The annual cost to the NHS of managing 3.8 million patients with a wound was estimated in 2020 to be £8.3 billion, of which £5.6 billion was spent on the 30% of wounds that did not heal and £2.7 billion on the 70% of wounds that healed (Guest, 2020).
One of the main symptoms associated with chronic ‘hard-to-heal’ wounds, defined as wounds that ‘do not close after care for up to a year or more’, is the production of excess exudate (Atkin et al, 2019). This is due to a prolonged chronic inflammatory response stimulated by a physiological cause, as occurs in malignant fungating wounds (Bernardes et al, 2021), and diabetic foot, venous and category 4 pressure ulcers (Atkin et al, 2019).
However, since there has been a 46% decrease in district nurses since 2010 (Queen's Nursing Institute, Royal College of Nursing, 2019), clinicians' knowledge of how to manage heavily exuding wounds may vary across the UK, consequently leaving patients to receive variable care that may impact on anticipated health outcomes and patients' quality of life (Edwards, 2013).
What is exudate?
In clinical settings, in the experience of this author and others (World Union of Wound Healing Societies (WUWHS), 2019), exudate is often referred to as ‘wound fluid’ or ‘wound drainage’. More correctly, it can be described as consisting of fluid that has leaked out of blood vessels that closely resembles the appearance of blood plasma (WUWHS, 2019). Exudate production forms part of the normal wound healing process and can be beneficial to healing by:
- Maintaining a moist wound healing environment
- Carrying tissue-repairing cells and essential nutrients
- Enabling autolytic debridement of the wound bed (natural removal of dead or devitalised tissue) – acute wounds
However, when in the wrong amount, in the wrong place, or of the wrong composition, exudate can delay healing and cause complications (WUWHS, 2019) – chronic wounds.
The main constituents of wound exudate are water (a medium for other components; prevents the wound from drying out); nutrients (promote cell health; eg glucose – cellular energy source); white blood cells (growth factor production/immune defence/reduction of bioburden within wound margins); proteases (degradation of proteins/assists autolysis and cellular migration); protease inhibitors; cytokines and growth factors (stimulate cellular growth) (adapted from WUWHS, 2019).
The main role of wound exudate is to facilitate the diffusion of vital healing factors (eg growth and immune factors) and the migration of cells across the wound bed during the wound healing process (Thomas, 1997; WUWHS, 2019).
Evidence of the presence and importance of wound exudate has been previously reported in the literature as being beneficial for the wound healing process, as follows:
- The benefits of moist wound healing were identified by Winter (1962) as improved healing rates, reduced pain/discomfort, and a decreased risk of infection
- According to consensus published by an international panel of experts (Expert Working Group/Satellite Expert Working Group, 2008): ‘Although a moist environment is necessary for optimal wound healing, conditions of extreme wetness or dryness may adversely affect (delay) healing’
- Providing a moist wound environment increased the formation of granulation tissue formation and increased epithelial migration, as reported by Dowsett (2013).
The overall aims of wound/exudate management are therefore to:
- Optimise the patient's wound healing environment and
- To stimulate a regenerative process, namely the replacement of dead cells by living cells (superficial wounds) or a repair process (with need characterised by tissue loss) that requires an extended time period before wound closure, due to the requirement of the synthesis of several tissue types (as seen in deep wounds) (Collier, 2023a).
Poorly managed wound exudate
Appropriate management of wound exudate should be a primary management aim for all clincians when relevant. It has been widely reported that, if poorly managed, the presence of excess exudate can have significant negative effects on a patient's health-related quality of life (HRQoL), such as increased stress and inconvenience, due to the need for increased dressing changes (Edwards, 2013).
Persoon et al (2004) reported that, when a patient has a wound that is leaking, they can experience psychological challenges, such as embarrassment and loss of dignity, which can lead to patients trying to hide their wounds under oversized clothes and in footwear. Embarrassment can also be the result of an exuding wound leaking through clothing, and lead to poor HRQoL for a patient (Wounds UK, 2013; Beldon, 2016) (see Box 1).
Box 1.The effects of exudate on a patient's wellbeing
Leakage
| Clinical consequences | Psychological consequences | |
|---|---|---|
| Too much exudate |
|
|
| Not enough exudate |
|
NB In wounds with low exudate production, adherence of dressings to the wound bed may cause damage to the wound bed and pain during dressing removal (Collier and Hollinworth, 2000)
Assessing a wound and associated exudate
A systematic wound assessment model is required to assess all wounds, levels and colour of exudate, as well as the surrounding skin (Flannagan, 2013; Collier, 2023a). All wound assessments should be fully documented to provide a baseline for subsequent reassessment and documentation of the wound, as clinically indicated (Collier, 2023b).
In the experience of this author and others (Hindhede and Meuleneire, 2012; WUWHS, 2019), when clinically indicated, the management of a wound producing ‘excess’ exudate is one of the main primary aims for managing that wound. However, it is, and has previously been, acknowledged that determining and classifying exudate levels in an objective and meaningful way is difficult, unless the use of a collection device is incorporated into the dressing regimen, such as with some negative pressure wound therapy (NPWT) systems.
Various approaches have been proposed to assess exudate levels produced from a wound, but these are generally accepted as being subjective, and they vary in complexity and ease of use – consequently, no single approach is ideal (Iizaka et al, 2011). However, the Expert Working Group that developed the WUWHS Exudate Consensus Document (2019) expressed a preference for Falanga's Wound Exudate Score (Falanaga, 2000) (Table 1).
Table 1. Assessment of wound exudate production
| Wound exudate score | Extent of control | Exudate amount | Dressing requirement | |
|---|---|---|---|---|
| Wound exudate score | 1 | Full | None/minimal | No absorbent dressing required. Dressing changes should be no more than twice a week, unless otherwise clinically indicated |
| 2 | Partial | Minimal amount | Dressing changes indicated every 2 days | |
| 3 | Uncontrolled | Very educative wound | Absorptive dressings required daily |
Fortunately, a number of modern wound management products whose composition includes superabsorbent polymers (SAP) have been developed to help clincians manage a patient's wound exudate effectively. One of these products is DryMax Super.
Many absorbent materials used in non-occlusive permeable dressings allow the moisture to be absorbed and then evaporate into the atmosphere. This property has been quantified as the moisture vapour transferability rate (MVTR) (Expert working group/Satellite Expert Working Groug, 2008). However, it should be noted that this characteristic is not strictly relevant to the action of a superabsorbent product, because these products have been designed to retain large amounts of moisture rather than to facilitate evaporation.
Many traditional absorbent dressings include a soft polymer core with or without an absorbent pad (National Institute for Health and Care Excellence (NICE), 2014) and these are generally best suited for use with lightly to moderately exuding wounds. Dressings that include SAPs as part of their design are commonly referred to as ‘superabsorbers’. These dressings – for example, DryMax Super, previously known as DryMax Extra/DryMax Soft, in the UK (CD Medical) – expand on absorption of fluid. However, it has been pointed out that ‘superabsorbent’ is a comparative, not an absolute term (Journal of Wound Care, 2023). As with all wound management products, health professionals should read the manufacturer's instructions prior to using a product.
Notwithstanding the above, the author would agree with Hindhede and Meuleneire (2012) that a dressing's efficiency in managing wound exudate should not be considered solely in terms of the volume of fluid absorbed, but should also take into account the product's ability to retain the exudate within the dressing when external pressure is applied, such as under compression therapy systems. Wound dressings that only absorb low volumes, and have little or no capacity to retain wound exudate, are more likely to result in periwound skin changes (maceration and/or excoriation) (Bishop et al, 2003). Consequently, dressings that absorb relatively large quantities of exudate, but lack the capacity to sequester the exudate and remain wet on the surface, may be less efficient in the management of exuding wounds than those that absorb less but retain the exudate within the dressing (Cutting et al, 2002; Bishop et al, 2003).
Therefore, it is important that all health professionals – those who prescribe and those who use absorbent wound dressing products – fully understand the properties of the chosen product, information that should be evidenced by the product's manufacturer. Health professionals should also be aware that the use of creams or ointments, for example zinc oxide-based preparations such as Sudocrem on the skin surrounding the injured area, may interfere with the absorbency and sequestering function of the product (Ljungh et al, 2006).
The DryMax dressing
DryMax Super/DryMax Soft and Absorbest Super (both names are used for the product internationally) is a conformable, sterile superabsorbent dressing for exuding wounds. It is regarded as a protease modulating dressing, absorbing exudate vertically and retaining it in its core to form a gel (Figure 1). As a result, the dressing core retains exudate-containing bacteria and other detrimental substances (Mihutescu et al, 2022; Journal of Wound Care, 2023). It should be noted that dressings that bind proteases are not suitable for dry wounds or wounds that have a leathery eschar (Hindhede and Meuleneire, 2012).
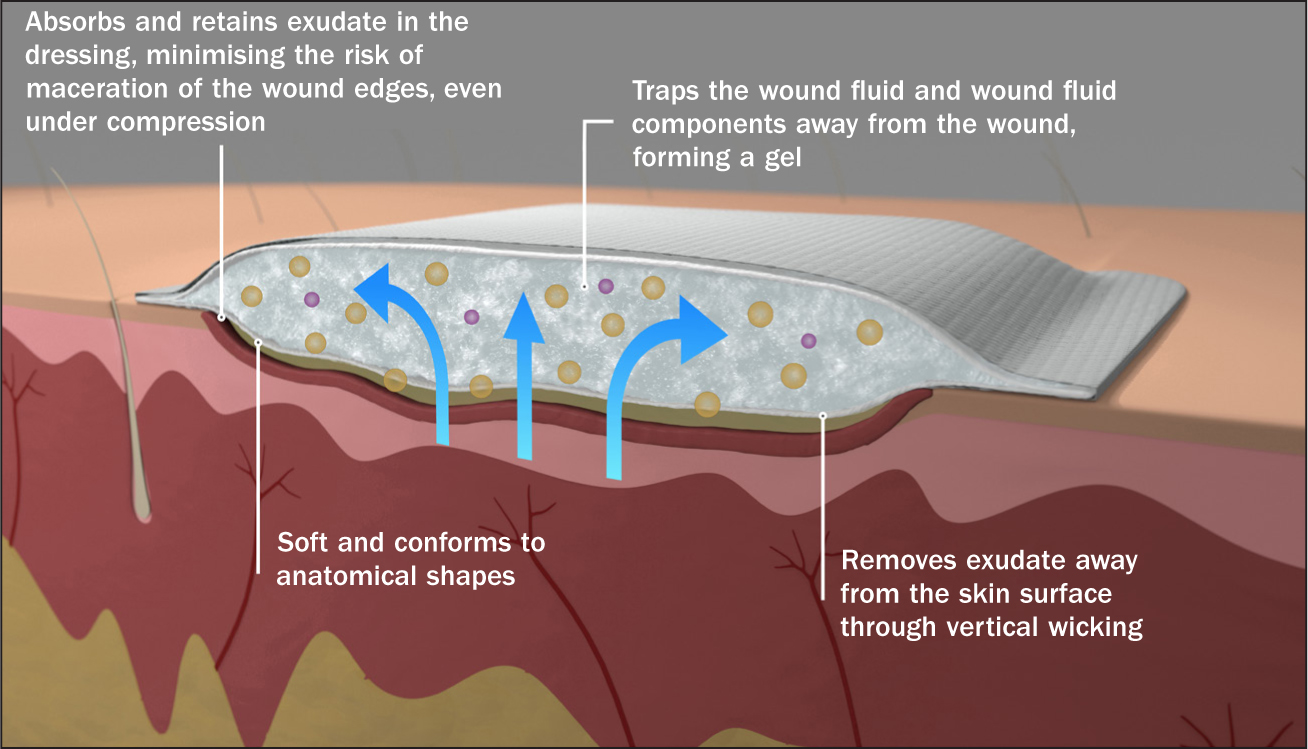
Furthermore, as the fluid component of any wound exudate is bound within the gel, this helps prevent periwound maceration and retain a humid (warm and moist) wound surface environment, which can enhance a patient's wound healing potential (Absorbest AB, 2020). Heavily exuding wounds have been reported to prolong the inflammatory phase, impede growth factor availability, and prevent or delay cell proliferation (Tickle, 2013). The DryMax Super/DryMax Soft and Absorbest Super dressing has been evaluated in a number of observational studies and is arguably an appropriate product for managing heavily exuding wounds. Studies by Stephen-Haynes (2011), Allymamod (2011), Hindhede and Meuleneire (2012) and Stephen-Haynes and Stephens (2012) demonstrated its clinical efficacy in managing chronic hard-to-heal wounds. All the cases documented involved exuding wounds, and DryMax Super dressings were reported to have managed and controlled the exudate, improving patients' wound healing potential.
DryMax Super can be used as both a primary and secondary dressing. It is clinically indicated for exuding wounds, such as leg ulcers, pressure ulcers, diabetic foot ulcers, burns and in the management of lymphoedema. In vitro studies have shown the product to effectively sequester and retain simulated exudate-containing bacteria and other detrimental substances within the dressing core (Figure 1), holding them away from the wound bed (Mihutescu et al, 2022). The product also has excellent properties for the absorption and retention of exudate (Absorbest AB, 2020; Surgical Materials Testing Laboratory, 2020).
Other wound dressing products in the DryMax range that are available in the UK include DryMax Blue and DryMax Border, both of which are classified as superabsorbers (Journal of Wound Care, 2023). Absorbest also manufactures Absorbest Super; Absorbest Super Foam; Absorbest Relevo; DryMax Easy and Gentle from its European base.
The study
This article describes a case series observational study involving a range of patients (n=47; 33 male/14 female) aged between 33 and 91 years (mean 67.4 years), with a variety of acute (n=11) and chronic exuding wounds (n=44). In total, 55 wounds of various aetiologies were managed with DryMax Super, in order to evaluate the previously highlighted properties of the product clinically.
On recruitment to the study, all patients were asked to sign an informed consent form and a photography consent and release form, following explanation by a health professional of the study protocol and reassurance that they could withdraw at any time, without prejudice. The consent allowed the initiating company – CD Medical (UK based) – to use the collected data and photographic materials for educational purposes and in future medical publications.
At all study locations – local Trusts/hospitals/clinical settings – appropriate patient protocols were followed, including the use of local patient consent forms, in addition to those highlighted above.
Evaluation method
The evaluation involved seven sites located across the UK. These were: Accelerate CIC; HCRG Care Group West Lancashire; Southport and Ormskirk Hospital; Beechwood Community Health Centre; Bridgewater; Durnford Treatment Room + Middleton Integrated Nursing Team; and Penrhos Stanley Hospital + Primary Care Treatment Room YPS.
The progress of each patient's wound was evaluated and documented in an evaluation booklet provided by CD Medical, to ensure consistency of data collection, which was carried out over a 4-week period or shorter, if the health professional assessed the wound as no longer requiring or likely to benefit from the use of the study dressing.
Within the evaluation booklet, additional helpful information (Table 2 and Box 2) was provided for the health professional with the aim of enhancing the quality of the data to be analysed/reported on conclusion of the evaluation process.
Table 2. Types of wound exudate
| Type | Colour/opacity | Consistency | Comments |
|---|---|---|---|
| Serous | Clear, amber or straw coloured | Thin, watery | Often a normal part of healing, but an increase or excessive amounts may indicate an underlying issue requiring reassessment |
| Fibrinous | Cloudy | Thin, watery | Containing fibrin strands, may indicate inflammation (with or without infection) |
| Serosanguineous | Clear, pink to light red | Thin, slightly thicker than water | Presence of red blood cells indicates capillary damage, may occur postoperatively or be due to traumatic dressing removal |
| Sanguineous | Red | Thin, watery | Low protein content or presence of red blood cells indicating capillary damage; may be associated with hypergranulation |
| Seropurulent | Cloudy, creamy, yellow or tan | Thin | Serous exudate containing pus, may indicate impending infection |
| Purulent | Opaque, milky, yellow, tan or brown, sometimes green | Often thick | Often thick/sticky – indicates infection, may be associated with malodour |
| Haemopurulent | Reddish, milky, opaque | Thick | Mixture of blood and pus, often due to established infection |
| Haemorrhagic | Red, opaque | Thick | May indicate trauma to the wound or bacterial infection |
Reproduced for evaluation by healthcare practitioners from Exudate Explained
(Wounds UK, 2021)Box 2.Wound odour rating descriptors
| Very strong | Odour is evident upon entering the room (6–10 feet from the patient), with the dressing intact |
| Strong | Odour is evident upon entering the room (6–10 feet from the patient), with the dressing removed |
| Moderate | Odour is evident in close proximity to the patient when the dressing is intact |
| Slight | Odour is evident in close proximity to the patient when the dressing is removed |
| No odour | No odour is evident at close proximity to the patient when the dressing is removed |
The first patient was enrolled in the study on January 18 2023 and the last on 16 May 2023. The study took place over a 4-month evaluation period.
Evaluation results
Throughout the study period, a total of 55 wound types were identified, as per evaluation protocol, and managed with the DryMax Super dressing. The majority of patients had venous leg ulcers (n=21), mixed aetiology leg ulcers (n=10) and surgical wounds (n=7); the incidence of other types of wound was between 1 and 3. Box 3 provides a full breakdown of the wound types encountered. The mean wound duration at first patient assessment was 11 months (range between <1 month and <12 months) (Table 3).
Box 3.Patient wound types (n=55)
| Tyoe | Number |
|---|---|
| Bullous pemphigoid | 1 |
| Diabetic foot ulcer | 2 |
| Haematoma | 1 |
| Lymphatic leaking areas | 3 |
| Lymphorrhoea (bilateral leg) | 1 |
| Mixed aetiology leg ulcer | 10 |
| Pressure ulcer | 6 |
| Surgical wound | 7 |
| Traumatic wound | 3 |
| Venous leg ulcer | 21 |
Table 3. Wound duration on presentation (n=55)
| Duration | Number |
|---|---|
| 1 month or less | 12 |
| 1–6 months | 18 |
| 6–12 months | 5 |
| More than 12 months | 16 |
| Not answered | 4 |
In roughly half the patients the DryMax Super dressing was used in conjunction with compression: 28 patients had compression versus 27 who did not. A range of compression systems were used: Coban 2 and lite (3M), Actico (L&R), Actilymph (L&R), K-two (Urgo) and K-plus (Urgo).
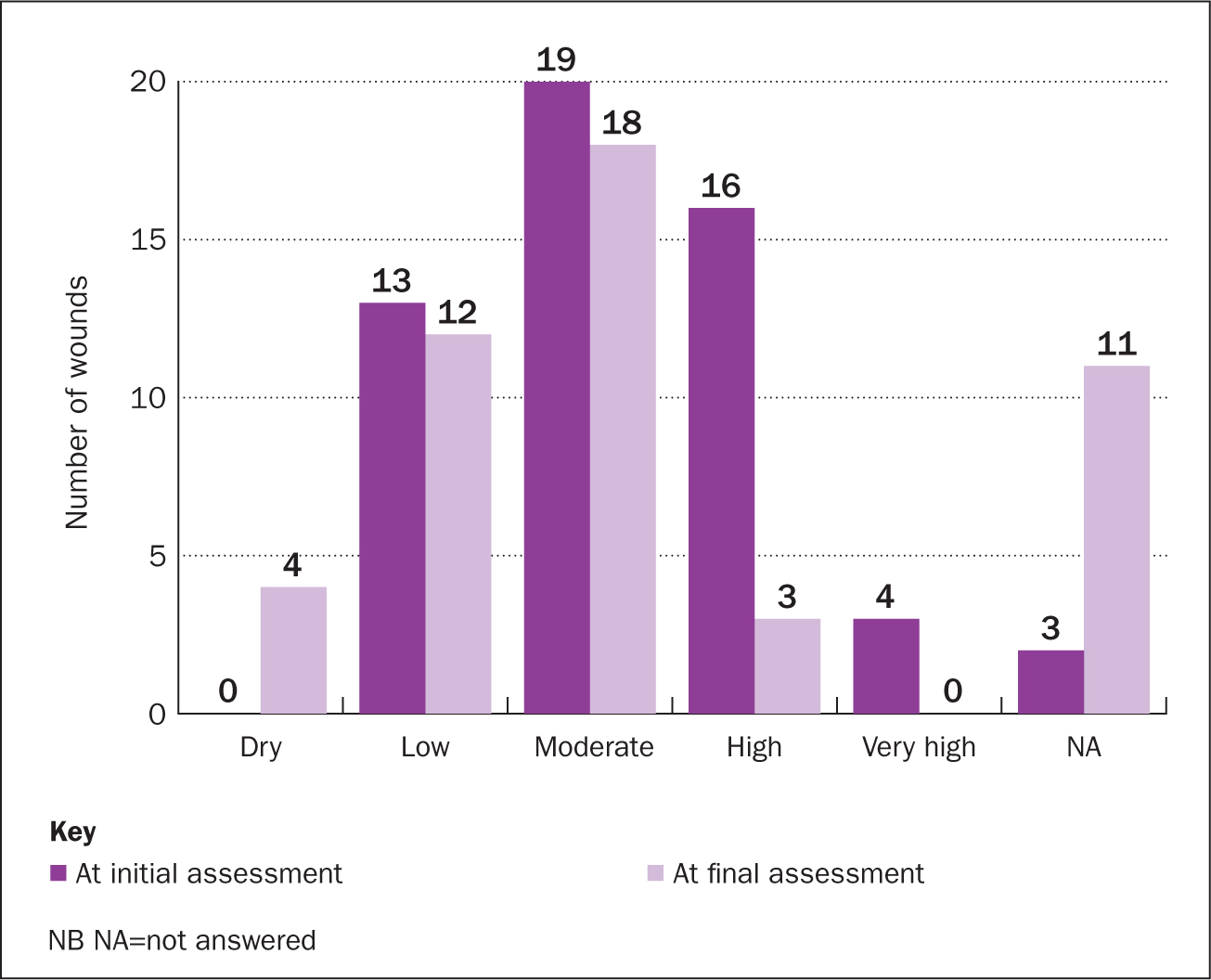
Exudate at start and end of study period
Through the evaluation period, the study dressing was assessed to have had excellent fluid handling properties, as the amount of wound exudate assessed during the initial and final assessments within the wound margins was reported to have reduced. Furthermore, the number of wounds assessed as having no excess wound exudate at initial and final assessment increased by 4 (Figure 2).
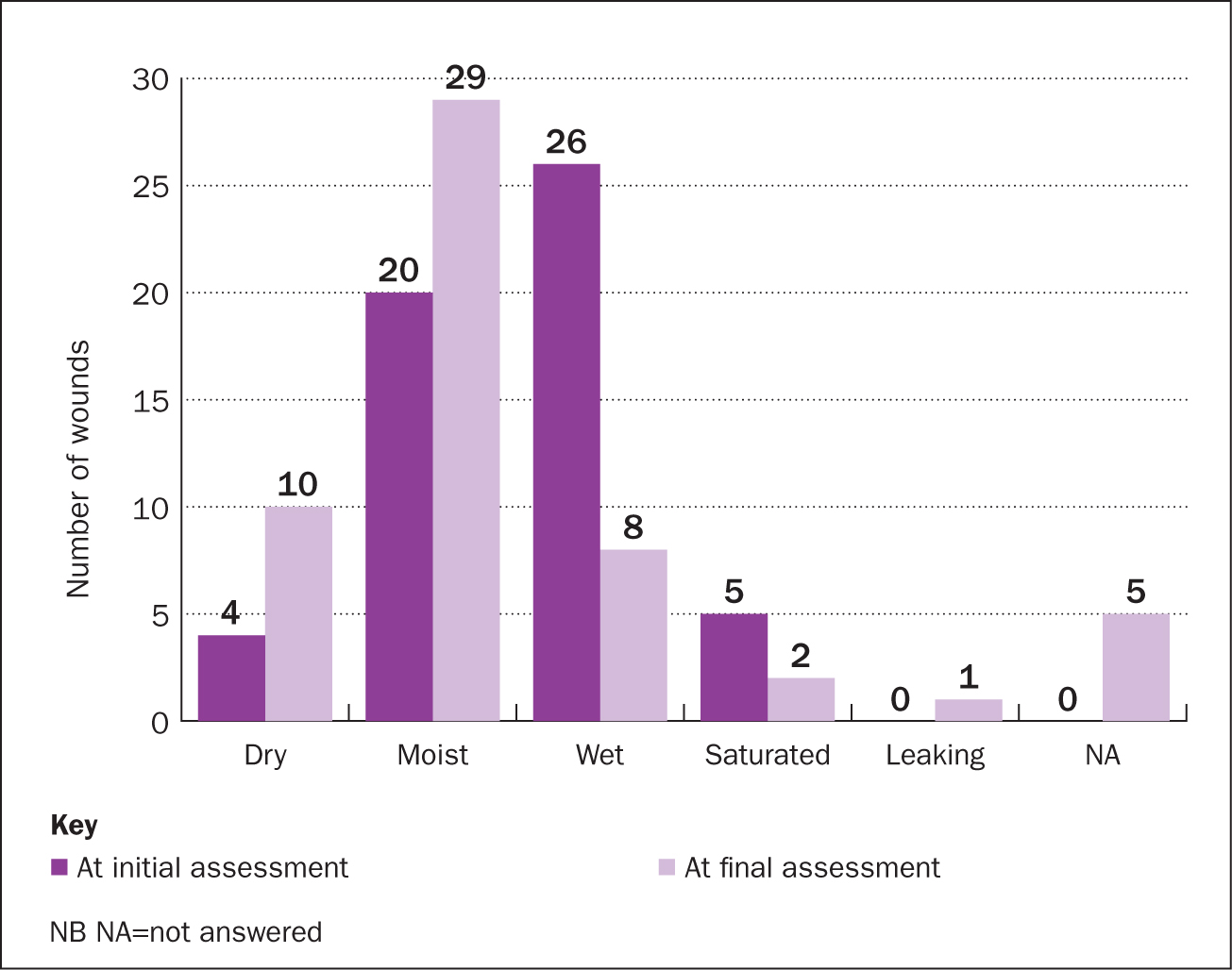
It was also reported that, at the time of dressing change the wound dressing had absorbed more wound exudate, at the end of the study period, compared with assessments undertaken at the start of the evaluation. The number of wounds that were assessed as not producing any excess exudate over the study period was also reported to have increased (Figure 3).
Wound condition
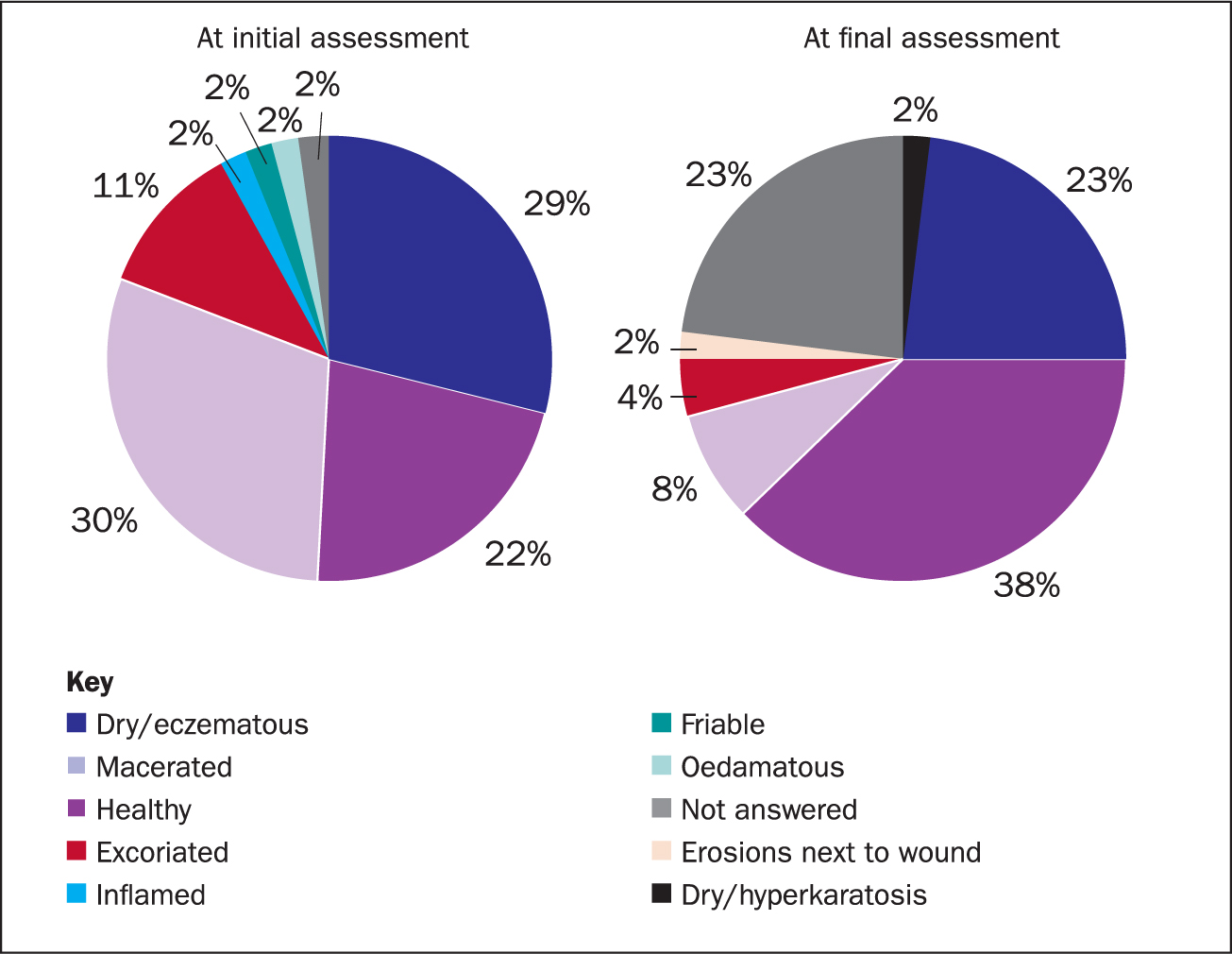
Over the 4-week evaluation period, the health professionals observed a reduction in macerated and excoriated periwound was observed (Figure 4). Average periwound condition reduced from 30% macerated at initial assessment to 8% at final assessment, and from 11% excoriated at initial assessment, to 4% at final assessment - assessed visually by the assessor. Healthy periwound skin assessments increased from 22% at initial assessment to 38% at final assessment.
Patient comfort
The majority of patients (85%) reported that they found the DryMax Super to be ‘much better’ or ‘better’ than the previous dressing used in terms of reported comfort (Figure 5). In addition, 90% said it was ‘much better’ or ‘better than the previous dressing used in terms of conformability.
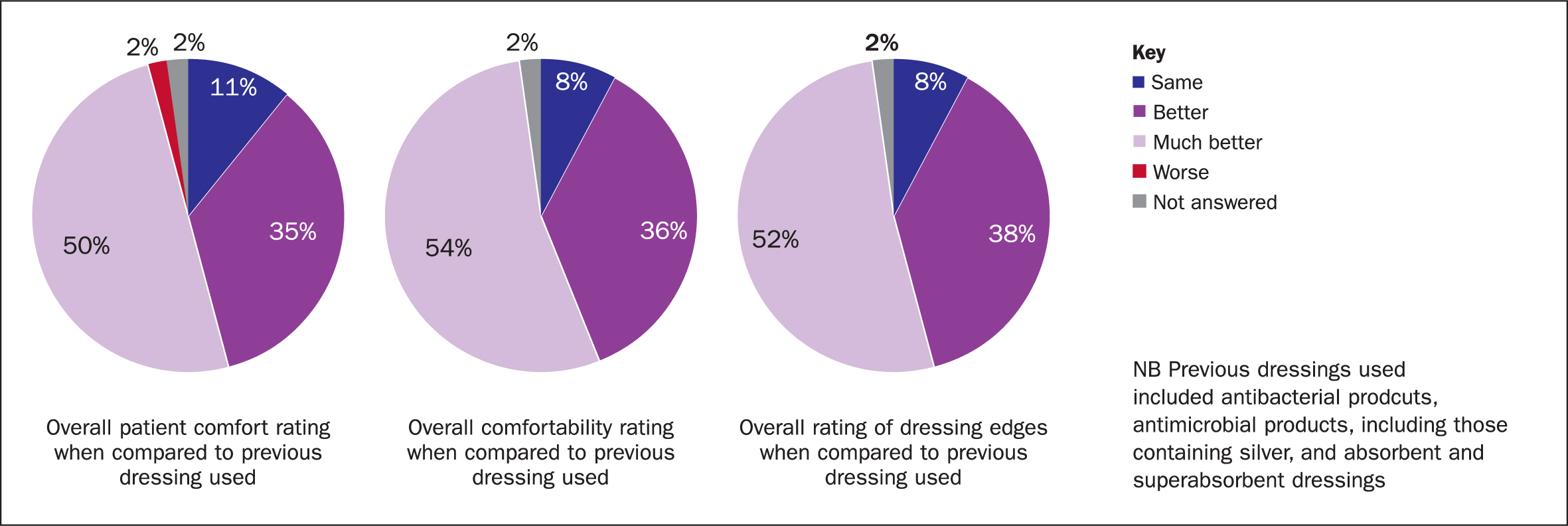
In terms of maintaining integrity (dressing edges), which was assessed visually by the assessor, in 90% of the cases DryMax Super was reported to be ‘much better’ or ‘better’.
Performance ratings of DryMax Super dressings
Summaries of the overall study findings are presented in Table 4 and Table 5. All study parameters are included: they highlight that the majority of patients and clinicians were satisfied with the performance of the dressing. They found it easy to apply and remove and, when in use, it was reported to conform to all of the patients' limbs. The dressing was also reported to have very good absorption and odour control (when applicable) properties.
Table 4. Reported and assessed overall performance characteristics on completion of the evaluation (n=55 wounds)
| 21.1 Ease of application of DryMax? | 21.2 Ease of DryMax removal? | 21.3 Overall conformability of DryMax? | 21.4 Exudate absorption capabilities of DryMax? | 21.5 Odour management capabilities of DryMax? (If applicable) | 21.6 Overall clinical assessment and satisfaction with DryMax? | 21.7 Overall patient satisfaction of DryMax? | |
|---|---|---|---|---|---|---|---|
| Very Good | 38 | 37 | 36 | 31 | 24 | 31 | 30 |
| Good | 17 | 17 | 19 | 20 | 14 | 21 | 21 |
| Fair | 0 | 1 | 0 | 3 | 6 | 3 | 2 |
| Poor | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| Very poor | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| n/a | 0 | 0 | 0 | 0 | 9 | 0 | 0 |
| Not answered | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
Table 5. Performance of DryMax Super at end of evaluation in comparison to previously used dressings (n=55 wounds)
| 23.1 Overall performance of DryMax | 23.2 Exudate management of DryMax | 23.3 Dressing edges of DryMax | 23.4 Non stick to wound bed of DryMax | 23.5 Comformability of DryMax | 23.6 Prevention of maceration of DryMax | 23.7 Odour control of DryMax | 23.8 Patient comfort of DryMax | 23.9 Ease of application of DryMax | 23.10 Ease of removal of DryMax | |
|---|---|---|---|---|---|---|---|---|---|---|
| Much better | 23 | 23 | 30 | 26 | 31 | 25 | 14 | 28 | 26 | 26 |
| Better | 10 | 9 | 21 | 10 | 20 | 7 | 4 | 20 | 8 | 8 |
| Same | 18 | 19 | 4 | 17 | 4 | 20 | 24 | 5 | 21 | 20 |
| Worse | 4 | 4 | 0 | 1 | 0 | 2 | 0 | 1 | 0 | 1 |
| Much worse | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| n/a | 0 | 0 | 0 | 0 | 0 | 1 | 12 | 0 | 0 | 0 |
| Not answered | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
Case studies
The case studies presented in Figure 6 and Table 6 are illustrative of the range and nature of the wounds that were included in this study.
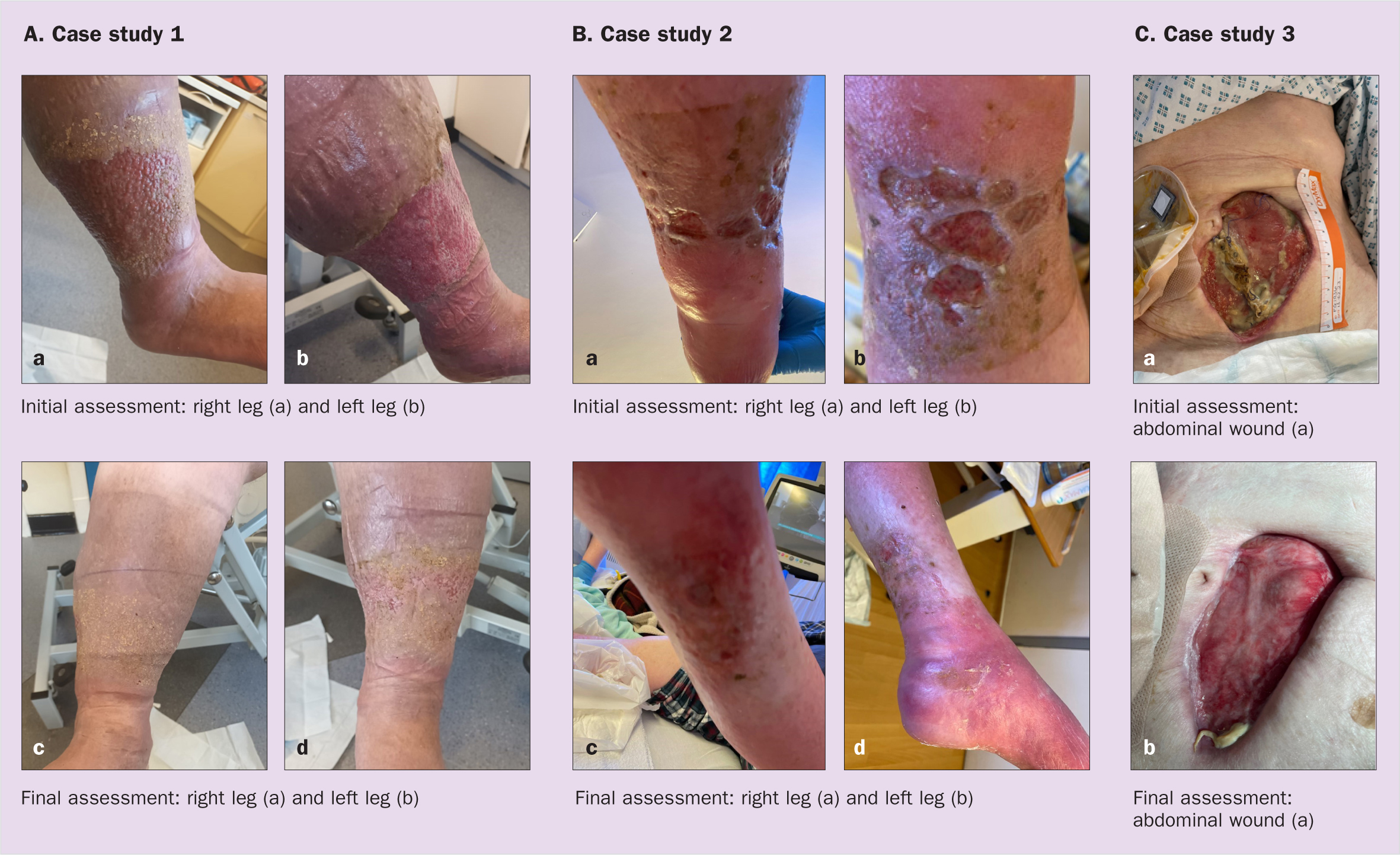
Table 6. Overview of presented case studies
| Case study 1 – see Figure 5(a) | Case study 2 – see Figure 5(a) | Case study 2 – see Figure 5(c) | |
|---|---|---|---|
| Initial assessment |
|
|
|
| Aim |
|
|
|
| Final assessment |
|
|
|
| Clinician comments |
|
|
|
Examples of case study reports included in the evaluation process (2023), courtesy of evaluation site data collectors
Discussion
The current study's results indicate that the evaluated product is suitable for the management of a variety of exuding wound types (low to very high), when used either as a primary or secondary dressing. It also performed well under a range of commercially available compression therapy products. The dressing was reported as being well tolerated by the patient and, according to the health professionals involved in the evaluation, it was easy to apply and remove. Their observations also suggested that the superabsorbent being evaluated promoted wound healing and was effective in protecting the periwound skin from maceration and erythema, for example. It could therefore be argued that the clinical efficacy of the superabsorber related to both exudate absorption and retention was supported by the results of this study.
It is worth noting that the results of this case study series support and build on previously published results from another significant observational study by Hindhede and Meuleneire (2012).
The previously published case series involved 30 patients - aged between 23 and 94 years, with acute and chronic wounds of various aetiologies to evaluate the capacity of DryMax Extra in managing excessive exudate. All patients recruited to the study were assessed at the same clinical centre and all patients were treated by the same practitioner. The study was undertaken over a 9-month period, between December 2008 and September 2009.
Limitations
As a case study series, no specific inclusion and exclusion criteria were indicated for the data collectors to follow, or the health professionals involved in the evaluations to consider when recruiting patients to the study. The lack of such criteria can result in the study population not being recruited in a consistent, reliable and objective manner.
The starting point for the study was dictated by the clinical needs of individual patients. As a result, it included a variety of patients with exuding wounds who appeared not to be responding to the previously chosen dressing regimen at the time of inclusion.
Conclusion
The clinical use of superabsorbent dressing materials has increased significantly over the past decade and, although it can always be argued that more evidence is required to support this group as well as all wound management products, this and other studies have indicated that DryMax Super dressings do manage and retain exudate well. The dressing helps to:
- Protect the patients' periwound skin
- It is comfortable and well tolerated by patients
- Clinicians report that it is easy to use.
As highlighted previously, poorly managed exudate can have a significant negative effect on a patients HRQoL and, therefore, it is important that, when assessing a wound, all health professionals choose the most appropriate dressing for a specific wound at the right time (stage of wound healing) in order to assist with achieving any identified management aims/objectives. The author hopes that the information within this article will help to clarify/enhance the evidence base colleagues use to support their and their clinical colleagues' future wound management choices.
KEY POINTS
- Excess and uncontrolled wound exudate can inhibit the wound healing process, with significant consequences for the patient. It has negative effects on patients' health-related quality of life, and also has avoidable cost implications for the healthcare system
- An observational case series designed to evaluate the absorbency and fluid handling properties of the study dressing (DryMax Super), and its use under compression, highlighted favourable results for the majority of patients included in the study
- The results of this case study series support and build on previously published results from another significant observational study by Hindhede and Meuleneire (2012)
CPD reflective questions
- What are the consequences of too much or too little wound exudate and the effects of both on the ‘normal’ wound healing process?
- How do you measure and document exudate associated with wounds in your own clinical setting?
- What are the main clinical properties of the study dressing (DryMax Super) referred to and as supported by the data reported within this article?


