Delirium is a form of acute brain dysfunction that affects up to 80% of patients admitted to an intensive care unit (ICU) (Pun and Boehm, 2011; Faria and Moreno, 2013; Porter and McClure, 2013). It is associated with an increased morbidity and mortality of critically ill patients and affects up to 50% of elderly hospitalised patients (Inouye et, 2014). The condition is characterised by acute alteration in cognition that develops within hours or days of hospitalisation and manifests in fluctuations of consciousness, attention, memory, thinking, perception and behavioural disorders (American Psychiatric Association, 2013). The subtypes of delirium and their signs and symptoms are shown in Table 1.
Table 1. The three subtypes of delirium and their signs/symptoms
| Hyperactive |
|
| Hypoactive |
|
| Mixed |
|
The pathophysiological mechanism of delirium is not yet understood and its aetiology is multifactorial in nature. One hypothesis points to interactions between neurotransmitter systems, with inflammatory processes and even with stress (Mantz et al, 2010). Table 2 summarises the risk factors for developing delirium in the critically ill patient (Barr et al, 2013; Faria and Moreno, 2013).
Table 2. Risk factors for development of delirium
|
The occurrence of delirium is associated with the critical state of a patient in ICU; it increases the discomfort and insecurity of the patient and requires the nurse to be more vigilant about the condition of the patient. Thus, the predictive value of delirium for complications and prognosis is evident (Dubois et al, 2001). The complications and prognosis related to delirium are listed in Table 3.
Table 3. Complications and prognosis related to delirium
|
The negative impact that an episode of delirium has on a patient in critical care indicates the need for research and action in clinical contexts, especially in preventing its occurrence. Of the ICU healthcare team, nurses are most closely involved in monitoring patients, so they are in a prime position to help identify patients at risk of delirium and to take preventive action when they detect that a patient is at risk of acute cognitive alteration.
This review aims to inform the planning of nursing care in the face of delirium in adult/elderly intensive care by guiding evidence-based clinical practice.
Objective
Identify possible nursing interventions that can be taken to prevent or manage delirium in adult patients in ICU.
Method
A scoping review was conducted based on the principles recommended by the Joanna Briggs Institute (2015).The authors started with the following research question: What nursing interventions in the scientific evidence are focused on the management of delirium in adult patients in intensive care?
Studies involving adults aged 18 years and older were included in the search. Although legal adult age varies between countries and regions, the starting point for this study was Hockenberry and Wilson's (2014) definition of 18–20 years characterising late adolescence.
Studies on nursing interventions were considered to be relevant. In 1996, the Nursing Intervention Classification (NIC) defined a nursing intervention as any treatment based on clinical judgement and knowledge that nurses use to improve patient outcomes (McCloskey and Bulechek, 1996). Studies that addressed the development of delirium during the stay of an adult in ICU were also considered. The search included qualitative and quantitative studies published in Portuguese, English and Spanish (as languages familiar to the authors), primary and secondary studies, which were undertaken within a 5-year period (2013-2018).
Once the relevant studies had been identified, the next stage of selection involved applying the Portuguese DeCS and English MeSH descriptors in order to use unique terminology for selection. The descriptors adopted for the search applied Boolean operators, and included searching for: delirium AND critical care AND critical care nursing NOT children NOT neonatal NOT pediatric.
The search was conducted in September 2018, using the search engine EBSCOhost. The following databases were searched: CINAHL, the Nursing and Allied Health Collection, Cochrane Plus Collection, MedicLatina, Medline, Pubmed, Scielo (Scientific Electronic Library Online), Portal regional da BVS [Bibloteca Virtual em Saúde], and RCAAP [Repositórios Científicos de Acesso Aberto de Portugal]. The selection process was initially carried out by scanning titles and abstracts, and then by a full reading of articles. Studies published in other languages or without the participation of nurses were excluded.
The survey identified 185 potential articles. Of these, 136 were excluded after evaluating the title and abstract. Of the remaining 49, a further 42 were excluded because they did not meet the inclusion criteria after reading the full text. The final sample was seven article. Figure 1 outlines the selection process.
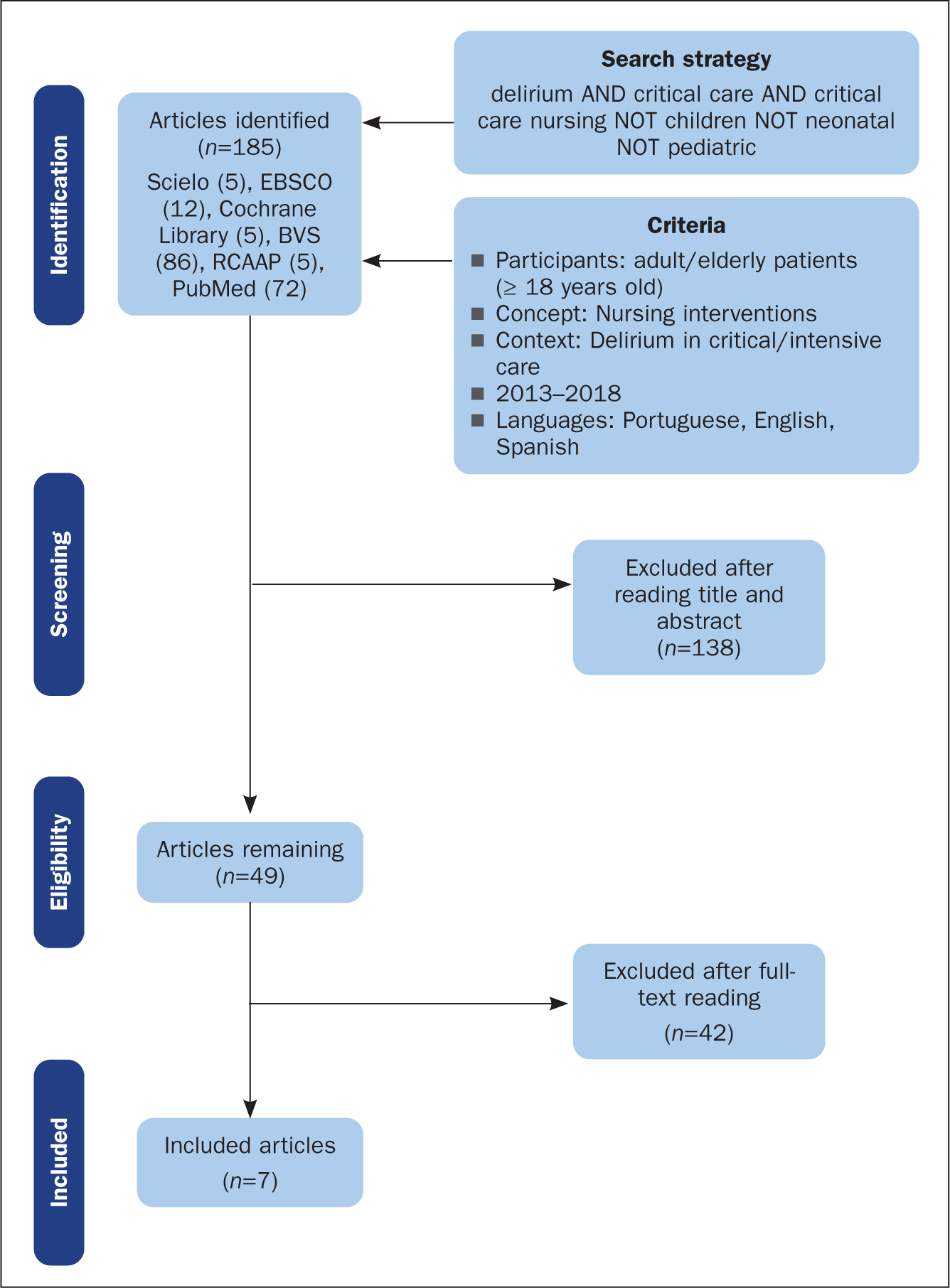 Figure 1. Flowchart of the literature review
Figure 1. Flowchart of the literature review
Results
To facilitate the dynamics of the research and mapping of the seven selected articles, Table 3 was collated to summarise the details of the articles and the nursing interventions they discuss.
Table 3. Articles included in the scoping review and identified interventions
| Article titles | Authors (year) Country | Nursing interventions |
|---|---|---|
| Nursing and patients with delirium: a literature review | Henao-Castaño and Amaya-Rey (2014) Colombia |
|
| Non-pharmacological measures for the treatment of acute confusional syndrome in the intensive care unit | Cachón-Pérez et al (2014) Spain |
|
| Nonpharmacological interventions to prevent delirium: an evidence-based systematic review | Rivosecchi et al (2015) London |
|
| Pharmacological interventions for delirium in intensive care patients: a protocol for an overview of reviews | Barbateskovic et al (2016) Denmark |
|
| The effect of nonpharmacological training on delirium identification and intervention strategies of intensive care nurses | Birge and Aydin (2017) Turkey |
|
| A family intervention to reduce delirium in hospitalised ICU patients: a feasibility randomised controlled trial | Mitchell et al (2017) Australia |
|
| Delirium prevention in critically ill adults through an automated reorientation intervention—a pilot randomized controlled trial | Munro et al (2017) USA |
|
Discussion
Of the seven articles included that fulfilled the objective of identifying nursing interventions aimed at addressing delirium in adult/older patients in ICU, four originated in Europe (Cachón-Pérez et al, 2014; Rivosecchi et al, 2015; Barbateskovic et al, 2016; Birge and Aydin, 2017), none of which were Portuguese.
Regarding methodologies, three were literature reviews (Henao-Castaño and Amaya-Rey, 2014; Rivosecchi et al, 2015; Barbateskovic et al, 2016), one was a qualitative phenomenological study that looked at nurses' experiences of using non-pharmacological interventions for delirium in ICU (Cachón-Pérez et al, 2014), two were randomised controlled studies (Mitchell et al, 2017; Munro et al, 2017), and one was a quasi-experimental study (Birge and Aydin, 2017). The methodologies used in these studies underline the need for more qualitative studies to be carried out, namely phenomenological studies, to evaluate the nursing experience in managing delirium and identifying patient needs that, ultimately, lead the quality of care to be improved.
Although the research strategy covered a 5-year time span the oldest study (Cachón-Pérez et al, 2014) included in the review was published 4 years ago. This aspect may represent a growing concern about delirium in ICU and, consequently, more interest in research by nurses on its incidence and management in ICU in critically ill patients.
The findings of these articles suggest that the nursing interventions employed meet the 2013 clinical practice guidelines for pain, agitation and delirium (Barr et al, 2013)— and the ABCDEF bundle (Marra et al, 2017), which succeeded the guidelines—are available in the literature to guide clinical practice in preventing and managing delirium. The ABCDEF bundle focuses mainly on the prevention of delirium (Marra et al, 2017), and specifically refers to:
- A Assessment, prevention, and management of pain
- B Awakening the patient and spontaneous breathing training
- C The selection of sedation and analgesia
- D Assessment, prevention, and management of delirium
- E Early mobilisation
- F Family involvement.
Rivosecchi et al (2015) referred to the benefits of non-pharmacological interventions for the prevention or treatment of known risk factors for delirium in ICU. Their findings were similar to those of Faria and Moreno (2013) because they both focus on the prevention of delirium by addressing modifiable risk factors, with the ICU environment itself cited as a factor. Similarly, Cachón-Pérez et al (2014) identified the control of ICU environments as necessary, namely reducing noise levels, exposure to artificial light and minimising these and other potentially stressful stimuli.
Another aspect related to the need to control the ICU environment mentioned by the authors above (Cachón-Pérez et al, 2014; Rivosecchi et al, 2015) was the need to identify the promotion of the routine sleep-wake cycle as a nursing intervention to help prevent delirium. Rivosecchi et al (2015) suggested the modification of the care routine, with essential care tasks grouped together to provide time for patients to rest.
The regular reorientation of a patient to current date, time and place is one nursing intervention mentioned that can help prevent delirium (Rivosecchi et al, 2015; Mitchell et al, 2017). Henao-Castaño and Amaya-Rey (2014) recommended that this activity should be performed at least once a shift.
With regard to cognitive stimulation, it is recommended that it is performed several times a day through nursing tasks (Henao-Castaño and Amaya-Rey, 2014). These tasks are identified as nursing interventions that promote cognitive stimulation, recording information in the patient care plan and clinical status (ie health status, tests ordered and test results), and talking to the patient in a way that requires memory recall (Rivosecchi et al, 2015). Cognitive and memory stimulation was undertaken by family members and nurses through visualisation using family photographs, discussing family life and reminiscing about events (Mitchell et al, 2017).
Another nursing intervention identified is the reduction of sensory deficits. For example, it is important that nurses identify which patients habitually wear glasses and hearing aids, and encourage nurses to help patients wear them during their hospital stay (Henao-Castaño and Amaya-Rey, 2014). Families can also be involved in this (Mitchell et al, 2017).
The removal of catheters, probes and physical restrictions as soon as possible were also identified as positive nursing interventions, highlighting the need to develop protocols for such interventions and in addition protocols for pain control (Cachón-Pérez et al, 2014). Early mobilisation should also be promoted by nurses. In some cases, it may only be possible to help patients make passive movements with a limited range of motion, while other patients can be encouraged to be more active themselves. The type of mobilisation should be decided by the multidisciplinary team on a patient by patient basis to ensure that it is in accordance with each clinical situation (Rivosecchi et al, 2015).
The integration of families in the care of critically ill patients to prevent delirium was identified in three articles, as already cited in their involvement in reorientation and cognitive stimulation activities. Cachón-Pérez et al (2014) also referred to the need for individual adjustment of visiting hours, according to the needs of individual patients and their families.
Only one study (Barbateskovic et al, 2016) referred to the use of pharmacological measures. This study was a systematic review that examined the findings reported in randomised clinical trials on the effects of drugs used in the management of delirium. The results of this review are not conclusive, which could be due to the fact that the pathophysiological mechanism of delirium is not yet understood (Mantz et al, 2010). However, the review brought together information on the benefits of some drugs used in the treatment of hyperactive delirium over others. With respect to sedative and analgesic drugs, as suggested in the ABCDEF bundle (Marra et al, 2017), clinical trials have found that the administration of dexmedetomidine has more benefits compared with the use of lorazepam and midazolam—it results in fewer delirium episodes and patients require mechanical ventilation for shorter duration (Barbateskovic et al, 2016).
In the Portuguese context, drug administration represents an interdependent nursing intervention that implies vigilance, knowledge about how specific drugs affect the patient's condition, and the actions required to manage the condition (Decree-Law no. 161/96, of 4 September, amended by Decree-Law no. 104/98, of 21 April, regulating Nurses' Professional Exercise Regulations).
Drug administration, as an intervention for treating delirium, appears to be associated with significant agitation and an associated risk of physical injury (Barbateskovic et al, 2016).
Limitations
The review included only research articles published in Portuguese, English and Spanish because these are the languages familiar to the authors. Articles published in other languages may have been relevant.
In this review, no recommendations for clinical practice are presented because a scoping review does not assess the methodological quality of the included studies, but rather maps out the evidence for use in clinical practice and identifies gaps in the topic. An identified gap points to the need for the training of nurses and other professionals working in ICU with regard to the identification and management of delirium (Cachón-Pérez et al, 2014; Birge and Aydin, 2017). Faria and Moreno (2013) mentioned that delirium in ICUs has only recently become a focus for research, which may explain this lack of information in the literature.
Given the negative impact that a delirium episode can have on the hospitalised patient, further quantitative and qualitative studies on preventing delirium during a stay in ICU are recommended for future research. It is also vital that the education of health professionals working in ICU includes the identification and prevention of delirium.
Conclusion
It was possible to identify the different categories of nursing interventions to manage delirium in adults/older patients in intensive care, namely pharmacological and non-pharmacological treatments. The interventions were mainly directed towards preventing delirium. Given that nurses are involved in the ongoing monitoring of patients in ICU, they are in a position to assess patients at risk, identify episodes of delirium, and to initiate non-pharmacological measures as preventive or management interventions. They are also in a position to educate their peers and other colleagues in the multidisciplinary team about the risk of delirium and ways it can be managed, as well as involving the families of patients in mitigating the risks of delirium.
KEY POINTS
- Delirium is an acute cognitive change that has a high incidence among critically ill patients
- An episode of delirium is associated with increased critical patient morbidity and mortality
- The pathophysiology of delirium is not yet understood and its aetiology is multifactorial in nature
- The ABCDEF bundle synthesises critical patient care for delirium management
- Nurses in intensive care can be crucial in the prevention and identification of delirium
- Training the clinical team on delirium management is crucial
CPD reflective questions
- After reading this article, do you think that the prevention of delirium is an indicator of quality of care in an intensive care unit?
- In addition to the nursing management of patients, how important is the involvement of the family in the care of the critically ill patient in preventing delirium?
- Reflect on your education and training. Was the identification of delirium episodes in critically ill patients a priority in educating nurses to work within a multidisciplinary team? How could this be addressed?


