COVID-19, caused by the SARS-CoV-2 virus, is a highly contagious respiratory illness that emerged in late 2019 and led to a global pandemic. We all remember the pandemic and the profound impact it had on populations worldwide. Although it has been a few years since the peak of the pandemic, COVID-19 continues to affect people globally. It is particularly important to understand the ongoing impact of the virus on vulnerable populations, such as stoma and ileoanal pouch patients, who face unique health challenges. This article examines the effects of COVID-19 on these patients, highlighting the need for continued vigilance and tailored healthcare strategies to support this susceptible group.
The COVID-19 pandemic resulted in significant morbidity and mortality, with millions of infections and deaths worldwide. When the pandemic began in early 2020, the knowledge of disease progression, including its non-respiratory symptoms, was unknown or very limited. As the pandemic progressed, health authorities around the world slowly learnt more about its pathology and associated non-respiratory symptoms. The UK was not an exception and vast research around symptoms has been conducted in the past few years to better understand COVID-19 and all its associated respiratory and non-respiratory symptoms. Additionally, when it comes to specialist areas, such as rare conditions, comorbidities and patients with unique needs, such as those with a stoma and ileoanal pouch, little is known about COVID-19-associated symptoms in this group.
COVID-19 symptoms are often perceived as respiratory only, however, recent findings (Alberca et al, 2021) have shown that gastrointestinal (GI) symptoms, which include lack of appetite, nausea, vomiting, diarrhoea and abdominal pain, are increasingly being recognised. In severe cases, inflammation caused by the virus can lead to ulceration of the oesophagus, stomach and duodenum. The reported incidence of GI symptoms associated with SARS-CoV-2 infection is around 50% of all patients (Chen et al, 2020; Brooks and Bhatt, 2021) and in some cases, these may be the only symptoms. Research (Lang, 2024) also demonstrates that the coronavirus enters epithelial cells by binding to ACE2 receptors, which are present in various body tissues, including the small and large intestines, an interaction that contributes to the prevalence of GI symptoms in COVID-19 patients.
A stoma (ostomy) is a surgically created opening into the abdomen that is used to divert the flow of faeces or urine outside the body (Marinova et al, 2021). When discussing enteral stomas, this usually includes ileostomy and colostomy, and less often jejunostomy.
An ileoanal pouch is created when the colon and rectum are removed, and a reservoir (pouch) is fashioned from part of the small intestine (ileum). The pouch is then joined to the anus and a temporary loop ileostomy is fashioned above the pouch. A loop ileostomy can be reversed in a separate operation (Perry-Woodford, 2018).
There are some complications associated with having an ileoanal pouch and stoma, such as pouchitis and high output. Pouchitis is an inflammation of the ileal pouch, causing symptoms such as urgency, increased faecal frequency (diarrhoea), abdominal pain, cramping, incontinence and bleeding. Treatment for pouchitis typically involves a 2-week course of antibiotics (ciprofloxacin or metronidazole), which is effective in most cases. If symptoms persist, healthcare providers may prescribe a longer course with a different antibiotic or a combination of antibiotics. In cases where pouchitis becomes chronic or does not respond to antibiotics, other treatment options may be considered (Shen, 2003).
A high-output stoma refers to a condition in which stoma output exceeds 1.5–2.0 L over a 24-hour period, although this can vary based on oral intake of food and fluids. Up to 31% of individuals with small bowel stomas may experience a high-output stoma (Nightingale, 2021).
The authors provide ongoing care for patients with a stoma and/or an ileoanal pouch in a variety of settings, including inpatients and outpatients, and for patients accessing telehealth services for advice. The clinical practice setting that offers patients with an ileoanal pouch and stoma a telephone and email adviceline has provided a unique opportunity to communicate and record numerous GI symptoms reported in patients during or post-coronavirus infection, with most patients being worried about new GI symptoms.
Therefore, a hypothesis that GI symptoms related to COVID-19 may make pouch or stoma function deteriorate or even mimic pouchitis symptoms in ileoanal pouches, and gastroenteritis in stoma patients, was proposed. The study aimed to investigate and test the hypothesis that GI symptoms related to COVID-19 may make ileoanal pouch or stoma function deteriorate or even mimic pouchitis or gastroenteritis symptoms, with the outcome potentially helping to improve patient care.
Data collection
The authors undertook a single-centre study with patients known to the authors' pouch nursing service. It involved a retrospective analysis of patients who had reported GI symptoms in the preceding 4 years (2020-2024) following infection with SARS-CoV-2. All patients had an ileoanal pouch or a stoma, and had had a positive lateral flow test or PCR test for coronavirus between 2020 and 2024.
Additional inclusion criteria were as follows:
The exclusion criteria were as follows:
The baseline data of patients' individual characteristics and symptoms during infection were collected using a COVID-19 symptoms-oriented questionnaire, developed locally by the authors' team. A summary of the information requested via the questionnaire is presented in Box 1. The data were anonymised and stored securely, and not shared with any third party.
Summary of the SARS-CoV-2 infection questionnaire
| Demographic data |
|
|
| Stoma/pouch history |
|
|
| COVID-19/coronavirus infection data |
|
|
| Symptom data |
|
|
Patients were recruited from the authors' outpatient settings and the patient adviceline, as well as in collaboration with the Red Lion Support Group and St Mark's Hospital Foundation, via their newsletters and social media accounts. The Red Lion Support Group is a registered charity supporting people living with an internal pouch; St Mark's Hospital Foundation is a registered charity that helps fund innovative research projects, and its vision is that of a future free from the fear of bowel disease through research, education and the dissemination of clinical excellence.
Patients were required to give study-specific informed consent to take part in the survey, which was administered online. Responses in the affirmative to five mandatory questions at the start of the questionnaire confirmed informed consent, after which patients went on to complete the survey. Potential participants had the opportunity to ask further questions before providing consent and were informed that they could withdraw consent at any time.
The data collection method protected patients' identities, by ensuring that any identifiable information was anonymised, and the final data collection sheet did not contain patient identifiers.
The need for ethical approval was considered; however, as the patient feedback project met the Health Research Authority criteria for a service improvement project (https://www.hra-decisiontools.org.uk/research/docs/DefiningResearchTable_Oct2022.pdf), it was decided that ethical approval was not necessary.
Findings
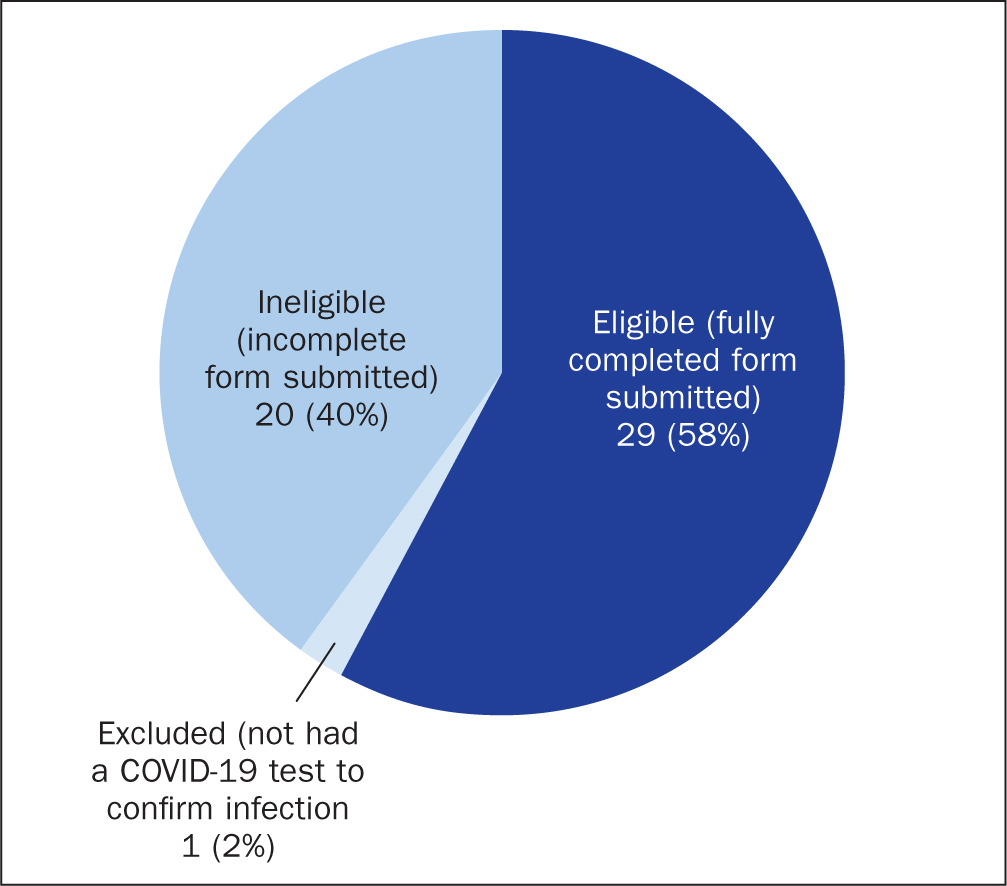
Fifty patients consented to take part in the study, of whom 30 (60%) completed the survey, with the remaining 20 leaving some sections blank; these 20 surveys were therefore incomplete and were not considered. One patient was subsequently excluded because they had not had a positive COVID-19 lateral flow or PCR test to confirm infection, so the adjusted number of final participants was 29 (Figure 1).
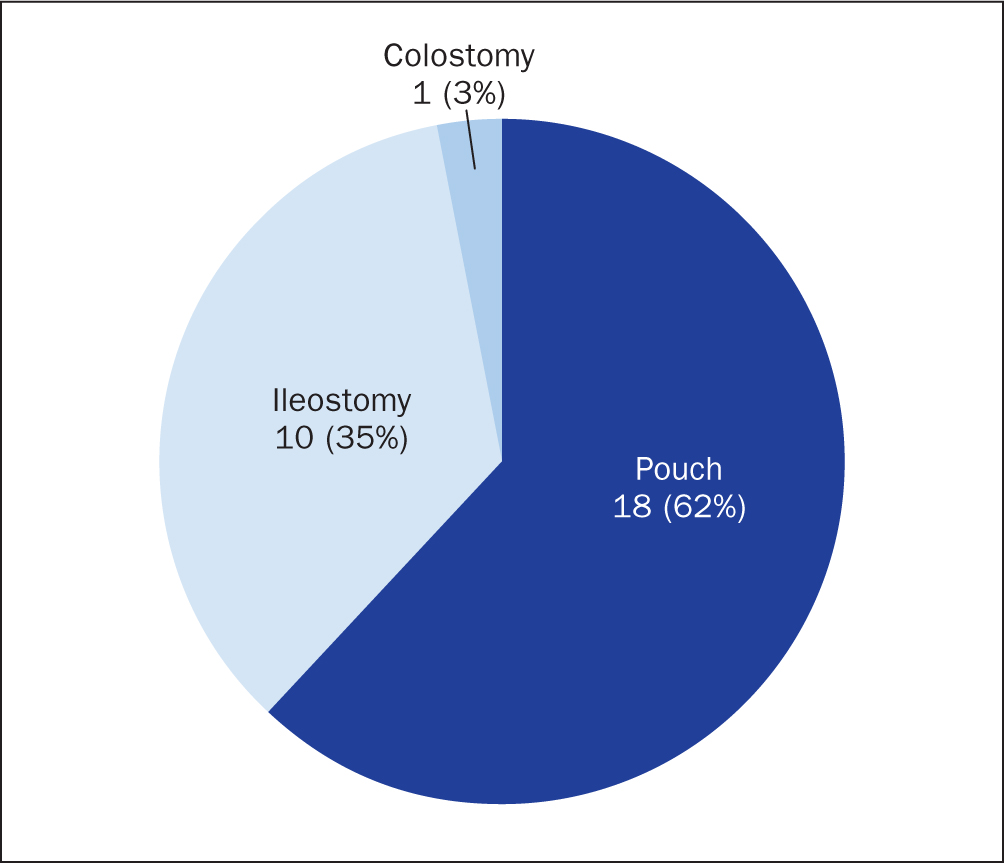
The demographic data showed that, of the 29 participants, 20 (69%) were female and 9 (31%) were male. The mean age across the study group was 54 years. Participants' medical history showed that 18 had an ileoanal pouch, 10 had an ileostomy, and 1 had a colostomy (Figure 2). No participant had any other type of enteric stoma, such as a jejunostomy.
Infection history showed that between 2020 and 2024 participants contracted COVID-19, with 9 (31%) reporting that they had had multiple coronavirus infections over the preceding 4 years.
Most participants did not report having chronic inflammation of the pouch or stoma. However, 6 of the 18 patients with a pouch had a history of chronic inflammation of the pouch (pouchitis) and high output, and 5 of the 10 with an ileostomy also had a history of high-output stomas.
In addition, 15 of the 18 pouch patients reported having GI symptoms when they had COVID-19, while the remaining 3 patients did not report having symptoms. Of the 15 who had GI symptoms, 5 had a history of chronic pouchitis and/or high-output pouch, while of the 3 who did not report GI symptoms, 1 had a history of chronic pouchitis and/or high-output pouch.
In contrast, 8 out 11 (78%) stoma patients (ileostomies and colostomies combined) had GI symptoms when they had COVID-19, while 3 did not report any GI symptoms. Of those who reported GI symptoms, 5 had a history of high-output stomas, while of those who did not report symptoms, none had a history of high-output stoma and one had a colostomy.
A common thread of GI symptoms was identified, including:
In addition, one patient with a pouch vaginal fistula reported that the fistula became very active during coronavirus infection after which symptoms had subsided. Similar symptoms were reported by patients with a defunctioned ileoanal pouch or rectal remnant and a stoma, where mucus discharge from the rectum or pouch was increased during coronavirus infection after which symptoms subsided.
One pouch patient reported reduced output, constipation, evacuation difficulties, and needing to use osmotic laxatives for the duration of the infection. Another pouch patient was treated for rectal cuff inflammation (cuffitis) after being diagnosed with cuffitis post-COVID-19.
Most patients who had GI symptoms reported that these started with the onset of COVID-19, but not prior to testing positive. Out of the 23 patients who reported having GI symptoms, 18 reported symptoms that had appeared along with COVID-19 symptoms and continued for the entire duration of the disease, lasting an average of 2-4 weeks post-COVID-19. However, some patients had symptoms lasting 3-6 months. The remaining 5 of the 23 patients with GI symptoms reported that their symptoms started 5-7 days prior to testing positive for coronavirus.
Only 5 of the 29 participants who had COVID-19 had sought advice from a health professional, and the remaining patients had either self-medicated or not needed treatment. However, 1 patient needed to be admitted to hospital with severe respiratory distress: this was early in the COVID-19 pandemic, at a point when vaccines were not available. However, most patients did not require prescription medication, such as antibiotics, and needed only over-the-counter medication, such as paracetamol, antacids and antispasmodic treatments.
However, 4 of the 6 ileoanal pouch patients with a history of chronic pouchitis had taken antibiotics to treat their GI symptoms, while 1 ileostomy patient had had to go to a hospital to have an intravenous fluid infusion.
Finally, of the final 29 participants who completed the survey 26 (90%) had had a COVID-19 vaccination at the time of infection, and 3 (10%) had not because they had had COVID-19 early on at a point before vaccines were available.
Limitations
The main limitation of the study was the small number of participants. Nonetheless, it is important to highlight that stoma and ileoanal pouch patients do not constitute a very large group; therefore the authors consider this to be a significant cohort of pouch and stoma patients, with a good response rate. It allowed the authors to obtain valuable information, providing the basis for potential future research on the topic.
Analysis and discussion
The authors' findings have shown that the majority of patients without a functioning large intestine (colon) – ileoanal pouch and ileostomy patients – had GI symptoms associated with being ill with COVID-19. The patient who had retained most of their large intestine, and had a colostomy, did not report any GI symptoms. However, it is important to highlight that there was only one participant with a colostomy, so it is likely that some colostomy patients may have reported GI symptoms associated with being ill with COVID-19. Furthermore, it should be noted that patients with colostomies, and who have a significant length of functioning large intestine, are less likely to experience severe electrolyte and fluid losses; consequently, their GI symptoms may be less noticeable.
Because two-thirds of the ileoanal pouch patients with a history of chronic pouchitis took antibiotics to treat their GI symptoms, it may be assumed that some of them may have treated their symptoms inappropriately with antibiotics. This is because their COVID-19 GI symptoms would have mimicked pouchitis symptoms, and they would have been prescribed or already had antibiotics to treat pouchitis at home from a previous prescription, not realising that these symptoms were due to being ill with COVID-19 and not true pouchitis.
Even if antibiotics had been prescribed by a clinician, this would most likely have been inappropriate – based on the assumption that the patient had pouchitis, rather than considering that the patient had COVID-19.
The patients without a history of chronic pouchitis had their symptoms subside spontaneously without antibiotics, which may suggest that the chronic pouchitis patients had taken antibiotics inappropriately simply because their COVID-19-related GI symptoms had mimicked pouchitis. However, it could also be hypothesised that those with a history of chronic inflammation or pouchitis may be more susceptible when they have COVID-19 and they may need antibiotics due to having a secondary infection; secondary infections post-COVID-19 have been reported since the beginning of the pandemic, because of a weakened immune system. Furthermore, research suggests that the risks of secondary infections arising from COVID-19 increase with subsequent coronavirus infections as immune dysfunction increases (Fazel et al, 2023).
It is also plausible that patients with high-output stomas or ileoanal pouches, or those with chronic pouchitis and high frequency, may not be able to notice marked changes in GI symptoms during a coronavirus infection, because they are already used to having similar GI symptoms due to poor function. Thus, it is reasonable to assume that some of the patients may have had some degree of GI symptoms while they were infected with coronavirus, but that these symptoms were not considered as such, because they did not present a great deviation from the patient's daily health status.
Some patients with chronic pouchitis or high output reported prolonged recovery from COVID-19, with some reporting that it took 3-6 months. These findings may be due to a weakened immune system, which would inevitably make patients more susceptible to inflammation.
Patients with a defunctioned ileoanal pouch or rectum reported increased mucus discharge from their pouch or rectum. These findings are consistent with inflammatory processes due to COVID-19, as the coronavirus uses the angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2) to attack the host's cells. ACE2 and TMPRSS2 are expressed in many different organs in the human body, including the intestine luminal cells (Alberca et al, 2021). The authors observed similar findings with patients with pouch fistulae, with secretions increasing during coronavirus infection, which is likely due to the ongoing inflammatory processes.
Another important consideration is the fact that almost all participants (90%) were vaccinated at the time of having COVID-19, which may have resulted in less severe symptoms. The literature suggests that symptoms of COVID-19 may be less common in vaccinated patients compared with unvaccinated patients, as well as the fact that individuals who have been vaccinated are more likely to be completely asymptomatic compared with unvaccinated patients (Antonelli et al, 2022).
Conclusion
GI symptoms in patients with a confirmed SARS-CoV-2 infection are more likely in patients with ileostomy and ileoanal pouches compared with the general population (among the general population the figures are 17-50% (Docherty et al, 2020; Luo et al, 2020; Pan et al, 2020) and in the authors' sample of ileostomy and ileoanal pouch patients the rates were 78–83%). It is therefore vital that both health professionals and patients are well informed about this, to ensure appropriate treatment and care is provided. In addition, because the first point of contact for these patients is often their stoma or pouch nurses, it is imperative to highlight the importance of nurse prescribers, with specialist knowledge in their area of practice; this ensures correct assessment and diagnosis, the provision of patient-centred treatment and high-quality management of disease.
Ensuring that the patient is correctly diagnosed with COVID-19 is even more important in ileostomy and ileoanal pouch patients. Incorrect diagnosis may lead to inappropriate treatment, because GI symptoms related to COVID-19 may make pouch or stoma function deteriorate or even mimic pouchitis symptoms in patients with ileoanal pouches and gastroenteritis in patients with a stoma.
Although this is an initial piece of research – and it supports the authors' hypothesis – further research into the effects of COVID-19 and GI symptoms in ileostomy and ileoanal patients would be beneficial to better understand disease progression and the most appropriate approach to treatment. One approach to repeating the study would be to undertake the research as a randomised trial involving a greater number of pouch and stoma patients, and preferably involving endoscopic investigations and analysis of stool samples to exclude underlying pouchitis or enteritis. This would enable further comparison of the similarities between patients with GI symptoms related to COVID-19 and those who have pouchitis or gastroenteritis.
In conclusion, COVID-19, caused by the SARS-CoV-2 virus, remains a significant global health concern even years after the peak of the pandemic. The ongoing impact of the virus is particularly pronounced in vulnerable populations, such as those with stomas or ileoanal pouches, who face unique health challenges. This is why it is fundamental that health professionals continue to practise vigilance and implement tailored healthcare strategies to support these susceptible patients, ensuring they receive the specialist care they need.


