The World Health Organization (WHO) (2022) has raised the global significance of addressing psychological wellbeing, highlighting the pervasive impact of mental health disorders on individuals, communities and economies. The mortality gap for mental illness illuminates a stark disparity in healthcare outcomes, with studies consistently demonstrating that individuals grappling with mental health disorders face significantly higher mortality rates compared to the general population (Campion, 2019). This gap persists due to numerous factors, including inadequate access to healthcare services, stigmatisation, socioeconomic disparities, and the prevalence of comorbid physical conditions (Byrne, 2023). WHO (2022) emphasises the urgent need for comprehensive mental health policies and services, advocating for increased investment in mental health services. However, this is a longstanding issue, with policies in the UK and internationally attempting to address mental health outcomes for over a decade (HM Government and Department of Health, 2011; WHO, 2013). With progress still to be made, and updated policies retaining the same key objectives (WHO, 2021), never has the specialist role of the mental health nurse been more pertinent.
Mental health nurses are different from their adult nursing cousins, holding a multifaceted role in the care and support of individuals experiencing mental health challenges (Connell et al, 2022). The mental health nurse's role and identity is difficult to articulate, requiring inconspicuous skills, including:
With allocated powers under the Mental Health Act 1983(revised 2007) mental health nurses also need to balance complex legal and ethical landscapes to be able to make critical decisions regarding detainment and least-restrictive practice, always prioritising patient safety and dignity. Most importantly, they do this while building therapeutic relationships with patients, fostering the trust and collaboration essential for recovery (Haslam, 2023).
In the UK, unlike our counterparts in the USA, Canada and Australia, prospective nursing students apply to study in field-specific programmes, qualifying and registering as either an Adult, Child, Mental Health, or Learning Disability nurse (Bifarin et al, 2024). In 2015, The Shape of Caring review highlighted the importance of holistic, person-centred care, emphasising the need for mental health nurses to have more physical health skills (Willis, 2015). In 2018, acknowledging calls for a more generic skillset, the Nursing and Midwifery Council (NMC) document Future Nurse: Standards of Proficiency for Registered Nurses outlined new pre-registration standards (NMC, 2018). Mentors and sign-off mentors were replaced with practice supervisors and practice assessors, and revised standards were introduced. This single set of standards across all fields of practice marked a clear departure from previous field-specific competency-based approaches, requiring all pre-registration candidates to fulfil the same specific criteria or ‘proficiencies’ prior to qualifying and joining the register. This document has now been updated with minor changes to the language, structure and layout (NMC, 2024).
In the 6 years since these new standards were introduced, concerns have been raised about the interpretation and application of the listed proficiencies to the unique role of the mental health nurse (Warrender et al, 2024). There is a renewed focus on task-based assessments, with students assessed as ‘proficient’ for being able to perform a set task in a single placement area, without consideration of the depth of understanding, ability to retain the information after the single assessment point, or ability to apply this learning to other settings (Whaley et al, 2024). Furthermore, time devoted to meeting physical health proficiencies is time made unavailable for developing fieldspecific knowledge and skills, diluting mental health nursing programmes; although physical health skills are important, there are concerns that they could overshadow mental health nursing skills (Warrender et al, 2023).
Difficulties for students
One of the issues expressed in service evaluations for mental health nursing students is that they perceive proficiencies to be easier to achieve for their peers on the adult nursing programme. Mental health nursing students often face challenges in obtaining sign-off for individual proficiencies due to the wording used in the NMC documentation (NMC, 2024), which includes action verbs such as ‘uses’, ‘undertakes’, ‘inserts’ and ‘removes’. In many mental health settings, there will be no opportunity to ‘undertake’ respiratory or cardiac assessment, or to ‘insert’ or ‘remove’ a catheter. The NMC has therefore made provision for interpretation of these proficiencies, indicating that different fields ‘may require different approaches’ (NMC, 2024: 37). However, given the clear instructions within each individual proficiency that indicate that a student is required to actively ‘demonstrate’ their proficiency, practice assessors may not accept that direct observation of tasks is not always necessary, and students may struggle to find alternative ways to demonstrate the required level of knowledge and skill. Students often seek their own solution, resorting to ‘insight visits’ in other mental health settings to source opportunities as an alternative way to demonstrate proficiency away from the main placement hub.
Stacey et al (2015) described the hostility that students can face when starting a new practice placement, highlighting the significance of student compliance and submissiveness as crucial factors for gaining acceptance within their new team. Students often prioritise the development of the new and complex relationships with their practice assessors and supervisors. They acknowledge the heavy workload and care responsibilities shouldered by assessors, leading them to focus on tasks beneficial to the clinical setting, sometimes at the expense of their own learning (Stacey et al, 2015). Considering the potential for conflict regarding the assessment of physical health proficiencies in mental health settings, such behaviours are understandable, maybe even advisable. However, this will likely have further repercussions on their ability to obtain signoff on proficiencies.
As a solution to this issue, mental health nursing students often find themselves placed in acute care settings and encouraged to use the opportunity to acquire a list of proficiencies. However, as Bifarin et al (2024) highlighted, such placements often emphasise skill acquisition from a medical-model perspective, neglecting the essential therapeutic qualities and psychosocial interventions fundamental to mental health nursing practice. There is a perception that this is merely a tick-box exercise, and that students do not really need to understand the skills being evaluated, as they will not use these skills within their field of practice (Buescher and McGugan, 2022). There is no balance here; students are either in field-specific placements gaining mental health nursing skills, the development of which is not acknowledged, or they are working through a list of required proficiencies that may have little or no relevance in their chosen career.
Difficulties for assessors
Whaley et al (2024) found a significant barrier for student attainment originating from practice assessors themselves, and mental health nursing students have voiced frustration at assessors’ reluctance or refusal to sign off certain proficiencies during their clinical placements. By shifting towards generic proficiencies, the NMC is tasking mental health nurses with evaluating knowledge and skills with which they are not familiar and for which they have not received training, and assessors often do not feel competent to make judgements on what does or does not constitute ‘proficiency’.
Practice assessors may feel unable to sign off specific proficiencies due to their own lack of competency in clinical skills, highlighting concerns that this may breach the responsibilities and accountability of their own NMC registration (Whaley et al, 2024).
This issue is exacerbated by the ambiguity surrounding the wording of each proficiency. Varying interpretations of what qualifies as an acceptable proficiency contribute significantly to whether a student successfully achieves them or not (Christiansen et al, 2021; Finstad et al, 2022). Another example of this is evident in the NMC's statement that ‘the level of expertise and knowledge required will vary depending on the chosen field of practice’ (NMC, 2024: 32), which fails to offer a clear definition of how to understand these levels in relation to the context of the clinical setting and patient need. For a practice assessor who does not use a particular proficiency in their own practice, recognising the varying levels of proficiency may be beyond their capability, further reducing their confidence to sign off on assessment of those proficiencies.
In contrast to the previous Standards to Support Learning and Assessment in Practice (SLAIP) (NMC, 2008), which mandated an initial training programme followed by regular updates, the new standards do not stipulate that practice assessors undergo formal training and allow for practice supervisors to be recruited from a wide range of professions. Given that the standards and criteria for assessing student performance may be vague or open to interpretation, practice assessors may lack clear guidance on what constitutes proficiency in various clinical skills, making it challenging to assess students accurately and consistently. This creates an additional barrier for practice assessors, who are already juggling competing priorities and heavy workloads. Teaching may be a low priority, and the lack of comprehensive training in the assessor role can lead to highly subjective assessments (Stacey et al, 2015).
Difficulties for educators
Mental health nurse educators are aware of the need to promote the importance of physical health skills, given the morbidity and mortality associated with a diagnosis of serious mental illness (Warrender et al, 2023). Although the importance of teaching these skills is not denied, there are questions about how to make the skills relevant to students’ current learning and development needs, as well as their future careers as mental health nurses. There is a missing piece to this puzzle: the connection between assessing proficiency and the learning experience itself. Educators play a pivotal role here, and there is an opportunity to employ pedagogical methods that connect theory and practice. It is necessary to support both students and assessors to align the assessment requirements with their practical experience.
Different placements present different challenges. In mental health settings, practice assessors not only have limited resources and opportunities, but struggle with interpreting ambiguous guidance and may lack confidence in their own assessment skills. In acute care placements, students are set task-oriented objectives and must physically perform each skill to meet the requirement for proficiency sign-off without any consideration of the depth of knowledge and understanding necessary for clinical decision-making in their post-registration role. Students need to make links between the individual skill, the associated health need, and a holistic view of the patient that accounts for their mental health as well as their physical health (Bifarin et al, 2024).
Educators have a pivotal role in ensuring that mental health nursing students can gain physical health skills that complement more nuanced mental health skills in communication, therapeutic relationships, critical thinking, and values-based decision making.
A potential solution
Within mental health nursing education there now exists a persistent conflict between practice assessors evaluating the profession-wide proficiencies mandated by the NMC (2024) and mental health nursing students striving to meet these standards. For educators, it can be difficult to effectively support both parties, but a potential solution lies in contextualising proficiencies for the mental health nursing student audience, integrating them into pre-registration programmes in a way that values the role of the mental health nurse and embeds skill-based tasks into the specialised clinical settings and patient groups. By providing clear links between physical health skills and mental health practice, educators can constructively align the learning opportunities available in a mental health setting with the prescribed assessment of NMC proficiencies.
The Proficiencies Directory is an innovative and sustainable teaching method, developed by the authors, which provides a resource for mental health nursing students and their practice assessors during practice placements. Currently, the directory is accessed by the mental health nursing students at the authors’ HEI through their online Blackboard module (a web-based virtual learning environment and learning management system). Two parallel directories have been created, one for part 2 and one for part 3 of the undergraduate mental health nursing programme, with each directory providing resources which link directly to the NMC proficiencies mapped to that stage of the programme. Using the HEI's own technology and communication media has ensured that there have been minimal costs attached, other than those associated with academic time to create and update the learning resources and materials.
The Proficiencies Directory in part 2 and 3 have enabled mental health nursing students to access asynchronous activities that are directly targeted at developing the knowledge and skills required to attain identified proficiencies, while supporting them to synchronise with practice placement experiences and opportunities. Identical formatting of both the part 2 and part 3 directories provides consistency and familiarity for students. Importantly, providing mental health nursing students with this resource at the beginning of both part 2 and part 3 ensures sufficient time for engagement, allowing students to develop more insightful and meaningful action plans before starting each practice placement. The Proficiencies Directory encourages mental health nursing students to delve into broader reading materials and engage in reflective exercises on their practical experiences. Figure 1 provides an extract from part 2 of the Proficiencies Directory.
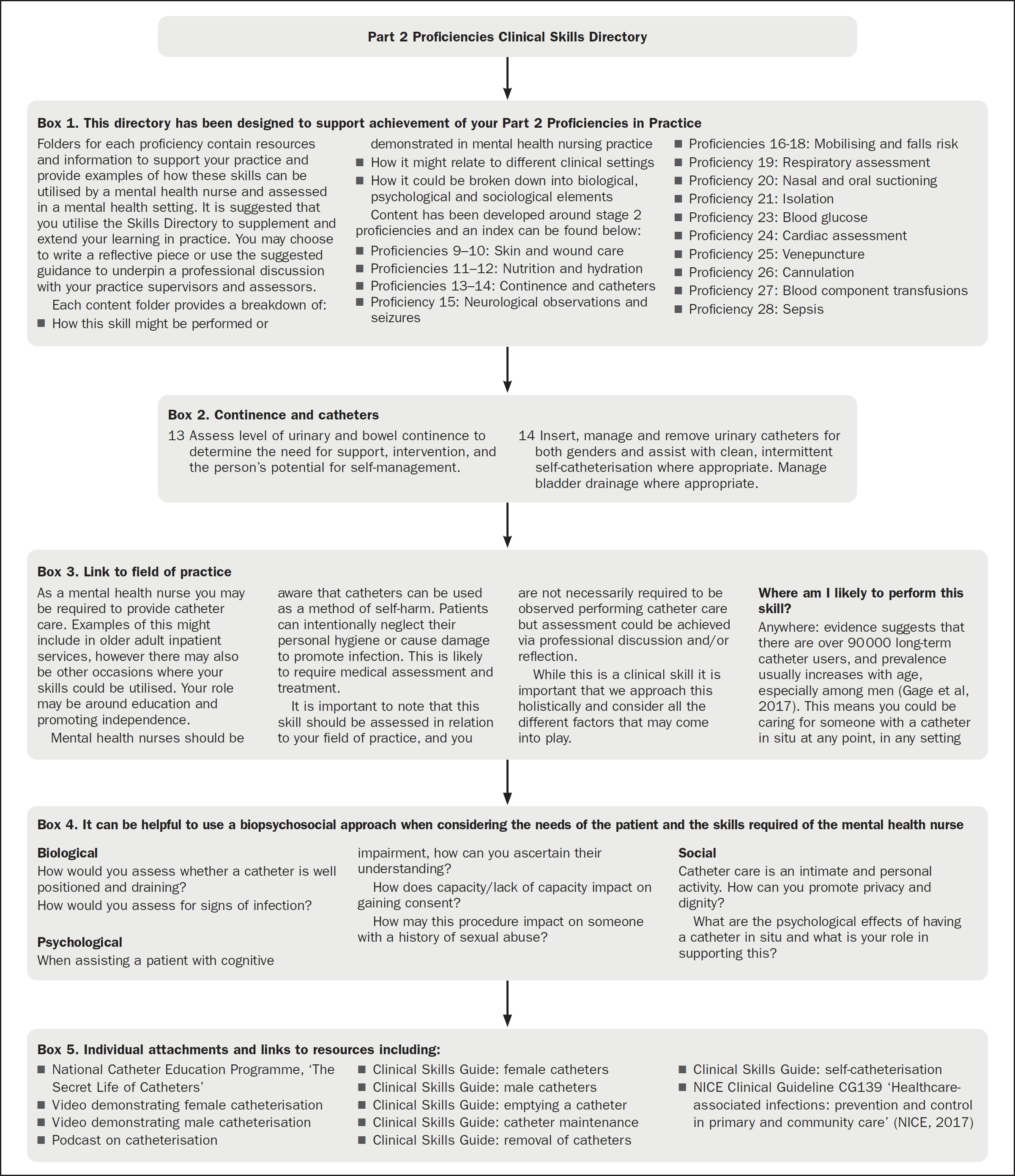
A specific content area was created within the Practice Assessment Module area on Blackboard, allowing students to quickly access a general introduction and overview of what is contained within the directory (Figure 1: Box 1). Beneath this, subfolders are arranged according to NMC proficiency number (Figure 1: Box 2). Within each subfolder, resources are arranged according to the same format. First, there is a link to the field of practice (Figure 1: Box 3) followed by examples linking the proficiency to the biopsychosocial model (Figure 1: Box 4). This additional information aims to emphasise the relevance of clinical proficiencies to mental health nursing students by highlighting when and where students can expect to use each technique within their own practice. Beneath this, within the same subfolder, a variety of asynchronous learning resources are provided (Figure 1: Box 5).
Evaluation and impact
End-of-module evaluations provided the following student insights into the use of the Proficiencies Directory:
The aim of the Proficiencies Directory is to aid understanding and contextualise proficiencies for both students and assessors. Early findings are that the Proficiencies Directory is both sustainable and replicable across other nursing programmes within the HEI and has potential for adoption by other HEIs. Indeed, the MSc in Mental Health Nursing course at the university has subsequently adopted this resource.
Limitations
It is acknowledged that this evaluation is limited in its data retrieval and further work is required for a more comprehensive triangulation of data across the student, practice educator and academic educator spectrums prior to wider integration into nursing curriculum.
A limitation of the Proficiencies Directory is that it is currently only accessible for students via the HEI's own technology and systems, and that practice partners lack access to, as well as knowledge of, the availability of this resource. Work is now underway to develop publicly accessed content to share with local placement providers.
Conclusion
Challenges faced by mental health nursing students, assessors, and educators in meeting proficiency standards set by the NMC are multifaceted and require innovative solutions. The evolution of nursing education towards generic proficiencies has brought about a need for contextualisation within the specialised field of mental health nursing. The authors have sought to adopt a solution-focused approach, as exemplified by the introduction of the Proficiencies Directory in their educational institution, which represents a promising solution to bridge the gap between prescribed proficiencies and the unique demands of mental health nursing practice. The Proficiencies Directory not only provides structured resources for mental health nursing students to develop necessary skills, but also offers guidance for practice assessors in evaluating student performance. By aligning learning experiences with assessment criteria, educators can facilitate a more comprehensive and meaningful learning journey for mental health nursing students.
Future efforts should focus on expanding access and promoting awareness among stakeholders. Additionally, ongoing research and evaluation are essential to ensure the effectiveness and sustainability of these initiatives across various nursing programmes and institutions. Ultimately, addressing the difficulties encountered in mental health nursing education requires collaboration, creativity, and a commitment to advancing pedagogical practices to better prepare future mental health nurses for the complexities of their role. Through initiatives such as the Proficiencies Directory, educators can ‘shave the corners’ which are the barriers to mental health nursing students learning and attainment, allowing the ‘square peg’ of generic standards to fit with more ease into the ‘round hole’ for fieldspecific nursing programmes.


