The onset and prolonged restrictions of the COVID-19 pandemic necessitated a move away from traditional face-to-face consultations between patients and clinicians to the increased use of virtual care as a routine part of patient services in healthcare systems (Walsh et al, 2021). Many clinics facilitated unscheduled phone call arrangements, where patients could call nurses who would provide them with rapid access to information and advice. This mode of care has continued and expanded following the pandemic. However, there is a lack of information about the impact of such unscheduled virtual consultation systems on nurses' workloads or patient evaluation of receiving care in this way.
A search of the most recent literature on the evaluation of unscheduled virtual care clinics reveals that they offer a safe, low-cost, flexible clinical care (Due-Christensen et al, 2015; Remy et al, 2020). Patient satisfaction was reported to be high for virtual care, but it should be noted not that all patients reported such high levels of this (Chew et al, 2019; O'Reilly et al, 2019).
Barriers to virtual care were reported as time constraints, high workloads, having to access relevant patient information by phone in the absence of electronic records, and knowledge or training deficits (Macartney et al, 2012). Other barriers identified to the uptake of virtual care were a lack of regulatory and accrediting policy and institutional skills and support (Adler-Milstein et al, 2014).
Unscheduled virtual nurse-led care is being increasingly provided across many long-term conditions, with diabetes being one area that uses this mode of care delivery (Due-Christensen et al, 2015; Jardine et al, 2021; Townsend et al, 2021). Telehealth, including unscheduled telephone virtual care, is used to manage various long-term conditions including diabetes (Evans et al, 2012; Remy et al, 2020). The need for flexible, cost-effective, clinically based initiatives in diabetes care to be developed and expanded is particularly urgent. The incidence of patients being diagnosed with diabetes globally is predicted to increase significantly (Saeedi et al, 2019; Khan et al, 2020; Gupta et al, 2022). By 2036, it is predicted that there will be approximately 200 000 more people in Ireland with type 2 diabetes than in 2020 (Standl et al, 2019; Pierse et al, 2021).
Healthcare organisations need to continue developing and expanding patient-initiated, nurse-led unscheduled care using technology in a sustainable and economically viable way. To inform this, nurses' practices and patient satisfaction with the services being provided at this study site in an acute care hospital in Ireland need to be examined.
Aim
The study aimed to examine nurse practices and patient satisfaction with the delivery of unscheduled nurse-led virtual care for diabetes provided in an outpatient setting in an acute care urban hospital.
Objectives
The aims of this study were to:
- Examine the activities associated with unscheduled nurse-led virtual care
- Assess patients' experiences of engaging in unscheduled nurse-led virtual care in the diabetes clinic.
Methodology
Study design
A cross-sectional, descriptive survey design was used. Data were collected between 9 May and 19 August 2022 in an acute care hospital in Ireland.
Data on clinical nurse specialists' (CNSs') practices related to unscheduled nurse-led virtual telephone consultations were collected using an outputs activities log adapted from Brady and Drennan (2020).
Data on patient satisfaction were collected using a patient satisfaction and enablement questionnaire adapted from the Patient Enablement and Satisfaction Survey developed by Desborough et al (2014; 2016).
Ethics
Ethical approval was granted by the hospital research ethics committee and the School of Nursing and Midwifery, Trinity College Dublin.
Sample and eligibility criteria
All unscheduled telephone calls made by patients, relatives or carers aged >18 years received by two CNSs at the diabetes clinic were deemed eligible for study inclusion.
Participants for the patient satisfaction and enablement survey were recruited through a gatekeeper (administrator) using the patient administrative system. The sample size target of 66 participants for the survey was based on 10% of the estimated number of consultations in a 1-month period (n=660).
Data collection
Data were collected from the nurse activities log and the patient satisfaction survey and enablement survey.
Over the study period, the nurse activities log was completed by the CNS after each unscheduled telephone virtual care consultation. The final activities log consisted of two sections, which covered call details and call outcomes when possible.
The patient satisfaction survey and enablement survey comprised four sections which included: patient satisfaction; patient enablement; diabetes care support; and demographic data. Questionnaires were administered to patients following their unscheduled telephone virtual consultation with the CNS. A member of the research team who was not involved in patient care contacted patients by phone and completed the survey using Qualtrics survey software.
Data analysis
The quantitative data collected from the activities logs were entered into Excel then exported to IBM SPSS v25. Descriptive and inferential analyses were conducted where possible. Categorical data were analysed by counting the frequencies (number and percentages) of participants. Continuous variables are reported using means, medians and standard deviations.
Results
Nurse activities log
During the study period, the CNS in the diabetes outpatient clinic received 1812 unscheduled telephone calls (Figure 1). The weekly average over the study period was 121 (SD 22.37), with a daily average of 25.38 calls.
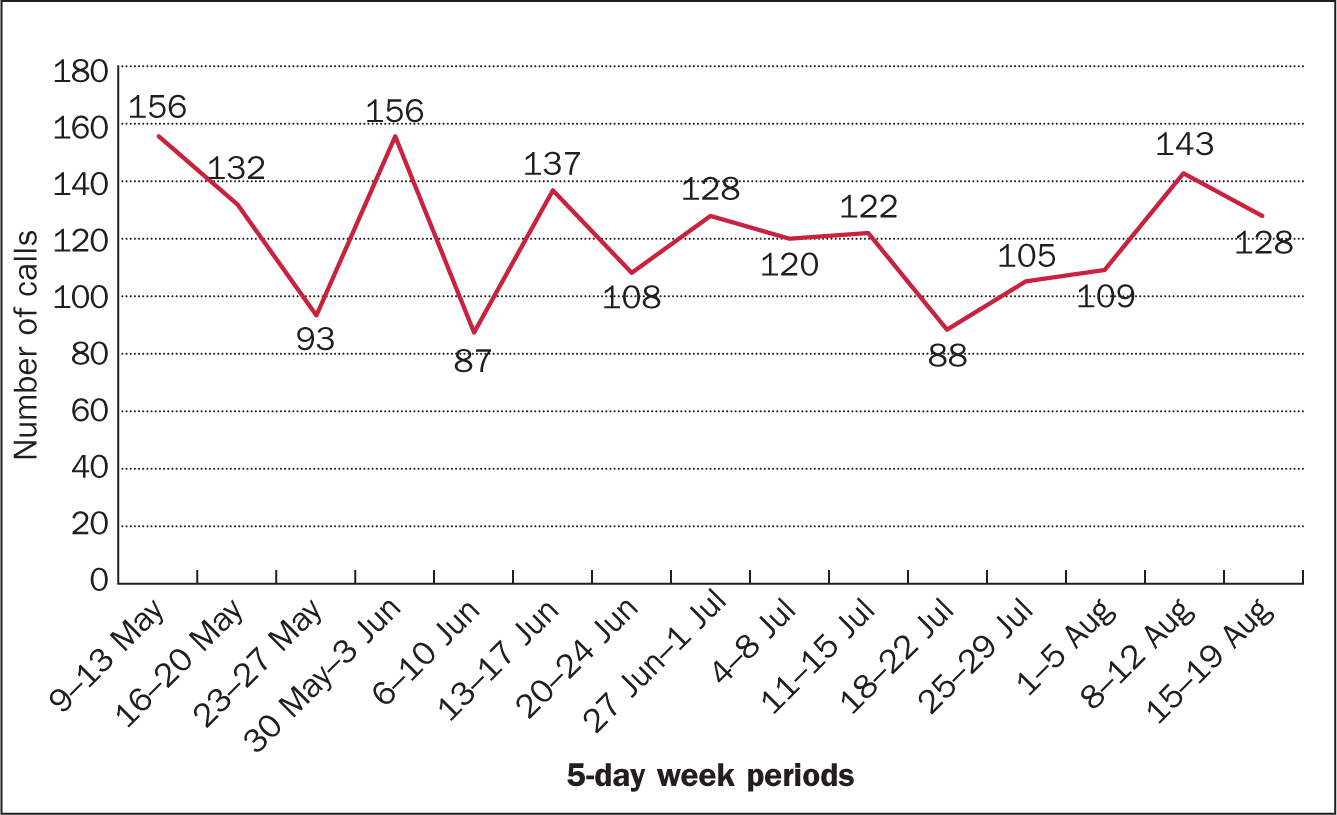
During this period, 337 unscheduled patient-initiated nurse-led telephone consultations were recorded in the activities log. These calls represent 18.6% of the total number of unscheduled telephone calls (n=1812) received by the CNSs. Because of the CNSs' workload burden, not all calls were included in the activities log.
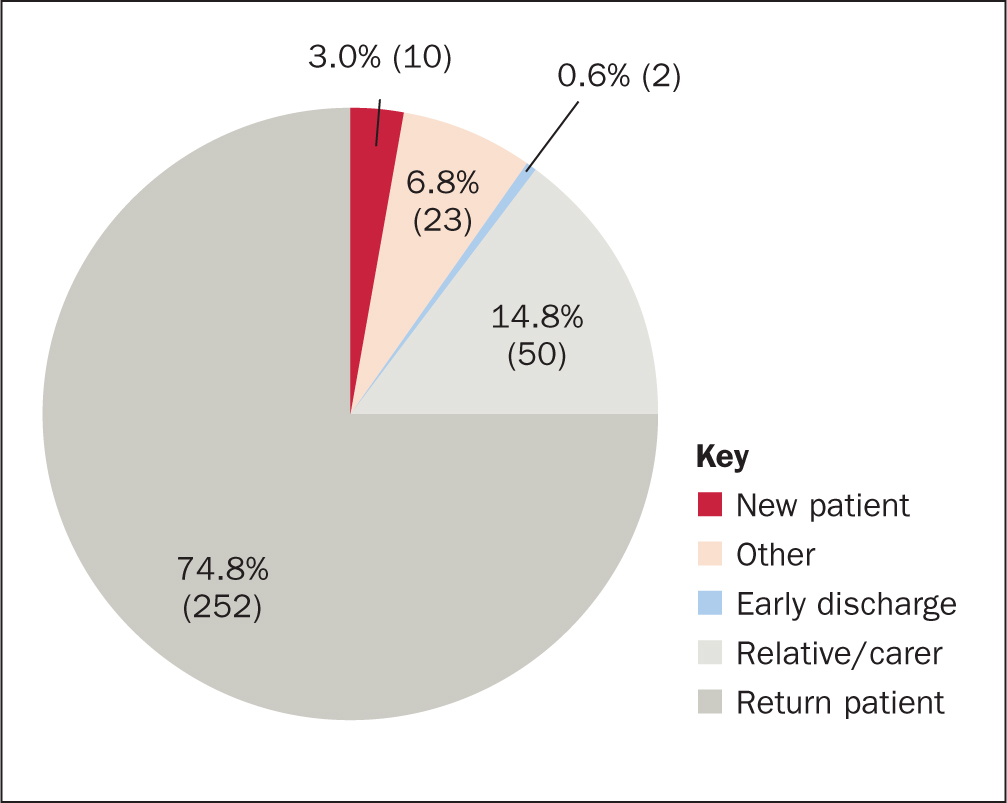
The duration of the 335 unscheduled telephone calls was recorded. The total call time over these 15 weeks (5-day weeks excluding two public holidays) was 2636 minutes (44 hours). The average length of a telephone consultation was 7.87 minutes and just over half of the calls lasted 5 minutes. Unscheduled consultation calls were primarily from return patients (74.8%) seeking ongoing clinical advice and 14.8% were from carers and relatives seeking advice. Two calls (0.6%) were from patients who were discharged early from hospital because of the telephone support provided by nurses (Figure 2).
The activities log had 19 options that could be selected to indicate the outcome or actions taken following each call logged. Multiple options could be selected per call (Table 1). There were 865 outcome activities attributed to the 337 unscheduled telephone calls that were logged. The average number of relevant outcomes per unscheduled telephone consultation was 2.5 (SD 1.76), with a median of 2 and in a range of 0-8 outcomes. Outcome activities are listed in Table 1 in descending order of frequency. The most common outcome (74.5%) associated with the unscheduled consultations was the CNS providing the caller with ‘expert advice/education on care and management of diabetes’. Unscheduled calls to the CNS facilitated early access to the diabetes outpatient clinic (18.1%) and avoided potential emergency department presentations (5.3%).
Table 1. Outcome of unscheduled calls
| Outcome items in order of most reported | n (%) |
|---|---|
| Gave expert advice/education on care and management of diabetes | 251 (74.5) |
| Involved in a shared decision-making strategy regarding patients' own care and management | 86 (25.5) |
| Patient agreed on suggested medication treatment options | 86 (25.5) |
| Discussed medication treatment options with caller | 85 (25.2) |
| New prescription issued as per nurse prescriber remit | 71 (21.1) |
| Early access to diabetes OPD clinic facilitated | 61 (18.1) |
| Laboratory investigations reviewed | 40 (11.9) |
| Referral made (if yes, state to whom) | 39 (11.6) |
| Laboratory investigations ordered as part of unscheduled call | 23 (6.8) |
| Scheduled to return for CNS OPD review | 23 (6.8) |
| Able to avoid an ED presentation (potentially) | 18 (5.3) |
| De-prescribed medication | 6 (1.8) |
| Prescription required consultation with a doctor | 6 (1.8) |
| De-prescribing required consultation with a doctor | 6 (1.8) |
| Gave expert advice/education on diagnosis of diabetes | 5 (1.5) |
| Patient disagreed on suggested medication treatment options | 2 (0.6) |
| Inpatients for a shorter number of days/early discharge facilitated | 2 (0.6) |
| Recommend presentation to ED related to condition | 2 (0.6) |
| Other (specify) | 53 (15.9) |
CNS: clinical nurse specialist; ED: emergency department; OPD: outpatients' department
Patient satisfaction and enablement survey
Eighty-one participants completed the survey (Table 2). Section 1 had 14 items and examined how satisfied patients were with the virtual care. Participants scored each item on a 5-point Likert scale, with a potential maximum score of 70. A response of ‘uncertain’ was considered as being dissatisfied with the care received. A total score ≥56 indicated overall satisfaction.
Table 2. Patient characteristics (n=81)
| n (%) | |
|---|---|
| Female | 44 (54.3) |
| Male | 37 (45.7) |
| Mean age (SD) | 54.51 years (16.45) |
| Overall health | |
| Excellent | 2 (2.5) |
| Very good | 25 (30.9) |
| Good | 31 (38.3) |
| Fair | 19 (23.5) |
| Poor | 4 (4.9) |
The average satisfaction score was above 56, with 96% of participants either satisfied or very satisfied with the care they had received (Figure 3). The two items with the highest level of satisfaction were ‘The diabetes nurse was very professional’ and ‘The care I received from the diabetes nurse was of a high quality’. The item with the lowest level of satisfaction was ‘I was included in the planning of my care’ (Table 3).
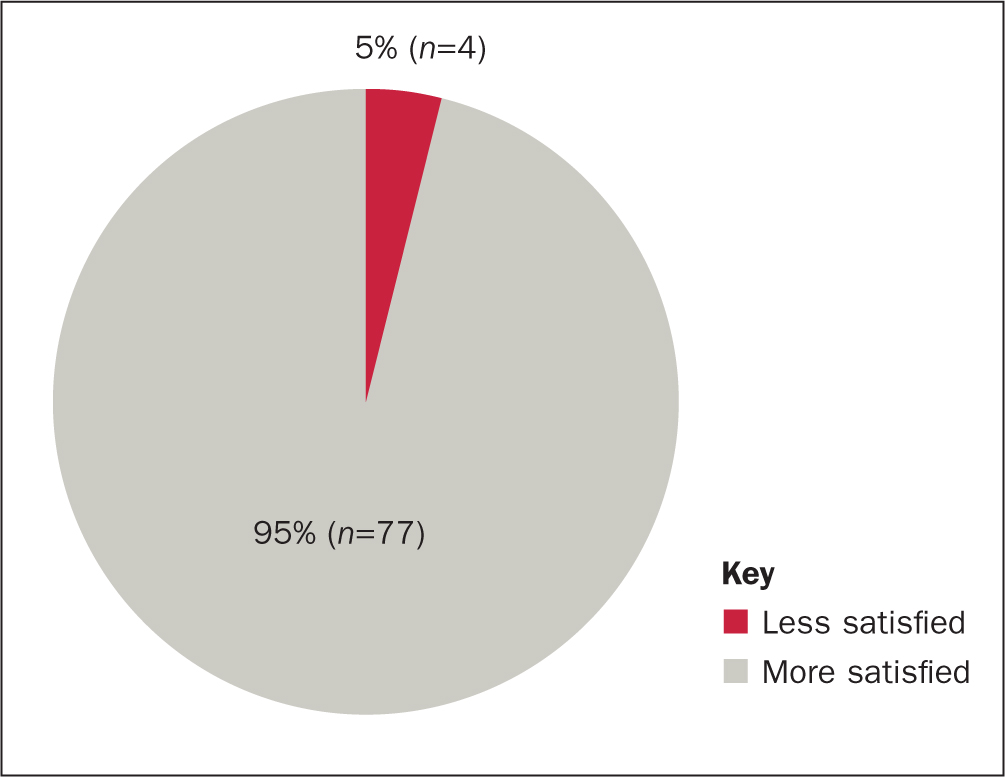
Table 3. Frequency of patient satisfaction scores (n=81)
| Questions | Strongly disagree n (%) | Disagree n (%) | Uncertain n (%) | Agree n (%) | Strongly agree n (%) |
|---|---|---|---|---|---|
| The diabetes nurse was understanding of my personal health concerns | 3 (3.7) | 0 (0) | 0 (0) | 13 (16) | 65 (80.2) |
| The diabetes nurse gave me encouragement in regard to my health problem | 1 (1.2) | 0 (0) | 0 (0) | 12 (14.8) | 68 (84) |
| I felt comfortable to ask the diabetes nurse questions | 1 (1.2) | 0 (0) | 0 (0) | 10 (12.3) | 70 (86.4) |
| My questions were answered in an individual way | 1 (1.2) | 1 (1.2) | 1 (1.2) | 17 (21) | 61 (75.3) |
| I was included in decision-making | 1 (1.2) | 1 (1.2) | 6 (7.4) | 19 (23.5) | 54 (66.7) |
| I was included in the planning of my care | 1 (1.2) | 0 (0) | 7 (8.6) | 22 (27.2) | 51 (63) |
| The treatments I received were of a high quality | 2 (2.5) | 0 (0) | 3 (3.7) | 14 (17.3) | 62 (76.5) |
| Decisions regarding my healthcare were of a high quality | 1 (1.2) | 1 (1.2) | 1 (1.2) | 16 (19.8) | 62 (76.5) |
| The diabetes nurse was available when I needed them | 1 (1.2) | 0 (0) | 3 (3.7) | 16 (19.8) | 61 (75.3) |
| The diabetes nurse spent enough time with me | 1 (1.2) | 1 (1.2) | 0 (0) | 12 (14.8) | 67 (82.7) |
| I was confident with the diabetes nurse's skills | 1 (1.2) | 0 (0) | 1 (1.2) | 11 (13.6) | 68 (84) |
| The diabetes nurse was very professional | 1 (1.2) | 0 (0) | 0 (0) | 5 (6.2) | 75 (92.6) |
| Overall, I was satisfied with my diabetes healthcare | 0 (0) | 3 (3.7) | 0 (0) | 12 (14.8) | 66 (81.5) |
| The care I received from the diabetes nurse was of a high quality | 0 (0) | 0 (0) | 1 (1.2) | 7 (8.6) | 73 (90.1) |
Section two of the survey had five items that measured patient enablement on a three-point Likert scale: ‘same or less’; ‘better’; and ‘much better’ (Table 4). More than 80% of participants reported better or much better enablement in all items after engaging in virtual care. Overall, 5% (n=4) of participants' patient enablement scores were the same or worse since the unscheduled telephone consultation with the diabetes CNS.
Table 4. Patients with improved patient enablement (better and much better) (n=81)
| Survey question | Frequency | % |
|---|---|---|
| Able to understand your illness | 74 | 91.4 |
| Able to cope with your illness | 72 | 88.9 |
| Able to keep yourself healthy | 70 | 86.4 |
| Confident about your health | 70 | 86.4 |
| Able to help yourself | 74 | 91.4 |
Discussion
The purpose of this study was to examine CNSs' practices and patient satisfaction with the delivery of unscheduled nurse-led virtual care for people with diabetes in an outpatient setting in an acute care hospital in Ireland.
Just under 60% of participants were self-referrals, and the majority (74.5%) sought advice and education on the care and management of their condition. Evans et al (2012) and Due-Christensen et al (2015) reported similar results, with the majority (55.3%) of calls being self-referrals lasting 5 minutes or less, most which related to advice and education.
The potential extent of the work involved in providing an unscheduled nurse-led virtual care service was not considered in this study. However, the average number of relevant outcomes per unscheduled telephone consultation was 2.5, which suggests a substantial impact on workload for nurses given that this is not scheduled into their normal working day. Howland et al (2021) also found virtual care increases the workload for nurses. This portion of the CNS daily workload had not been fully captured previously and is an important consideration in terms of providing future virtual care services that are sustainable.
Patients who used the unscheduled telephone call service reported high satisfaction levels, which supports the retention and future expansion of the service. Similar services in Denmark are supported by the CNS being able to access electronic medical records (Due-Christensen et al, 2015). In this study, the diabetes clinic's unscheduled incoming requests for health care are conducted solely by telephone. It was not possible for the CNSs to access to electronic records, which added to the workload burden of both nurses and administrators and limited efficiency, and is a barrier to the sustainability and effectiveness of nurse-led virtual patient care (Mills et al, 2023).
As patients and staff become more technologically competent with the proliferation of technology, there will be opportunities to enhance and expand the service through communication platforms such as Webex or Zoom. Due-Christensen et al (2015) recommended greater use of videoconferencing technology for the provision of care. It is recommended that CNSs and other healthcare and administrative staff are trained in the use videoconferencing to aid virtual healthcare delivery. This medium would be advantageous for both unscheduled and scheduled calls to the service as the proliferation of technology and patient knowledge of said technology increase over time (Bestsennyy et al, 2021).
The findings of this study identified 18 occurrences of diabetes patients potentially avoiding presentation to an emergency department because they had access to unscheduled nurse-led, telephone-facilitated diabetes care. Comparable research undertaken in the UK and Australia reported that nurse-led virtual care helped reduce the number of patients presenting to emergency departments (Evans et al, 2012; Karimi et al, 2021). Evans et al's (2012) UK study witnessed 218 occurrences of callers (92.7%) avoiding presenting to the hospital. Due-Christensen et al (2015) reported that a similar telephone service had aided in reducing the number of type 1 diabetes patients needing to attend hospital, with 15 out of a total of 17 patients at risk of requiring admission avoiding having to attend hospital because of this service. The present study did not aim to identify potential or actual cost savings for the health service; however, it is likely that this would be an outcome of this type of service based on reduced admissions. The Irish healthcare funding model does not calculate or remunerate the cost of CNS time for unscheduled telephone calls.
This study along with previous research suggest this type of service supports diabetes self-management skills of patients at home, treatment compliance, safety and effectiveness, improves patient access to healthcare services, potentially reduces emergency department presentations and increases avoidance of hospital admission (Evans et al, 2012; Remy et al, 2020).
However, a sustainable funding method that includes remuneration and staffing for this nurse led-service and IT that is reliable and fit for purpose are essential when planning to expand virtual care services. Without reliable internet and wi-fi connection with patients, the service may be unsatisfactory and result in failed or suboptimal consultations (Kobeissi and Hickey, 2023).
Other key aspects of essential infrastructure include education regarding relevant policy and its implementation in terms of delivering nurse-led virtual clinic services, for example data protection requirements. Organisational training concerning the application of procedures and processes for delivering effective nurse-led virtual clinics are essential for all members of the multidisciplinary team, including administrative staff (Kobeissi and Hickey, 2023).
Strengths and limitations
This study explored unscheduled virtual care provided by CNSs in the diabetes outpatients' department of an urban hospital using reliable and validated instruments. Although this is a small study, the findings contribute to the body of evidence on the hidden and extensive work undertaken by CNS when providing unscheduled virtual consultations in the diabetes outpatients' department. The study identifies the nature of nursing interactions and interventions undertaken during these unscheduled calls and their potential contribution to emergency department presentation avoidance.
The study was somewhat limited by the volume of data collected, which was below the levels that the authors had hoped to gather. This was down to several factors, including time constraints on the CNS completing the daily activities log. The recording of such data by CNSs is problematic given the unscheduled nature of their work; other data collection methods would need to be considered in future research.
Conclusion
The activity logs portion of the survey provide insight into an aspect of the clinic work being undertaken at one diabetes clinic that is often unseen and unaccounted for. The volume of time and effort accounts for a considerable portion of the clinics staff's weekly duties.
The efforts of the diabetes clinic are well regarded and recognised by the service users, with satisfaction levels with the care received being exemplary.
Remuneration, additional administrative and IT support along with policy development and education support are essential for the development and sustainability of this type of service.
KEY POINTS
- Most people calling a nurse-led diabetes clinic were existing patients seeking diabetes education and guidance.
- The majority of people using the service were very satisfied with it and felt better able to keep themselves healthy as a result
- Providing a service to receive calls adds substantial unscheduled work to the clinical nurse specialist workload
- Further research is needed to identify cost savings attributed to this service in terms of avoiding hospital admission
CPD reflective questions
- Consider the psychological benefits to those self-managing newly diagnosed diabetes from being able to gain expert advice by telephone without an appointment
- What other long-term health conditions might benefit from a similar service?
- Think about the education and skills you would need to conduct virtual care using different technologies
- What are the potential benefits of extending such a telephone diabetes service to operating out of hours, considering most patients would present to emergency departments if they did not have access to expertise provided virtually on demand?


