Nurses represent the largest proportion of health professionals (Haddad et al, 2020). Regulatory bodies influence nurse education, set standards and seek to advance the profession, while striving to ensure care is well-informed, person-centred and compassionate (American Nurses Association, 2015; Willis, 2015; Nursing and Midwifery Board of Australia (NMBA), 2018; Nursing and Midwifery Council (NMC), 2018a). Wong et al's (2015) analysis of World Health Organization documents identified nursing education as a global concern and acknowledged that better postregistration continuing professional development (CPD) education enables nurses to question care, provide quality care and develop extended skills.
Since 1995, CPD has been mandatory for UK nurses (Beaumont and Stainton, 2016). Governments, employers and regulators expect nurses to keep themselves up to date (Willis, 2015; NMC, 2017; NMBA, 2018). ‘Revalidation’ requires nurses to undertake a minimum of 35 hours of CPD relevant to their scope of practice over 3 years to maintain registration (NMC, 2019). Internationally, numerous activities are available (Hughes and Quinn, 2013; Bungeroth et al, 2018). Local identification of activities is encouraged, with precise requirements varying (Wong et al, 2015; NMBA, 2016; NMC, 2017).
A dichotomy exists between expectation and practice. Nurses struggle to complete CPD in the face of workforce pressures (Keogh, 2014; Bungeroth et al, 2018; Glasper, 2018). Some identify expectations from managers to use personal time for CPD (Jones-Berry, 2016). Schweitzer and Krassa's (2010) integrative review identified the most frequent deterrents as cost, time and personal responsibility. Although CPD is an individual's responsibility, employers often influence accessibility (Bungeroth et al, 2018). Although there are often no legal requirements for employers to facilitate CPD (Beaumont and Stainton, 2016; NMC, 2019), many UK hospitals recognise governance and CPD are inextricably linked (Wood, 2006).
Deeper comprehension of factors influencing CPD engagement may enable educators to advocate and facilitate postregistration CPD more effectively (Frankel, 2009; Hughes and Quinn, 2013; Jones et al, 2015).
To increase understanding, a systematic review was undertaken and formed part of an MA in Practice Education. The review question was: ‘What factors influence hospital-based nurses’ engagement with CPD activities in the UK?' Obtaining ethical approval was not considered necessary for this type of review.
Methods
The Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines informed processes (Liberati et al, 2009).
The Population, Exposure and Outcomes (PEO) framework informed research question formulation and search terminology (Bettany-Saltikov and McSherry, 2016). Predefined database terminology, consideration of synonyms, abbreviations, truncation and Boolean operators enhanced searches. Four groups of terms were used, adjusted to fit individual databases:
Librarians advocated use of country and study type within searches. Published and grey literature were searched via EBSCO Discovery Service and the British Nursing Index in November 2018 and the British Library EThOS database in January 2019. Google Scholar facilitated citation chaining and retrieval of full texts. Manual searching of reference lists of included studies occurred. A comparative CINAHL search was requested via the Royal College of Nursing.
Primary UK-based research considering attitudes, beliefs, opinions, views, perceptions, perspectives, experiences or engagement of hospital-based nurses with CPD was included. As UK CPD requirements were introduced in 1995 (Beaumont and Stainton, 2016), the timeframe was January 1995 to November 2018. Studies were excluded if the profession or workplace was unclear, nurses were not the respondents, or data were inseparable from non-nurses or non-hospital-based nurses in the study.
Searches yielded 769 articles (209 duplicates were automatically removed by EBSCO). Manual cross-checking excluded 141 additional duplicates; 419 articles were evaluated against the inclusion criteria by title then abstract and 76 full texts reviewed. Five returns required confirmation of participant workplaces. Clarification was sought from some authors, resulting in one inclusion and four exclusions. Five further returns related to one study. Two published articles and a thesis were retained. Two conference papers were unobtainable. Five studies were finally identified for review (in eight articles and one thesis) (Figure 1).

A condensed version of the ‘Reader's guide to the Literature on Interventions Addressing the Need for education and Training’ (ReLIANT) and the ‘Mixed Methods Appraisal Tool’ (MMAT) (Koufogiannakis et al, 2005; Hong et al, 2018) were combined into a standardised, piloted form used to critique the studies. No studies were excluded at this stage.
Bibliographic information, research questions, aims, population, sample recruitment and demographics, data collection and analysis, results or themes were recorded (Table 1).
| Study | Aims | Study design | Setting and population | Sample and data collection | Themes/findings | Strengths/limitations |
|---|---|---|---|---|---|---|
| Bahn (2007a) (2007b) | To gain information on the current orientation of registered nurses towards continuing education and lifelong learning |
Qualitative empirical | Not stated [author contacted] Hospital based, England |
Randomly selected candidates |
|
|
| Balls (2010) | To explore the perceptions of band 5 nurses and the factors that affect their development and ability to change posts in a large acute Trust | Interpretive/hermeneutic phenomenology | Large acute Trust, England |
Non-random purposive |
|
|
| Gould et al (2007)/Drey et al (2009) | To explore qualified nurses' experiences of continuing professional development (CPD); to explore the relationship between CPD undertaken by nurses in standard and extended roles and their levels of professional and organisational commitment | Qualitative, descriptive and quantitative | Three contrasting, acute NHS Trusts in London, England |
Random |
|
|
| Hogston (1995) | To understand what impact nurses perceived [CPD] to have on the quality of nursing care | Qualitative, grounded theory | Large hospital; south of England |
Opportunistic 18 individuals Unstructured interviews |
|
|
| Tame (2009) (2011) (2012 | Exploring and describing perioperative nurses' lived experiences of continuing professional education and reasons for non-participation | Descriptive qualitative framework | Large teaching NHS Trust; north of England |
Non-probability, purposive |
|
|
Narrative synthesis enabled elucidation of themes and formulation of areas for future investigation (Centre for Reviews and Dissemination, 2009). Qualitative, diagrammatical and tabulated data were reviewed. Congruency between findings was considered. Original data were retained to enhance synthesis. Tabulating textual data enabled open coding and higher-order heading formation, facilitating preliminary synthesis through an iterative, inductive process. As themes evolved, interrogation facilitated exploration of relationships.
Explicit, reproducible, comprehensive strategies were followed. Since the review was conducted as part of a Master's pathway, predominantly independent processes were required which could introduce bias, subjectivity and decrease credibility (Bettany-Saltikov and McSherry, 2016) so mitigating strategies were implemented. The protocol, including piloted quality appraisal and data extraction forms, was approved by the University Systematic Review Board. Academic librarians endorsed searches and an independent search provided comparison (Cooke et al, 2012). An experienced supervisor advised on processes and conducted independent appraisal and extraction of one study for comparison (Cooke et al, 2012).
Findings
All except Tame's (2009) doctoral thesis were published. All produced qualitative data. In the largest study reviewed, which produced two reports, Gould et al (2007) and Drey et al (2009) employed a questionnaire distributed across several hospitals. Remaining studies used face-to-face techniques (interviews and/or focus groups) within one hospital. The quality appraisal revealed that only Bahn (2007a, 2007b) had a clear research question and only Tame (2009) provided a clear explanation of method. None described their population in detail.
Most recruited a cross-section of nurses, although Tame (2009) focused on perioperative nurses. Balls (2010) recruited ‘newly qualified’ nurses; however, participants may have been qualified for up to 3 years and the gender ratio (3 male: 3 female) seems unrepresentative of the workforce. Another study produced two publications: one exploring interview data (Bahn, 2007a), and the other, focus groups (Bahn, 2007b). It was unclear whether any participants contributed to both. Further information may be found within Table 1.
Forty-two findings were aggregated into 35 categories then synthesised into four over-arching themes: individual resources, nurses' professional motivation, organisational commitment to learning and development and managerial support. Consideration of GRADE-CERQual facilitated confidence in the synthesised findings (Lewin et al, 2018).
Individual resources
Funding influenced engagement. Some nurses were unsure how CPD was funded (Balls, 2010). Many expressed anger at being expected to source grants, or self-fund, and considered this a barrier (Bahn, 2007a; Tame, 2009; Balls, 2010). Some recognised managers and organisations were limited by financial constraints (Hogston, 1995).
Nurses criticised expectations of using personal time, including holidays, particularly when CPD was primarily to enhance service delivery (Bahn, 2007a; Gould et al, 2007; Tame, 2009; Balls, 2010). Personal time included travel, attending activities, completing assignments and co-ordinating childcare (Gould et al, 2007; Tame, 2009). Compromises regarding time and funding were made, including negotiating shift patterns (Tame, 2009; Balls, 2010). Time and funding had the largest impact on work–life balance (Gould et al, 2007; Tame, 2009). Family support often made the difference between accessing, completing or withdrawing from CPD (Bahn, 2007b; Tame, 2009). Guilt was expressed as nurses and their families made sacrifices and redefined roles (Tame, 2009). Others rejected such personal sacrifices arguing they already worked in underpaid, severely stretched systems with few guarantees of promotion or financial gain from CPD (Bahn, 2007a; Tame, 2009).
All studies found that CPD affected self-confidence and self-worth. Three studies identified appraisals and personal development plans (PDPs) as supporting engagement (Bahn, 2007a; Tame, 2009; Balls, 2010). In all studies, participants discussed the importance of individualised CPD. This applied to content, mode of delivery and the potential to impact patient care (Hogston, 1995; Bahn, 2007b; Gould et al, 2007; Balls, 2010). Facilitating identification of activities, enabling congruence between individuals' resources, practice requirements and patient benefits, appraisals and PDPs also acted as a monitor regarding CPD uptake and parity (Bahn, 2007b; Tame, 2009; Balls, 2010). Although lack of appraisal or PDPs were noted in areas where engagement was low, some nurses sought CPD to gain feedback (Tame, 2009).
Some nurses worried they were falling behind due to changes in nurse education (Bahn, 2007a). Previous experiences of school, pre-registration or postregistration courses dissuaded some from higher education courses (Gould et al, 2007; Tame, 2009). University staff attitudes were influential on continued engagement (Bahn, 2007b; Tame, 2009).
Professional motivation
Participants in all studies were motivated to access CPD, identifying that it consolidated, maintained and updated skills, enabling professional progression and status, impacted competence and enhanced care (Hogston, 1995; Bahn, 2007a; Gould et al, 2007; Tame, 2009). The tenet of high-quality care is intrinsic to nursing professionalism (Bahn, 2007b). Hogston (1995) considered the relationship between CPD and care, identifying that learning must occur, not simply attending activities. Although increased knowledge can improve standards (Bahn, 2007a; Tame, 2009), this may not follow when CPD is solely to fulfil registrational statutes. Some were motivated by CPD facilitating the evolution of extended roles (Bahn, 2007a; Gould et al, 2007; Tame, 2009). Nurses considered CPD facilitated legitimate questioning of care, enabling them to improve practice (Hogston, 1995; Bahn, 2007b; Tame, 2009).
Organisational commitment to learning and development
Some organisations influence CPD by making it mandatory. Some nurses believed this ensured nurse and patient safety, although others considered it merely organisational protection (Bahn, 2007b; Gould et al, 2007). Organisational aspects such as low staffing led to CPD omission, the implications of which were not fully appreciated (Bahn, 2007b; Drey et al, 2009).
Nurses working in organisations where CPD was not valued expressed reduced confidence, increased anxiety, secret study and horizontal violence (Balls, 2010; Tame, 2011; 2012). Horizontal violence, as discussed by Tame (2012), refers to negative behaviours such as devaluing, harming or showing disrespect among colleagues, often those of a similar grade, with the aim of influencing or controlling others. Where learning and development was embedded, with staff enabled to disseminate learning and implement changes, care standards and working relationships appeared enhanced (Hogston, 1995; Bahn, 2007a; Gould et al, 2007; Tame, 2009).
Nurses stated that staffing levels affected non-mandatory CPD more, with organisations unable to free staff to attend (Bahn, 2007a; Gould et al, 2007; Tame, 2009). Reduced funding to back-fill staff or pay for CPD was identified (Bahn, 2007a; Gould et al, 2007; Tame, 2009; Balls, 2010). Transferable skills were highlighted as potentially encouraging organisations to support non-mandatory CPD (Bahn, 2007b).
Increased awareness of CPD influenced engagement, although resentment ensued if it was inaccessible (Gould et al, 2007; Balls, 2010). There was disparity within and across organisations (Bahn, 2007a; Gould et al, 2007; Tame, 2009; Balls, 2010). In another article Tame (2011) identified managers sabotaging nurses' attempts to study through ‘fixing’ rotas or restricting study time. Part-time working, shift patterns, career stage and age were discussed as potentially preventing CPD (Bahn, 2007b; Gould et al, 2007; Tame, 2009). Seeing nurses ‘earmarked’ for progression and being offered more CPD, or conversely refusing to engage, were highlighted as unfair (Hogston, 1995; Tame, 2009; 2012). Nurses believed staff retention was facilitated by organisations encouraging CPD, while the converse was also true (Gould et al, 2007; Drey et al, 2009; Tame, 2009; Balls, 2010).
Managerial support
Although organisations influence CPD, managers were described as pivotal in influencing the ‘cultural milieu’ (Tame, 2012). The value managers placed on CPD dictated how much and what was accessed by individuals (Hogston, 1995; Bahn, 2007a, 2007b; Gould et al, 2007; Tame, 2009). Managers who engaged with CPD, fostering positive environments for learning, dissemination of knowledge and reviewing practice, were viewed as good managers (Bahn, 2007a; Gould et al, 2007; Tame, 2009). Nurses receiving managerial support felt encouraged and valued as a professional, perceiving managerial confidence in their abilities (Hogston, 1995; Tame, 2009). Others identified managers as feeling threatened or jealous of junior nurses accessing CPD (Gould et al, 2007; Tame, 2009).
Nurses understood staffing levels and funding were often beyond managerial control (Tame, 2009). Some believed that if CPD relevance was apparent, managers were more likely to support funding and staff release (Hogston, 1995; Bahn, 2007a). Implicit, and explicit, was the potential for using CPD as a reward or sanction, to motivate or enhance performance (Hogston, 1995; Gould et al, 2007; Drey et al, 2009).
Lack of managerial engagement caused frustration (Hogston, 1995; Gould et al, 2007; Tame, 2009; Balls, 2010). Nurses remained determined to develop in the face of managerial resistance and might avoid approaching these managers or disclosing their CPD (Bahn, 2007b; Tame, 2009). Others felt pressured into CPD by managers fulfilling organisational requirements (Gould et al, 2007; Tame, 2009).
Discussion
Health care, nursing roles, and professional requirements have metamorphosed during the period in which these studies were undertaken. Nurses must respond to increasingly complex patient needs, demonstrate critical thinking and evidence-based decisions while delivering efficient, compassionate care (Willis, 2015; Irwin et al, 2018; NHS England and NHS Improvement, 2019). All studies confirmed nurses' awareness of professional requirements to facilitate care through maintaining and updating skills, as discussed by Glasper (2018). Nurses must be empowered to access CPD (Mazhindu, 2014).
Nurses' professional motivation was threatened when CPD engagement was thwarted. Insufficient organisational or managerial support, or disparity, meant nurses were struggling to balance personal resources against professional demands. Organisational austerity affects CPD and expecting nurses to use personal resources is a concerning trend (Shaw, 2012; Glasper, 2015; Jones-Berry, 2016; House of Commons Health Committee, 2018). Nurses are spending personal time and money on CPD (Keogh, 2014; Jones-Berry, 2016; Glasper, 2018). Personal sacrifices are considerable, particularly for those with families (Dowswell et al, 2000; Ellis and Nolan, 2005). Nurses struggle to maintain an acceptable work-life balance, citing insufficient developmental opportunities as the top reason for leaving (Jones-Berry, 2016; NHS England and NHS Improvement, 2019). Some feel bullied into CPD; Tame's (2011, 2012) emotional language of ‘horizontal violence’ highlighted this. Discord impacts retention within organisations and the profession (Hasselhorn et al, 2003).
Bungeroth et al (2018) and Glasper (2018) emphasised CPD is a basic requirement, with reduced resources potentially preventing nurses from re-registering (House of Commons Health Committee, 2018). Reduced workforces, or nurses whose practice is outdated, may have far-reaching consequences as they train the next generation (Glasper, 2018). CPD should be viewed as an investment, increasing retention amid global concerns regarding nursing shortfalls (Health Workforce Australia, 2014; Wong et al, 2015; NHS England and NHS Improvement, 2019; Haddad et al, 2020).
Although managers and organisations must govern activities, their approach is crucial (Ellis and Nolan, 2005; Hughes, 2005; Wong et al, 2015) as they influence the largest employee group (Glasper, 2018; NHS England and NHS Improvement, 2019; Haddad et al, 2020). They must recognise that as nursing transforms, so do individual career trajectories (Pool et al, 2015). This is particularly relevant in a predominantly female profession where many require flexible shift patterns, fitting in with personal responsibilities (NHS England and NHS Improvement, 2019; Haddad et al, 2020). No nurse should believe their development is considered insignificant (Hasselhorn et al, 2003; NHS England and NHS Improvement, 2019). Attempts to mitigate barriers must be considered (Brook et al, 2019).
Role extension and revisions to UK nurse education affect CPD (Wong et al, 2015; Kristjánsson et al, 2017; Irwin et al, 2018). New nurses require up-to-date and relevant support and development (Quek and Shorey, 2018; Brook et al, 2019). Imminent pre-registration amendments necessitate further CPD evaluation (NMC, 2018b). Mazhindu (2014) identified that nurses with extended roles still struggle to receive suitable CPD, as found in this review (Gould et al, 2007). Collaboration between universities may facilitate opportunities for both groups (Kristjánsson et al, 2017; Gray et al, 2018).
The importance of employers' support cannot be underestimated (Jones-Berry, 2016). Maintenance and development of professional roles through CPD is acknowledged by many UK organisations, with professional bodies desiring their support (Willis, 2015; Bungeroth et al, 2018). As more nurses undertake primary research, CPD that improves the quality of research reporting could be valuable given the weaknesses identified in the studies. This review shows nurses' professional motivation incorporated a desire to improve patient safety and enhance care. CPD engagement is essential to this with the potential to transform workplace cultures (Bjørk et al, 2009; Shaw, 2012; Zander et al, 2016; NHS England and NHS Improvement, 2019). Leadership influences extend to facilitating or preventing implementation of learning from CPD, potentially inhibiting contemporary, evidence-based practices (Jones-Berry, 2016; NHS England and NHS Improvement, 2019). Organisational or managerial disengagement may affect organisational ranking. The UK's Care Quality Commission (2020) considered evidence substantiating that staff receive appraisal of learning needs, adequate support and training to deliver safe, effective care.
Limitations
Incomplete reporting resulted in an inability to confirm participant workplaces. Failure to successfully contact authors resulted in study exclusion. Despite hoping to find studies from across the UK, only studies based in England were retrieved. The absence of exploration from across the wider UK may affect findings.
Conclusion
Bahn (2007b) identified three essential components to effective healthcare delivery: employer, nurse, and patient. Forming the bulk of healthcare workforces, nurses are vital (Haddad et al, 2020). Throughout 40-year careers, CPD must be facilitated (Bjørk et al, 2009; Pool et al, 2015; NMC, 2018a). As pre-registration education transforms, and patient acuity increases, so must CPD, enabling continuous development of competent, highly skilled practitioners (Irwin et al, 2018; NMC, 2018b; Quek and Shorey, 2018).
Nurses recognise that CPD impacts professional status and competence. This review identified factors influencing CPD engagement as nurses' individual resources, professional motivation, organisational commitment to learning and development and managerial support. Organisations and managers must commit to supporting CPD. The value of nurses' CPD must be elevated by professional bodies, governments and global organisations. The consequences of decreased development or depleted workforces affects healthcare for everyone.
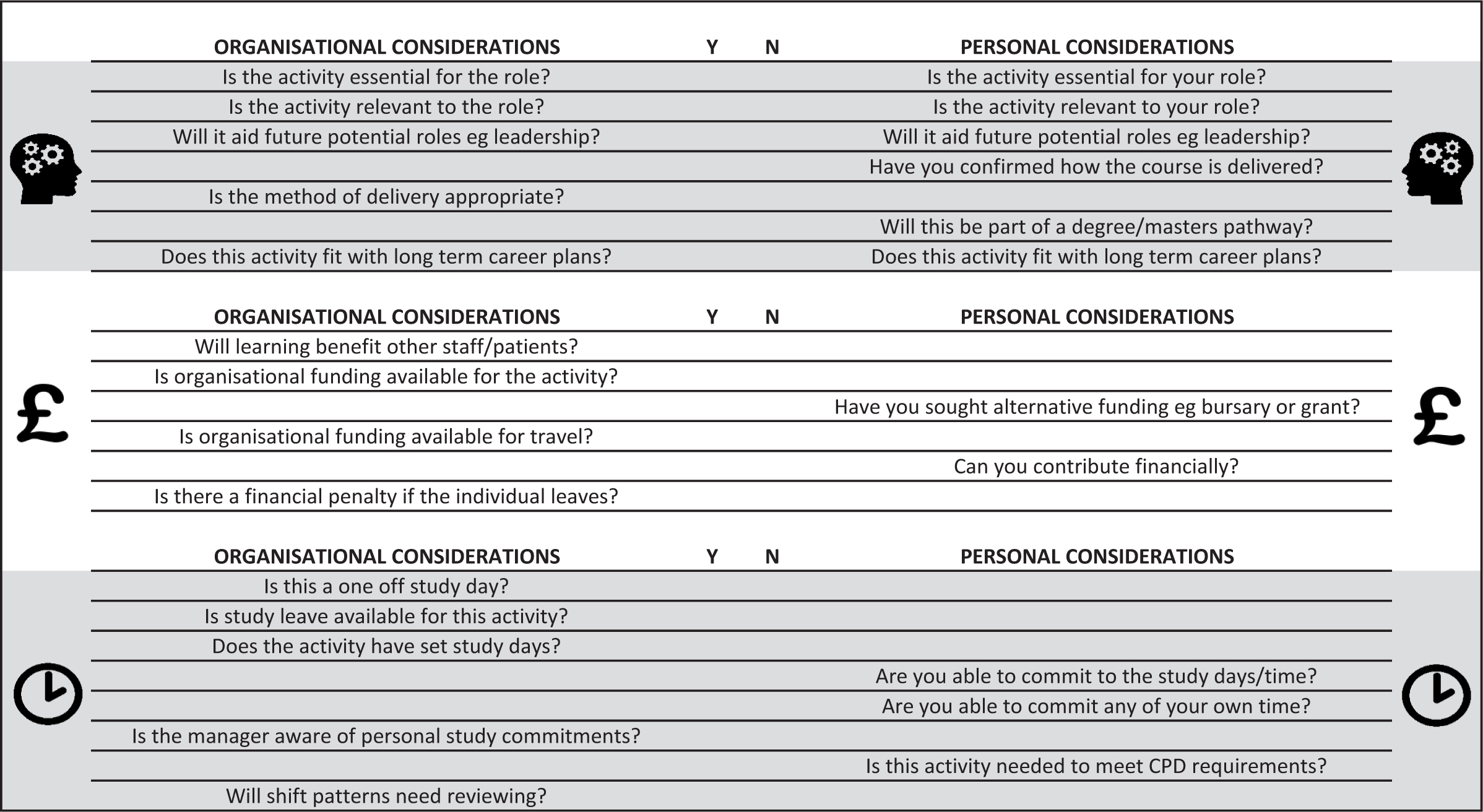
Educators can facilitate CPD for individuals and organisations, thereby safeguarding care standards (Smith, 2009; Sykes et al, 2014). They could coordinate organisational and managerial support, which nurses find invaluable, as this review identified. To aid discussions, a checklist has been developed (Figure 2), which could be used by individual nurses, managers and appraisers. Central to discussions is the need to ensure individuals meet professional requirements. Although the influence of each factor (individual resources, professional motivation, organisational commitment and managerial support) will vary, individuals should evaluate these. Appropriate CPD engagement will maintain and develop practice, benefitting the organisation and patients.
To support this, the authors recommend:

