I am an experienced registered nurse with over a decade of practice in health care, including 5 years in the field of infection prevention and control (IPC). Like many of my colleagues, I faced numerous challenges during the COVID-19 pandemic, an experience that has strengthened my commitment to nursing and patient safety.
I have led several quality improvement initiatives at my organisation, which led me to receive the Gold Award in the Infection Prevention Nurse of the Year category this year at the BJN Awards. Here, I would like to present a summary of some of these initiatives.
Improving standards of care of central venous catheters
In October 2022, a quality improvement strategy was implemented in response to an increase in the number of central lineassociated bloodstream infections (CLABSIs) at a local intensive care unit (ICU). Baseline data were collected over 3 months to observe the practices for inserting and maintaining central venous catheters (CVCs) and identify potential lapses in care. Unfortunately, the audit revealed significant concerns around the care that CVCs received.
The audit revealed non-compliance with hygiene recommendations before touching CVCs, as per the World Health Organization (WHO) recommendations (Sax et al, 2007). It was observed that the lack of this action was primarily driven by the use of gloves during intravenous (IV) drug preparation, with approximately 40% of the nursing staff wearing gloves during this process. A literature review demonstrated that gloves are unnecessary for routine IV drug preparation (Gorski, 2017) and that change in this field was possible (Dunn et al, 2019).
Using the Model for Improvement (MFI) methodology (Langley et al, 2019), the objective was to achieve this by eliminating the unnecessary use of gloves during routine IV drug preparation and reinforce appropriate hand hygiene. Crucial to this quality improvement project was the engagement of the ICU nursing staff, who were recognised as the primary users of CVCs. Nursing staff were asked to assess the need for gloves during their routine IV drug preparation at each encounter, and to wear gloves only if deemed necessary, such as for cytotoxic and anti-monoclonal therapy drugs (Gorski, 2017). Before implementing this change, comprehensive training around glove use and line care was provided alongside the information collated from audit and national data. Visual posters and screensavers were created based on staff feedback from anonymous questions identifying staff concerns. Statistical process control charts were also employed to understand the practice variation and analyse the data.
During the evaluation phase, we achieved a sustainable compliance rate of non-glove wearing above 90% for IV drug preparation (less than 10% wearing gloves) among ICU nursing staff. This outcome, a testament to our collective efforts, was not without its challenges. It was difficult to determine which intervention was the most effective, although conducting the myth-busting exercise dispelled common staff concerns.
The findings align with the COM-B behaviour model (West and Michie, 2020), which indicates that increasing capability, opportunity, or motivation can help bring about behaviour change. Staff were motivated to adopt this approach by demonstrating the environmental impact of unnecessary glove use.
Improving care of peripheral vascular access devices
Taking into consideration an increased number of bloodstream infections related to peripheral vascular access devices (PVADs) since 2019 at a local trust, a stakeholder group exercise was held to identify critical failures within the PVAD care process. Concerns and frustrations regarding the existing electronic patient record system PVAD documentation were raised. During the transition from a paper-based documentation to an electronic patient record system in 2019, several data entry sites for PVAD documentation were missed. This system made it challenging for staff to locate where the insertion of PVAD was documented or where maintenance checks were being recorded.
The focus group agreed that it would be beneficial to have a single, easily accessible form for performing cannula maintenance checks, similar to the paper-based documentation previously in place. The group suggested incorporating appropriate PVAD documentation into an application on a handheld electronic device that nursing staff use for observation records.
Pioneering this innovation by first recognising collective learning from PVADrelated bloodstream infections through the process and need for adequate PVAD documentation, and with the support of IT engineers, we designed a simple tool that can be easily implemented in clinical practice. The design of this new PVAD documentation system in the application had no extra cost for the trust and could translate into improving staff performance around PVAD documentation. As described by nursing staff on the wards, one of the main benefits of this application is that it allows nursing staff to enter patient data at the point of care once and without the risk of missing data, duplicating it or recall bias.
Development of a skilled and efficient IPC link workforce
As the trust's IPC education lead, education is fundamental to every patient and/or staff contact I encounter. To ensure that staff can adhere to high-quality standards, it is essential to provide them with comprehensive education and training around the fundamental principles of IPC. A detailed competency booklet that included a mix of theoretical knowledge and competency assessment tools in IPC was assembled. This approach helped to ensure that the IPC link practitioners demonstrate competency in the vital role they play in supporting people to understand and follow IPC recommendations. With the IPC link network now fully compliant with competencies, the next step will be to expand this initiative to different staff groups, such as ward managers and departmental matrons, throwing the net wider and improving IPC's presence in the clinical environment.
Reducing the five moments of hand hygiene to three
Finding new alternatives, techniques, and ideas is paramount to improving productivity and enhancing the quality of care in healthcare settings, yet IPC teams often struggle to find new creative approaches to influence practice. Improving hand hygiene compliance is no less daunting as compliance is often not up to the mark (Gould et al, 2017).
Klymenko and Kampf (2015) argued that healthcare staff are usually uncertain about when hand hygiene should be performed to reduce the risk of infection, highlighting the need for further quality improvement interventions. Additionally, Woodard et al (2019) found that only one out of every five individuals could recognise the WHO ‘5 moments for hand hygiene’ model, suggesting that a new model may be required.
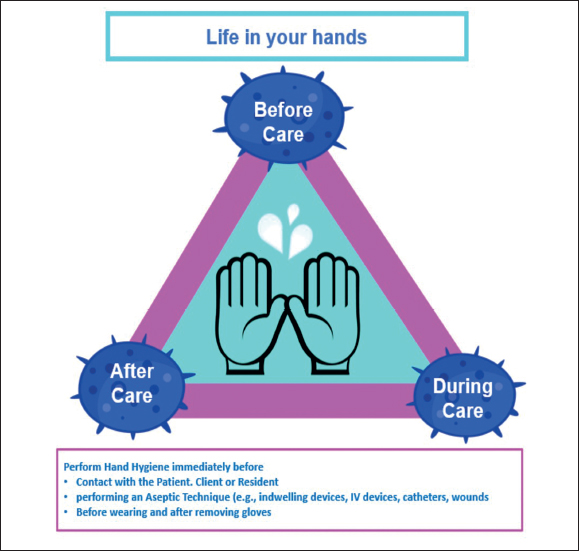
In collaboration with other students on the MSc in IPC course at the University of West London, a new model for hand hygiene was developed, named the ‘Hand Hygiene Triangle: Life in Your Hands’ (Figure 1). This model identifies three critical points that trigger an opportunity for hand hygiene, which are based on the WHO moments 1, 2, 4, and 5. By focusing on the key points that represent a greater risk for patients acquiring an infection (moments 1 and 2), this simplified framework can be more accessible for staff to understand and promote excellent practices while ensuring patient safety. Trust feedback has been positive, although discussions on how to review this model's effectiveness are required before implementation.
‘Significant and sustainable change can only occur if the key staff members are willing to co-operate ’
Conclusion
Recognition and successful implementation of quality improvement projects often results in more effective internal processes and the IPC career path gives these opportunities in abundance as demonstrated above. Nonetheless, it is important to recognise that, although tools assist in identifying obstacles and solutions, significant and sustainable change can only occur if the key staff members are willing to co-operate. This complex dynamic should be based on genuine interpersonal and professional relationships if it is to improve patient care and delivery.
Receiving the Gold Award has been an incredible and humbling experience. This recognition has driven me to pursue my academic career further, with the hope of bridging the gap between evidence-based literature and clinical practice.


