radiation field when the radiographer is making an exposure (Whitley et al, 2016). Mobile patients not on a life support system and members of the public should stand at a safe distance during the X-ray exposure. The recommended minimal safe distance is 2 metres, at which scattered radiation is attenuated equivalent to background levels (Chiang et al, 2015).
Patients within 2 metres of the radiation field should be provided with shielding such as lead aprons, especially paediatric patients, who are most vulnerable to ionising radiation due to a higher sensitivity of the developing organs and tissue (International Commission on Radiation Protection, 2013). It should be noted that radiographers and nurses have a responsibility to ensure that no one is within the radiation field during the X-ray exposure of the patient. This is achieved by informing all persons in the immediate area that an X-ray exposure is about to be made and asking them to stand a safe distance from the radiation field area.
Shielding
Placing a barrier of lead or concrete between the radiation source and an individual provides protection from X-radiation (Jones and Taylor, 2006; Ehrlich and Coakes, 2017). During mobile radiography, anyone assisting in an examination and staying in the radiation field should wear a lead-rubber apron or stand behind a mobile lead screen. Generally, walls in special care units where ionising radiation is used are designed to contain the radiation produced by the mobile X-ray tube within a set of criteria and limits determined by relevant legislation (Hart et al, 2002).
Conclusion
It is highly recommended that mobile radiography is restricted to patients whose conditions make it difficult to be transported to the radiology department. Most radiological examinations should be performed in the radiology department where stationary high-powered X-ray equipment is used that produces high-quality images. The department is also designed to contain the radiation produced by the X-ray tube (Hart et al, 2002). It should be stressed that mobile radiography requires adequate knowledge on this topic by the health professionals involved in the radiological examinations. This should be acquired during undergraduate training and supplemented with continuous professional development (CPD) learning activities to keep health professionals updated with knowledge and skills.

