Medical device-related pressure ulcers/injuries (MDRPUs/MDRPIs) are caused by external forces that are applied by skin-contacting medical devices (Gefen et al, 2020). A recent systematic review reported that the incidence and prevalence of MDRPUs are 12% and 10%, respectively (Jackson et al, 2019). Hence, MDRPUs are common in the hospital setting and, therefore, create a considerable financial burden, both in terms of direct treatment costs and in the context of litigation since, in many cases, MDRPUs are by definition a hospital-acquired injury.
Similar to the influence of sustained bodyweight forces, cells in the soft tissues under and near medical devices may undergo extreme shape distortions and deformations that result from the forces applied by the device, eventually leading to the loss of biological function of the distorted cells. The loss of cell integrity due to sustained forces, which ultimately causes cell death, can be compared with a building that loses its reinforcing structures such as the foundations, columns and beams. When these reinforcing structures are damaged, the walls or the roof of the building may develop cracks through which rain, hail or snow can penetrate and flood the interior space. Like buildings, living cells contain a reinforcing structure that supports their walls, that is, the cytoskeleton that supports the plasma membrane—the envelope of cells.
The plasma membrane functions not only as the walls, but also as the gatekeeper, controlling all the traffic of molecules and ions into and out of the cell body through specialised mechanisms, much like windows and doors function in a house. When the plasma membrane does not receive sufficient structural reinforcement from a degrading cytoskeleton and the cell is unable to maintain its plasma membrane intact, pores appear on the membrane, through which molecules and ions can move freely. The control mechanisms that cells have on their plasma membrane thereby become ineffective and the affected cells lose their ability to regulate the transport of molecules and ions inwards or outwards. This results in loss of the delicate biological equilibrium of essential molecules and ions such as metabolites and metabolic by-products in the cells or their vicinity, leading to cell death due to the loss of homeostasis, killing the first cells within minutes (Lustig et al, 2021).
This deformation-inflicted cell damage, triggered by the sustained cell deformation exposure, initiates and perpetuates a vicious cycle (Figure 1). Sustained mechanical forces lead to cell deformation and cell death, which in turn causes inflammatory oedema and increased interstitial pressures. The build-up of interstitial pressures due to the inflammatory oedema further distorts the cells, leading to additional loss of cytoskeletal integrity and increased poration of their plasma membranes. At a certain point, the elevated interstitial pressures developing under a medical device may cause obstruction or even occlusion of the vasculature or the lymphatics, which would potentially add ischaemic damage related to hypoxia and acidosis due to increased glycolysis and lactic acid production in the anaerobic environment. In relation to medical devices that constrain a relatively thin mass of soft tissues, such as a continuous positive airway pressure (CPAP) mask that compresses and shears facial skin and underlying soft tissues against the rigid skull surface, tissues have no space for swelling in response to the progressing oedema. If no swelling is possible, the interstitial pressure will rise sharply and instantaneously (Lustig et al, 2021), further escalating the vicious cycle depicted in Figure 1.
Figure 1. The vicious cycle of cell and tissue damage in medical device-related pressure ulcers/injuries, resulting from sustained soft tissue deformations, which are the triggering event for this cycle
The latter example, of a CPAP mask, is highly relevant in the context of the COVID-19 pandemic, which has dramatically increased the use of this non-invasive ventilation method as a first-line treatment for patients presenting with breathing difficulties. In this regard, the aetiology of COVID-19 strongly interacts with the vicious cycle of MDRPUs in several aspects (Gefen and Ousey, 2020; Lustig et al, 2021). First, the systemic cytokine storm in patients with serious COVID-19 illness causes their inflammatory system to become less sensitive to molecular signalling from a local source of a forming MDRPU, which allows cell deformation-inflicted damage to progress unnoticed by the inflammatory system until massive cell death has already occurred. Second, once the cell death has been detected by the inflammatory system, the endothelial dysfunction in such seriously ill patients makes them more susceptible to inflammatory oedema. The extent and spread of the oedema (and the associated inflammatory damage) thereby becomes more severe. Third, the increased tendency of these patients to clotting and thrombosis contributes to decreased tissue perfusion and oxygenation. Hence, all these COVID-19-related factors combine to fuel the vicious cycle of MDRPUs (Figure 1) (Gefen and Ousey, 2020; Lustig et al, 2021).
A number of factors are unique to the aetiology of MDRPUs (with respect to general pressure ulcer aetiology) and contribute to the formation of an injury (Gefen et al, 2020):
- Many skin-contacting materials in medical devices are considerably stiffer than native skin and underlying soft tissues (Bader et al, 2019)
- Some devices such as CPAP masks require securing on the body by applying forces (such as via the tension in the straps of a CPAP mask which is applied to prevent air leakage)
- Devices that should theoretically fit the contours of the body are made in uniform shapes and sizes, with the consequence that ideal fitting to an individual patient's body surfaces may never occur
- Devices, such as invasive and non-invasive ventilation equipment, act in a hot and humid environment (CPAP masks again being a good example), which compromises the tolerance of the skin to the applied loads and potentially increases frictional forces on the skin (Schwartz et al, 2018)
- It is also difficult to assess the skin under medical devices without detaching or moving the device (which compromises its function)
- Finally, as with bodyweight-related pressure ulcers, there is sometimes a lack of awareness of the need to remove or reposition medical devices, and the necessity to continue to provide routine skin assessments and care under the devices.
Determining tissue loading states under medical devices: the key to prevention
The aetiology of MDRPUs is exemplified here through two common clinical scenarios—of a CPAP mask that is being used extensively in the current COVID-19 pandemic (Figure 2), and of a doughnut-shaped head positioner applied to ‘protect’ surgical patients and, sometimes, bedridden individuals who receive intensive care in a supine position (Figure 2). These two medical devices cause intense, localised mechanical stresses (forces per unit area of tissue) to the facial skin, particularly at the nasal bridge and underlying tissues for the CPAP scenario, and to the occipital scalp for the doughnut-shaped positioner case (Figure 2). In both cases, the affected soft tissues cannot swell in response to the expected inflammatory oedema (Figure 1), as the tissues are sandwiched between the device and the skull. Accordingly, the two devices result in characteristic and common MDRPUs that are avoidable through appropriate prophylactic interventions. Suitable preventive measures are to use preventive dressings under the CPAP mask and to replace the doughnut-shaped head support device by a more advanced, shape-conforming, soft support aid to alleviate the elevated tissue stresses.
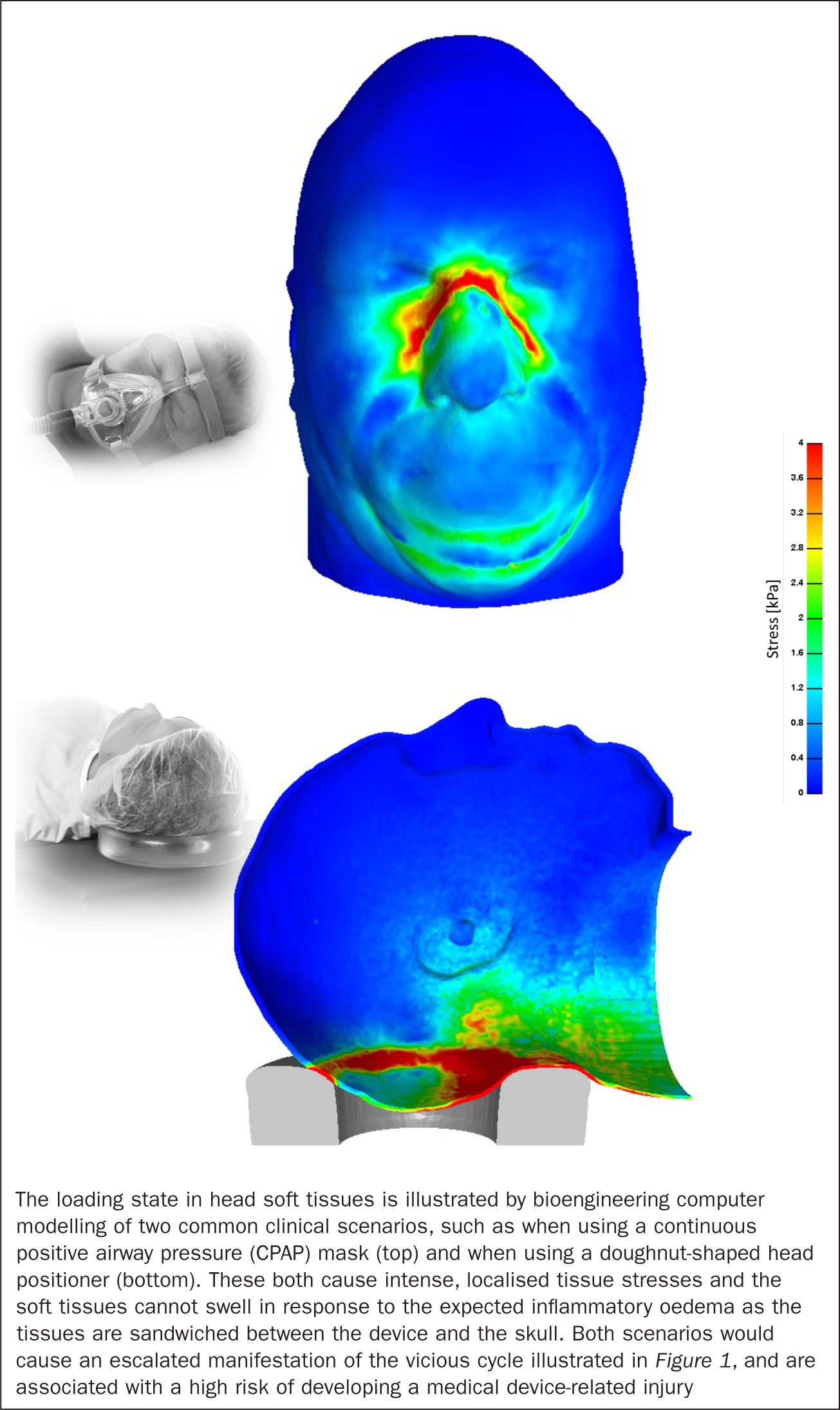 Figure 2. Computer reconstruction of the state of tissue stresses when using a continuous positive airway pressure mask and a doughnut-shaped head positioner
Figure 2. Computer reconstruction of the state of tissue stresses when using a continuous positive airway pressure mask and a doughnut-shaped head positioner
To determine the loading state of the nasal bridge under a CPAP mask and how tissue stresses there may be alleviated and dispersed using dressing cuts applied prophylactically (Mepilex® Lite, Mölnlycke Health Care, Gothenburg, Sweden), the author's research group has developed a bespoke force measurement system that is able to measure the compressive contact forces between the CPAP mask and the nasal bridge (Peko Cohen et al, 2019). Using an anatomically realistic computer model of the head of an adult male, the measured compressive forces were delivered to the nasal bridge to form the computer reconstruction of the state of tissue stresses (with the aforementioned dressings versus without them). The above dressings have shown substantial biomechanical effectiveness in alleviating facial soft tissue loads, by providing localised cushioning to the tissues at risk (Peko Cohen et al, 2019).
To investigate the effects of a doughnut-shaped gel head positioner on the occipital scalp tissues, the author's research group has similarly used an adult head model, to which the above head support has been added (Figure 2). The occurrence of scalp tissue stresses while the doughnut-shaped gel head support was in use was compared with the tissue stress state associated with a fluidised head positioner, which is moulded to mirror the shape of the head of the individual and maintains that specific shape (Z-Flo®, Mölnlycke Health Care, Gothenburg, Sweden). The scalp stress state was further calculated for a baseline condition with respect to the application of both positioner types; the baseline condition was the head resting on a flat, regular medical foam cushion (Katzengold and Gefen, 2019). The doughnut-shaped gel head support inflicted the greatest exposure to tissue mechanical stresses, particularly to the high and, therefore, hazardous stress domain, when compared with the other positioners. It was concluded that, while the doughnut-shaped gel head support is designed to divert tissue loads away from the occiput, in practice, it fails to do so (Figure 2). Rather than spreading the tissue loads, the doughnut-shaped head support actually causes the head-weight forces to focus and transfer through a relatively narrow ring of scalp tissues, which results in elevated localised and sustained tissue stresses along that ring (Figure 2). This phenomenon, of focal occipital tissue stresses along the ring, eventually causes the typical MDRPUs seen in this clinical scenario, ie those that have the contours of the gel doughnut-shaped support (Katzengold and Gefen, 2019). The fluidised head positioner resulted in the lowest scalp stress levels through the optimal, patient-specific envelopment that it provides to the back of the head (Katzengold and Gefen, 2019).
Clinical relevance and conclusions
Bioengineering research, such as the computer modelling work demonstrated in Figure 2, is vital for understanding the aetiology of MDRPUs and, in particular, for targeting and focusing effective clinical interventions, as confirmed through clinical trials.
A number of studies reported that padding CPAP masks with foam dressings reduces the incidence of MDRPUs associated with these devices, as reported in a World Union of Wound Healing Societies consensus document (Black et al, 2016). For example, a study in an acute care setting in Taiwan demonstrated that implementation of the practice of using Mepilex foam dressing technology under CPAP masks lowered the incidence of pressure ulcers from 5.90% to 0.90% (Hsu et al, 2010). The same group of clinicians later reported that, among a group of patients hospitalised in a respiratory ward (n=30), the incidence of MDRPUs associated with ventilation devices was brought down to zero in patients who received care using the above foam dressings (0/13) compared with approximately 18% (2/11) in the control (no dressing) group (Hsu et al, 2011).
Related to these findings, Boesch et al (2012) subsequently reported a decrease in the incidence of MDRPUs associated with tracheostomy tube flanges in children, from a baseline of 8.1% to 3.4%, after the introduction of a bundled change programme including education and application of Mepilex Lite dressings under these devices. These and other work have led a panel of clinical experts to state that ‘the attributes of foam dressings would appear to have benefit in these patients by reducing pressure and absorbing moisture, where hydrocolloids and films cannot absorb moisture’ (Black et al, 2015).
With respect to preventing MDRPUs associated with the use of doughnut-shaped head positioners, the author and clinical collaborators recently reported a post-test design with a historical control group in an intensive care unit (Barakat-Johnson et al, 2019). Patients in that setting who participated in the study received extracorporeal membrane oxygenation, were mechanically ventilated or had raised intracranial pressures. The intervention consisted of the aforementioned fluidised positioner device that maximises the envelopment of the occipital region under the head of each patient (Katzengold and Gefen, 2019), and routine skin assessments (every 8 hours). Outcome measures included the occurrence of occipital pressure ulcers among the patients who received the above interventions (n=64), with respect to the rate of injuries reported in the health records of the historical controls (n=63). The results of this work showed a statistically significant reduction in the occurrence of occipital pressure ulcers, by approximately 88% (2/64 patients in the interventional group versus 16/63 in the historical controls) (Barakat-Johnson et al, 2019).
Direct links and strong associations between laboratory bioengineering evaluations and clinical trials have proved to be highly effective and powerful in the context of preventing MDRPUs. This had been demonstrated not only with regards to understanding the fundamental causes of the problem (for example, in identifying that the doughnut-shaped head positioner does not reduce scalp tissue exposure to loads but, on the contrary, intensifies the occipital tissue loading), but also in directing solutions to these clinical problems. It is well established that correct aetiological understanding leads to effective technological and clinical interventions. Accordingly, since the heart of the matter of MDRPUs is soft tissue exposure to sustained mechanical loading, alleviating the tissue stress exposures as per the above examples has already led to considerably better clinical outcomes, improved quality of life for patients and a substantial reduction in treatment costs.
KEY POINTS
- Pressure ulcers are localised soft tissue damage sites caused as a result of continuous tissue exposure to sustained mechanical forces, such as bodyweight or an interfacing object
- The latter pressure ulcer type is a specific sub-class of injuries termed ‘medical device-related pressure ulcers’ (MDRPUs), where the injury has been caused by a medical device applied for a diagnostic or therapeutic purpose
- Aetiological research has established three key contributors to the formation of MDRPUs: direct cell and tissue deformation, inflammatory oedema and ischaemic damage, which typically act sequentially to escalate the injury process
- Bioengineering computer modelling is essential for understanding the aetiology of MDRPUs and for targeting and focusing effective clinical interventions to reduce the injury risk
- This article summarises the aetiology of MDRPUs and depicts the role of computer modelling in identifying and evaluating protective means for the prevention of MDRPUs
CPD reflective questions
- What are the three important aetiological damage factors in the formation of medical device-related pressure ulcers (MDRPUs)?
- Which aetiological factors are unique to the aetiology of MDRPUs with respect to the general pressure ulcer aetiology that is known to date?
- How do COVID-19-related pathophysiological factors fuel the vicious cycle of MDRPUs?
- Think about how your area of practice approaches the problem of MDRPUs and the evidence base used for prevention. Could practice be improved? What steps could you take to achieve this?


