About 6% of hospitalised patients require invasive nutrition support (Elia, 2015), the majority being nasogastric (NG) or nasointenstinal (NI) feeding. Of the blindly placed (unguided) feeding tubes, 1.5% enter the respiratory tract and, though most are detected and removed, one third (0.5%), result in pneumonia or pneumothorax (Taylor, 2018). Applying this to the 790 000 UK feeding tubes used in 2015 (NHS Improvement, 2016), would equate to nearly 4000 major complications (Taylor, 2018). Guided tube placement offers a means of detecting tube misplacement before the tube deeply enters the lung.
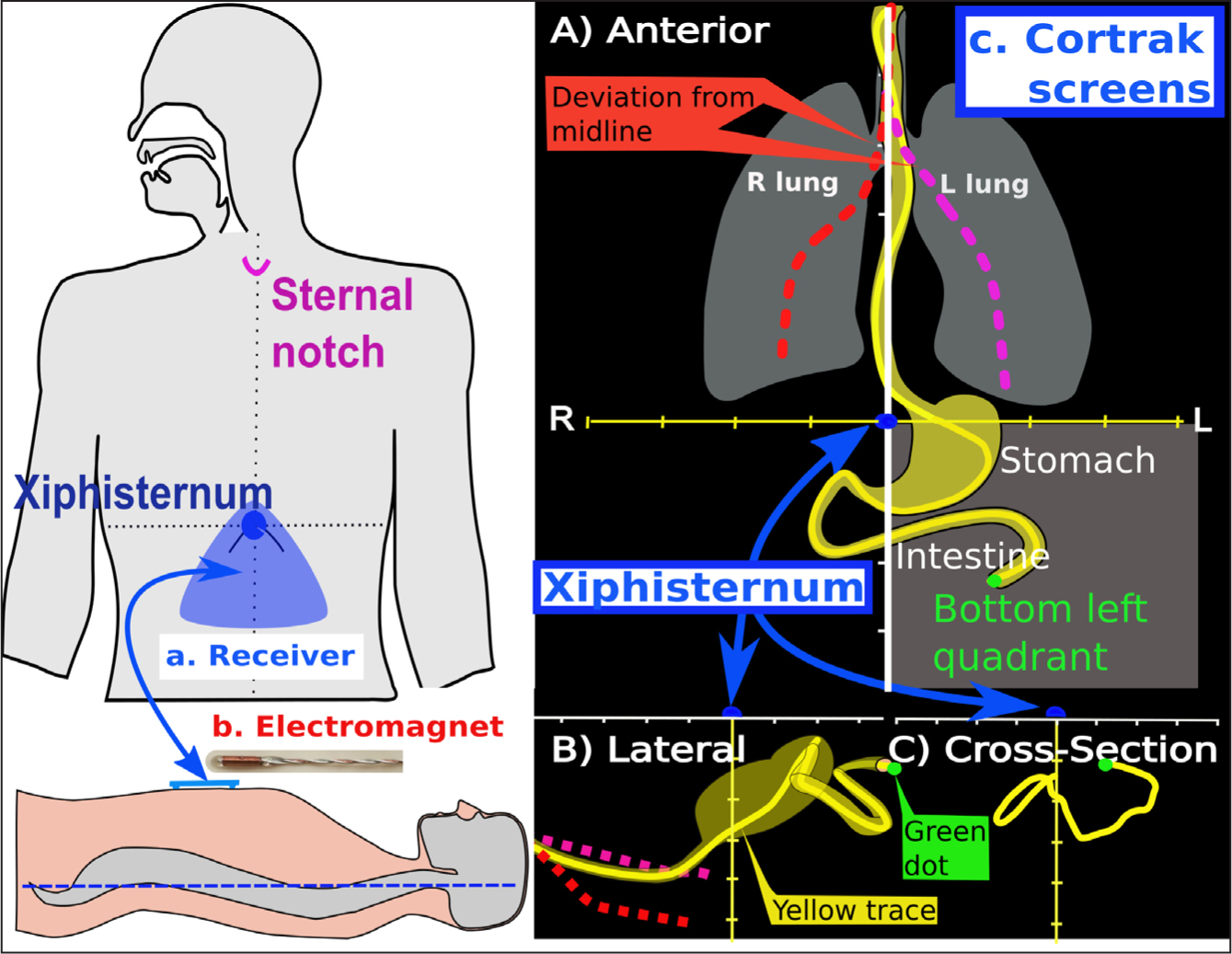
Cortrak is the most widely used bedside guided tube placement system (Medex, 2017). As shown in Figure 1, Cortrak consists of a receiver unit (a) that detects the tube guidewire's electromagnet (b) inside the body and the computer generates a screen trace (c) displaying the tube path frontally (A), patient's head at the top, from the side (B), head at the left and in cross-section (C). From the patient's perspective of ‘left and right’ the electromagnet is seen as a green dot tracing a yellow path on the screen. A ‘gastric trace’ moves vertically down the midline on the anterior (A) screen, turns left close to the xiphisternum (Figure 1, blue dot), then downward and then right into the intestine. The lateral screen path moves left to right, deep in the oesophagus, becoming shallow in the stomach, then deep intestinally. The cross-section screen shows depth from the abdominal surface and only displays a path once below the anterior screen horizontal line and to the right of the vertical midline.
Interpretation of Cortrak placement has been congruent with X-ray (McCutcheon et al, 2018; Powers et al, 2018). However, this appears to be expertise dependent, evidenced by 54 US and eight UK undetected misplacements, defined in the UK as a ‘Never Event’ (NHS Improvement, 2016); most such events resulted in severe complications or death (Metheny and Meert, 2014; 2017; Bourgault et al, 2017; Strategic Executive Information System (StEIS), 2018). The major cause of undetected placement appears to be inaccurate trace interpretation caused by insufficient training (Bryant et al, 2015). Although manufacturer guidance advises a minimum of three supervised placements to achieve competence (Avanos Medical Inc, 2018), expert centres have suggested that between 10 and 75 are required (McCutcheon et al, 2018; Bourgault et al, 2019). Unfortunately, there is no widely accepted evidence-based method of Cortrak interpretation.
To address this, the ‘GI flexure’ system was developed by characterising the shape of the Cortrak trace at different flexures (Taylor, 2018):
In contrast, if manufacturer guidance was used to interpret Cortrak traces, 38% of safe GI traces might be incorrectly considered lung placements because they deviate >5cm from the vertical midline, 49% of oesophageal traces would be accepted as gastric and 12% of gastric traces would be rejected because they were in the upper left anterior screen quadrant (Taylor et al, 2017a; 2017b). Similarly, of six undetected lung misplacements in patients who received feed, using manufacturer guidance, four traces might mimic receiver misplacement or unusual anatomy; all suffered aspiration pneumonia and one died (Taylor et al, 2019). In contrast, the ‘GI flexure’ system characterised anatomical points on the Cortrak trace and differentiated all lung misplacements from safe GI placements (Taylor et al, 2017a; 2017b; 2019).
The authors audited the ‘GI flexure’ system of Cortrak trace interpretation against X-ray evidence to tube position. Radiological criteria for GI tube position were:
Where possible, it was radiologically confirmed whether the tube was visible at:
Methods
Design and study population
The authors prospectively observed the accuracy of the ‘GI flexure system’ of Cortrak tube trace interpretation against radiological assessment in consecutive intensive care unit (ICU) patients requiring primary NI tube placement for clinical reasons at Southmead Hospital, Bristol. Patients were excluded if tube placement was aborted before reaching the gastric body or there was no radiological evidence of tube position.
For each electromagnetic (EM) trace a research dietitian (ST, KA, RC) attempted to confirm that the tube was safely within the stomach by identifying GI flexures on the trace (Taylor et al, 2017a; 2017b; Taylor, 2018). Two ICU consultants, blinded to the EM results, independently reviewed coincidental X-ray or CT scan post-tube placement. The first radiological image and any later image showing deeper tube placement were scored and analysed separately, then combined. To check sensitivity, four X-rays of lung placements were included without the knowledge of the consultants doing radiological assessment.
Statistical analysis
In a previous study of EM-guided placement, the EM-trace and/or clinical symptoms indicated that 10.3% of tubes initially entered the respiratory tract (Taylor et al, 2017b), whereas 1.5% of blindly placed tube remain undetected until X-ray (Taylor, 2018). A sample size of 134 is required to detect an effect size of -0.01 (equivalent to a 1% misplacement rate), assuming a power of 0.8 and significance of 0.05 for a one-tailed test of proportions. A one-tailed test is appropriate when looking at the probability of X-ray detection of lung misplacement after it had been interpreted as safe from an EM trace. The Kappa statistic was used to measure inter-rater reliability, a measurement of how consistent raters are. The McNemar test specifically looks at only the measurements where a disagreement occurred, ignoring all the cases where the raters agree. In this instance, it is used to detect whether there is a systematic difference in how the raters disagree; for example, does one rater say ‘unsure’ when another would say ‘unsafe’. Discrepancies are described.
As an audit of current standards, using routine records and no study-related interventions, ethical approval was not required for this study.
Results
Study population
Between 5 April 2016 and 11 January 2019 the authors attempted 244 primary NI tube placements, of which 185 had an X-ray or CT scan while the tube was in situ. Patient demography and clinical state were similar between those with and without X-ray or CT scan except for initial tube position (Table 1). Where NI placement failed, the tube was often quickly removed.
| Parameter | No X-ray or CT | X-ray or CT | P-value | |||
|---|---|---|---|---|---|---|
| Median or n | IQR or % | Median or n | IQR or % | |||
| Group | N | 59 | 25.7 | 185 | 74.3 | |
| Age | 52.7 | 38–53.2 | 52.4 | 36.6–67.7 | 0.54 | |
| Sex | Male | 40 | 67.8 | 132 | 71.4 | 0.84 |
| APACHE 2 | Score | 16 | 11–22.3 | 16 | 10–20 | 0.56 |
| Disease | Medical | 12 | 20.3 | 42 | 22.7 | 0.76 |
| Neurosurgical (non-trauma) | 12 | 20.3 | 30 | 16.2 | ||
| Surgery (general) | 19 | 32.2 | 53 | 28.6 | ||
| Trauma | 16 | 27.1 | 60 | 32.4 | ||
| Consciousness | Awake | 16 | 27.1 | 35 | 18.9 | 0.41 |
| Sedated | 39 | 66.1 | 136 | 73.5 | ||
| Unconscious | 4 | 6.8 | 14 | 7.6 | ||
| Airway | Normal | 13 | 22 | 24 | 13 | 0.18 |
| Endotracheal | 43 | 72.9 | 144 | 77.8 | ||
| Tracheostomy | 3 | 5.1 | 17 | 9.2 | ||
| Tube placement | Day | 4 | 3–4.7 | 4 | 3–5.7 | 0.46 |
| Initially respiratory tract | 6 | 10.2 | 21 | 11.4 | 0.88 | |
| Stomach | 13 | 22 | 5 | 2.7 | <0.0001 | |
| Duodenum (d) part 1 | 6 | 10.2 | 9 | 4.9 | ||
| d2 | 1 | 1.7 | 2 | 1.1 | ||
| d3 | 2 | 3.4 | 9 | 4.9 | ||
| d4 | 12 | 20.3 | 50 | 27.7 | ||
| Jejunum | 25 | 42.4 | 110 | 58.7 | ||
CT=computerised tomography; IQR=interquartile range
Radiological confirmation
Sensitivity and groups analysed
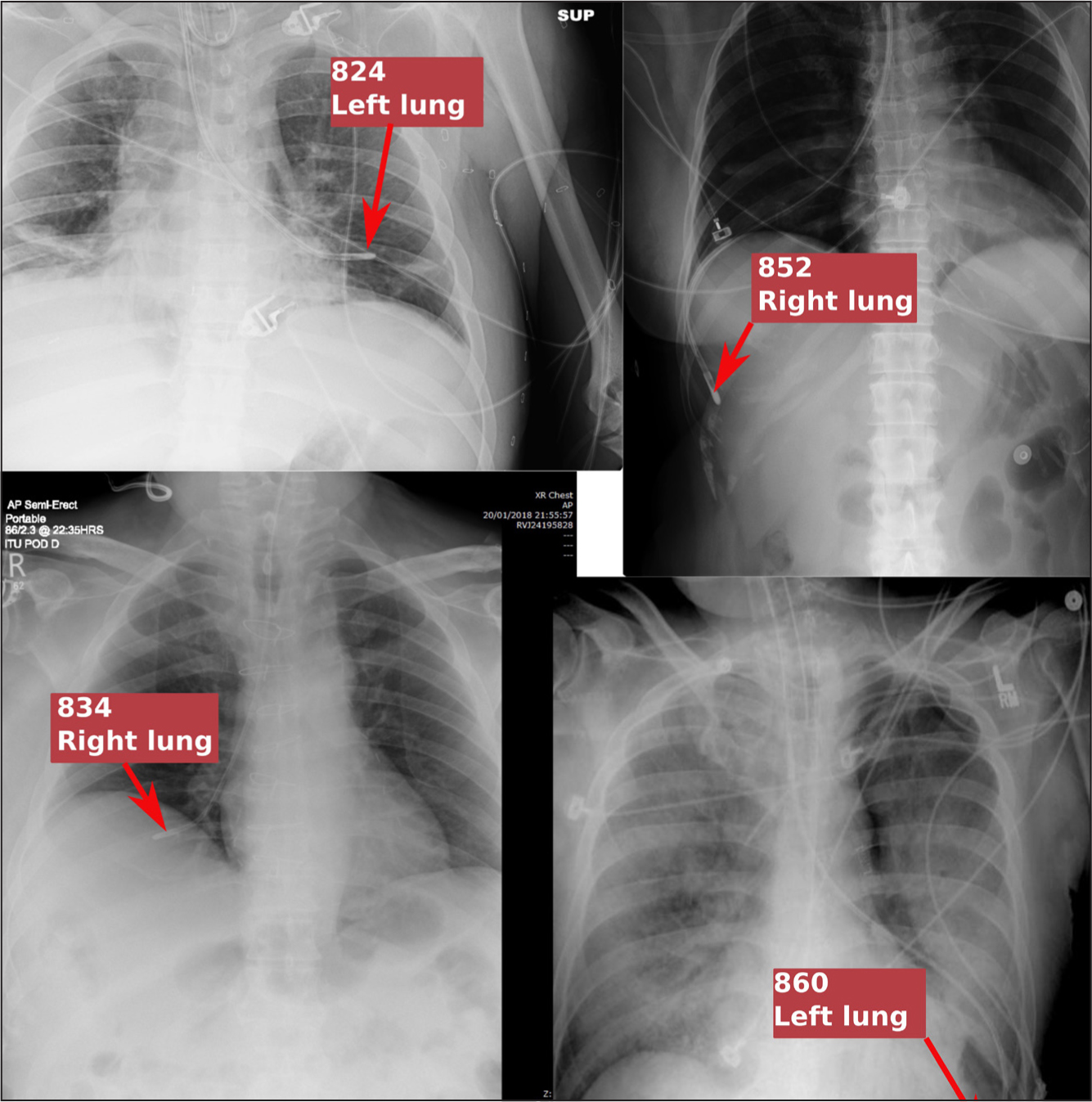
Both consultants correctly categorised four X-rays as lung placements (Figure 2). Median time to first X-ray or CT scan was 1 day (interquartile range (IQR): 1-3) and when including images that showed more of the placement, 2 days (IQR): 1-5). Agreement between radiological scoring for ‘first’ and ‘all’ images was similar, so only ‘all’ image scoring was compared to Cortrak.
Inter-rater scoring
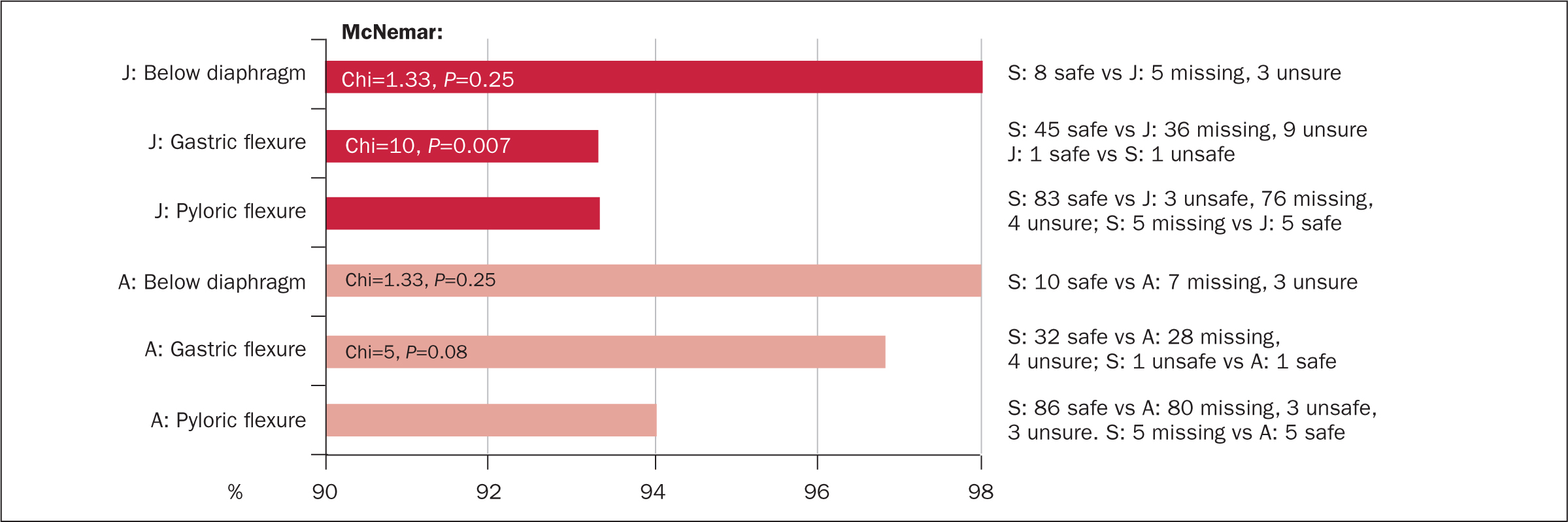
Kappa tests of agreement were not possible for Cortrak vs X-ray because all the Cortrak traces were interpreted as ‘safe’ and therefore systematically different from X-ray interpretation. McNemar tests, or its variant, could only be done when there was the same number of choices by both raters.
Despite Cortrak traces and/or clinical symptoms initially indicating respiratory placement in 11.4% of cases, Cortrak operators ultimately deemed all as safely within the GI tract. In the below diaphragm, gastric and pyloric flexures, radiological raters J and A agreed with Cortrak interpretation in 93.3-98.3% of cases (Figure 3). Disagreement was mostly because radiological raters were uncertain, this was significant for rater J at the gastric flexure. Intestinal Cortrak interpretation was contradicted radiologically when the first radiological record:

In one patient with abnormal anatomy, the gastric flexure was not identified, but other flexures confirmed GI position.
Inter-rater analysis showed the radiological ‘gold standard’ to be flawed with 3-18% disagreement (Figure 5). The highest agreement among raters was in the visibility of the tube below the diaphragm, followed by absence of bronchial bifurcation; presence beyond the pylorus; and presence beyond the gastric flexure.

Discussion
Patient population
Patients for whom Cortrak traces and X-rays were available for analysis had similar characteristics to patients without X-rays except that the latter group were more likely to have failed intestinal tube placement (13% vs 5%) and had the tube removed early, hence no confirmatory X-ray.
Primary outcome
Agreement between Cortrak interpretation and radiological images was high (93.4–98.3%) but not sufficient to validate the GI flexure system by ruling out the expected 1.5% incidence of lung misplacements detected by end-of-procedure X-ray. However, although 11.4% of tubes initially appeared to enter the bronchus based on the Cortrak trace and/or clinical symptoms, similar to the authors' previous study (10.2%) (Taylor et al, 2017a; 2017b), X-ray showed no undetected misplacements. Both radiological raters detected the four lung placement X-rays substituted into the list and had a high, though imperfect, level of agreement.
Radiological discrepancy with Cortrak
Discrepancies between Cortrak showing tubes passing through the pylorus and radiological interpretations contradicting this appear to be artefacts. In two the radiological image showed the tube had regurgitated into the stomach >24 hours after the Cortrak trace; regurgitation was confirmed by subsequent Cortrak trace. In three other patients, the first X-rays failed to clearly show the pylorus, but subsequent X-rays showed probable or definite intestinal placement. Except for the one tube that failed to remain in the intestine and was removed, the remaining four were used for feeding and drugs for 5-13 days without incident until blocked or the patient had transitioned to NG feeding (both n=2).
Interestingly, rater J was more certain of tube safety than rater A at the bronchial bifurcation and below the diaphragm, whereas rater A was more certain a tube had safely passed beyond the gastric flexure. No pattern was apparent regarding the tube beyond the pylorus. In the authors' view, radiological assessment of tube tip position has significant limitations.
Limitations
Radiological images were taken for clinical reasons, not NI tube confirmation, and therefore sometimes lacked adequate clarity or covered too little anatomy. In addition, radiological raters examined records retrospectively, in four batches and without clinical context. These factors are likely to increase the number of records where the rater was unsure of tube position and prone to error due to fatigue. Conversely, Cortrak traces were interpreted during tube placement. Nevertheless, both raters correctly diagnosed the four lung placements covertly substituted into the list when they had expected correctly placed intestinal tubes.
Safety and efficacy of Cortrak confirmation
Except for 2.7% of tubes, where intestinal placement failed, all were used for feeding. The fact that no patient aspirated feed indicates that all Cortrak confirmations were safe. However, these Cortrak traces were interpreted by experts using the evidence-based GI flexure method (Taylor et al, 2017a; 2017b). The experience level of other Cortrak operators is unknown and manufacturer guidance or other published methods of identifying Cortrak traces are not objective or evidence based.
Conclusions and recommendations
There was a high level of agreement between Cortrak and radiological interpretation. This was not high enough to prove that Cortrak could reduce end-of-procedure detection of lung misplacement to below the blind insertion rate of 1.5%. Failure was principally due to some radiological records being unclear or not covering the full anatomy. However, of the 244 Cortrak placements all lung misplacements were detected during placement. Use of GI flexures to interpret Cortrak traces accurately confirmed tube position. Further testing will necessitate a similar sized study, but using prospective radiological imaging covering the required anatomical areas.

