Patient safety should be at the heart of all healthcare, including protecting patients from catheter-associated urinary tract infections (CAUTIs). Over the past decade, the NHS has been working to reduce CAUTIs. The main thrust of this has been the ‘no catheter equals no CAUTI’ approach (NHS England and NHS Improvement, 2018; Trueland, 2019). But there will always be patients who require a urinary catheter (Royal College of Nursing (RCN), 2019). How are they to be kept safe from CAUTIs?
Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH) took a different approach. The Trust took the decision to ensure that the catheter gel used by staff when catheterising patients provided as much protection as possible against CAUTIs.
This article outlines the policies relating to catheterisation that have been published over the past 15 years or so, and the emphasis on reducing CAUTIs. It also discusses why the right catheter gel is so important in urethral catheterisation, and why the NNUH chose one particular gel.
Trust background
NNUH is situated in the Norfolk town of Norwich. The Trust comprises the Norfolk and Norwich University Hospital, the Cromer Hospital and the Jenny Lind Children's Hospital. The Norfolk and Norwich University Hospital has more than 1200 beds and serves the population of Norfolk. It provides a full range of acute services. Specialist services include oncology and radiotherapy, neonatology, trauma and orthopaedics, plastic surgery, vascular surgery, bone marrow transplants, interventional radiology, brachytherapy, specialist cardiology, paediatric medicine and surgery. It has the fifth busiest NHS cancer service in England (NNUH, 2020).
Catheterisation
RCN guidance stated that catheters can provide an effective way of draining the bladder, for both short and long-term purposes (RCN, 2019). Being continent is a very important factor in maintaining a patient's dignity. Although incontinence should be thoroughly investigated and catheterisation should not be the first line of treatment, catheters can be an effective tool in managing a patient's incontinence. It is usually used in patients who are having problems emptying their bladder, for a variety of reasons (Hill and Michelle, 2020).
Catheterisation is an invasive clinical procedure, which involves inserting a flexible tube, a catheter, into a patient's bladder, either via their urethra or a suprapubic stoma, to empty their bladder (Hill and Michelle, 2018). It involves serious risks to a patient's health, such as an increased risk of urinary infection and possible damage to the urethra (Kyle, 2011). Therefore a risk assessment must be undertaken before performing catheterisation (RCN, 2019). (See Box 1 for examples of when catheterisation is appropriate). Catheterisation should be undertaken only by health professionals who are suitably trained and competent in the type of catheterisation required, whether female urethral, male urethral or suprapubic (National Institute for Health and Care Excellence (NICE), 2017).
The entrance to the urethra, the urinary meatus, needs to be cleaned before catheterisation begins (Loveday et al, 2014). This can be achieved with the use of sterile normal saline and a gauze pad (Loveday et al, 2014). This is not to clean microorganisms from the urinary meatus, but to remove any detritus and contaminates, such as stale urine and even faecal matter, reducing the risk of introducing them into the bladder when the patient is catheterised.
Owing to the risk of causing a urinary tract infection during catheterisation, catheter insertion should always be carried out as an aseptic technique (Wilson, 2011). Catheters are supplied as a sterile item, placed in a plastic bag within the outer packaging. This enables the health professional to insert the new catheter without having to handle it. As an aseptic procedure, any gloves need to be removed, hands decontaminated and sterile gloves applied before catheterising the patient (Loveday et al, 2014). Some patients will require re-catheterisation. In such cases, removing the previous catheter, and cleaning the urinary meatus, should be done as a clean procedure, after washing the hands and wearing clean examination gloves.
Catheter insertion gels are an important part of the catheterisation kit and need to be used at all catheterisations, for both men and women (Wilson, 2013). Simple lubricants, such as KY Jelly, are not a suitable substitute (Kyle, 2011). Designated catheter insertion gels have been purposefully designed for lubrication during catheterisation. Catheter insertion gels often contain a local anaesthetic and an antiseptic; Instillagel® Anaesthetic Antiseptic Lubricant (UK Distributor: CliniMed Ltd, 2020), for example, contains lidocaine hydrochloride and chlorhexidine, respectively.
The biggest health risk from catheterisation is a CAUTI. Approximately one in five NHS hospital inpatients has a urinary catheter (Smith et al, 2019). Of these patients, 7.3% will develop a CAUTI (Smith et al, 2019). This may not sound like a large percentage, but in reality this is 52 085 individual patients a year (Smith et al, 2019). Of these patients, 4.8% will develop a catheter-associated bloodstream infection (CABSI), which has a mortality rate of 19.5% (Smith et al, 2019). CABSIs cost the NHS £99 million annually (Fisher et al, 2017). CAUTIs are serious infections with serious patient outcomes associated with them, resulting in an economic burden for the NHS. They are not ‘just another urinary tract infection’ (UTI).
Catheterisation policy
Numerous policies and guidance have been introduced over the past 20 years or so, with the aim of reducing the number of healthcare-associated infections (HAIs), and preventing UTIs has been a large part of this.
In 2003, the Department of Health (DH) published Winning Ways (DH, 2003). This emphasised the problem of infections in healthcare. It stated that a urinary catheter should only be used when there is no alternative and removed as soon as possible because of the risk of CAUTIs.
In 2005, the DH published Saving Lives (DH, 2005). This was a programme to reduce HAIs, focusing on meticillin-resistant Staphylococcus aureus and Clostridium difficile. It listed five high-impact intervention care bundles, including one on urinary catheter care.
In 2009, the National Audit Office (NAO) published Reducing Healthcare Associated Infections in Hospitals in England (NAO, 2009). This report was based on an audit carried out in English hospitals in 2006, which found that 20% of recorded hospital infections were UTIs, and 80% of these infections were related to catheters.
In 2013, the DH published The UK 5 year Antimicrobial Resistance Strategy 2013-2018 (DH, 2013). This set goals and guidelines for reducing HAIs, and specified percentage reductions, divided into programmes. In programme 1, it required a 50% reduction in healthcare-associated Gram-negative bloodstream infections in England by 2020/2021. A large cause of these bloodstream infections are urinary tract infections, and as the NAO report revealed (2009), a large number of urinary tract HAIs are from catheters. Programme 2 required, in the same time frame, a 50% reduction in inappropriate antibiotic prescribing. Because CAUTIs make up one of the largest groups of HAIs (Smith et al, 2019), a dramatic reduction in these would also see a large reduction in antibiotic prescribing. This policy of reducing infection rates and antibiotic usage, directly set targets for NHS trusts to reduce CAUTIs. They could not meet these targets without doing so.
In 2014, NICE published infection prevention and control guidelines. NICE required that catheterised patients are not just assessed before catheterisation but they are regularly reviewed to determine if the catheter is still needed, and if it is not, it should be removed as soon as possible (NICE, 2014).
In 2017, NHS Improvement and Public Health England (PHE) published Preventing Healthcare Associated Gram-Negative Bloodstream Infections (NHS Improvement and PHE, 2017). This required that the infection rate for Gram-negative bloodstream infections be reduced by 50% by 2021. As Gram-negative bloodstream infections are often secondary to urinary tract infections, reducing CAUTIs would have a direct effect on the rate of bloodstream infections.
In 2017, the Health Innovation Network (HIN) published a report into their campaign ‘No catheter, no CAUTI’ (HIN, 2017). This was the final report on their campaign to reduce catheter usage, and where catheters are necessary, to de-catheterise patients as soon as possible. RCN guidelines also recommend avoiding catheterisation if possible, emphasising the need for assessment before each catheterisation and ongoing assessment to determine if a catheter is still needed (RCN, 2019).
The aim of current policy and guidance is now to not catheterise patients unless absolutely necessary, to reduce the risk and the rates of CAUTIs. But what about the patients who need catheterisation—patients who have functional issues that stop them from being continent or cause urinary retention. How are CAUTIs to be prevented in such patients?
NNUH policy
NNUH added an extra element that has helped reduce CAUTIs in its patients, by requiring a specific catheter gel be used during all catheterisation and re-catheterisation procedures.
In 2007, in response to the Saving Lives catheter care bundle (DH, 2005), NNUH began to look at which catheter gel should be used in the Trust. This was a long discussion, involving clinicians, infection control staff, the procurements department and pharmacy.
In 2011, NNUH carried out a point prevalence survey and found that 16.5% of the Trust's patients were catheterised and that 11% of its HAIs were caused by UTIs (NNUH internal unpublished report, 2018) (Figure 1). This led to the Trust taking measures to reduce the incidence of CAUTIs. It first adopted the epic 3 National Evidence-Based Guidelines for Preventing Healthcare-Associated Infections in NHS Hospitals in England (Loveday et al, 2014) as Trust policy. This stated:

Next came the choice of catheter gel. The epic 3 guidance required that the catheter gel is sterile, single-use and contained an anaesthetic ingredient (Loveday et al, 2014). The Trust had already been using Instillagel for catheterisation, but it also looked at different products during this process. The Trust's chief pharmacist argued that the choice of catheter gel should come under the pharmacy department's remit rather than that of procurement. The pharmacy department wanted a product that contained chlorhexidine in a stable formulation, which would not degrade over time, and a similar lidocaine dose. The infection control staff were also keen that the product used was proven to contain the correct dose of chlorhexidine, for its antibacterial properties. Instillagel, as a licensed medicine, fulfilled this requirement, whereas other gels did not, in the Trust staff 's experience. When seeking approval for a catheter lubricating gel to be used Trust-wide, the chief pharmacist chose to present Instillagel to the Trust's medicine management board and the procurement department presented an alternative product. The medicine management board approved Instillagel for Trust-wide use.
All catheters and related products are dispensed by the pharmacy department, which is able to record all batch numbers and to which department they are distributed. Pharmacy was thus able to control the supply of catheter gels and ensure that only Instillagel was supplied for catheterisation. Instillagel is covered by a drug protocol as part of the urinary catheter policy, to be used by any suitably trained staff. Because it is supplied by the pharmacy department, there is no need for it to be prescribed or for there to be a patient group directive (PGD) written to cover it. This may not be possible for all trusts, especially those that cover community services, outside the reach of a central pharmacy department. In that case a PGD should be considered. This would allow non-prescribing practitioners to access a product such as Instillagel, ensuring it is used with all catheter patients.
When Instillagel was first introduced, prior to it being adopted Trust-wide, the Trust invited staff from CliniMed, to do ‘walking the wards’ training, in different clinical areas. When Instillagel was adopted Trust-wide it was included in all catheter training courses. Periodically, there have been infection prevention and control awareness weeks and catheter awareness days, where CliniMed staff were also invited to promote Instillagel usage, involving ward-based training and displays in the canteen.
In 2016, another point prevalence survey was carried out in the Trust, following the adoption of the epic 3 recommendations and the trust-wide introduction of Instillagel. The results of this revealed that 20.2% of the Trust's patients had a urinary catheter, which was nearly 4% more than in 2011, yet HAI UTIs had reduced to 4% of all HAIs (NNUH internal unpublished report, 2018) (Figure 2).
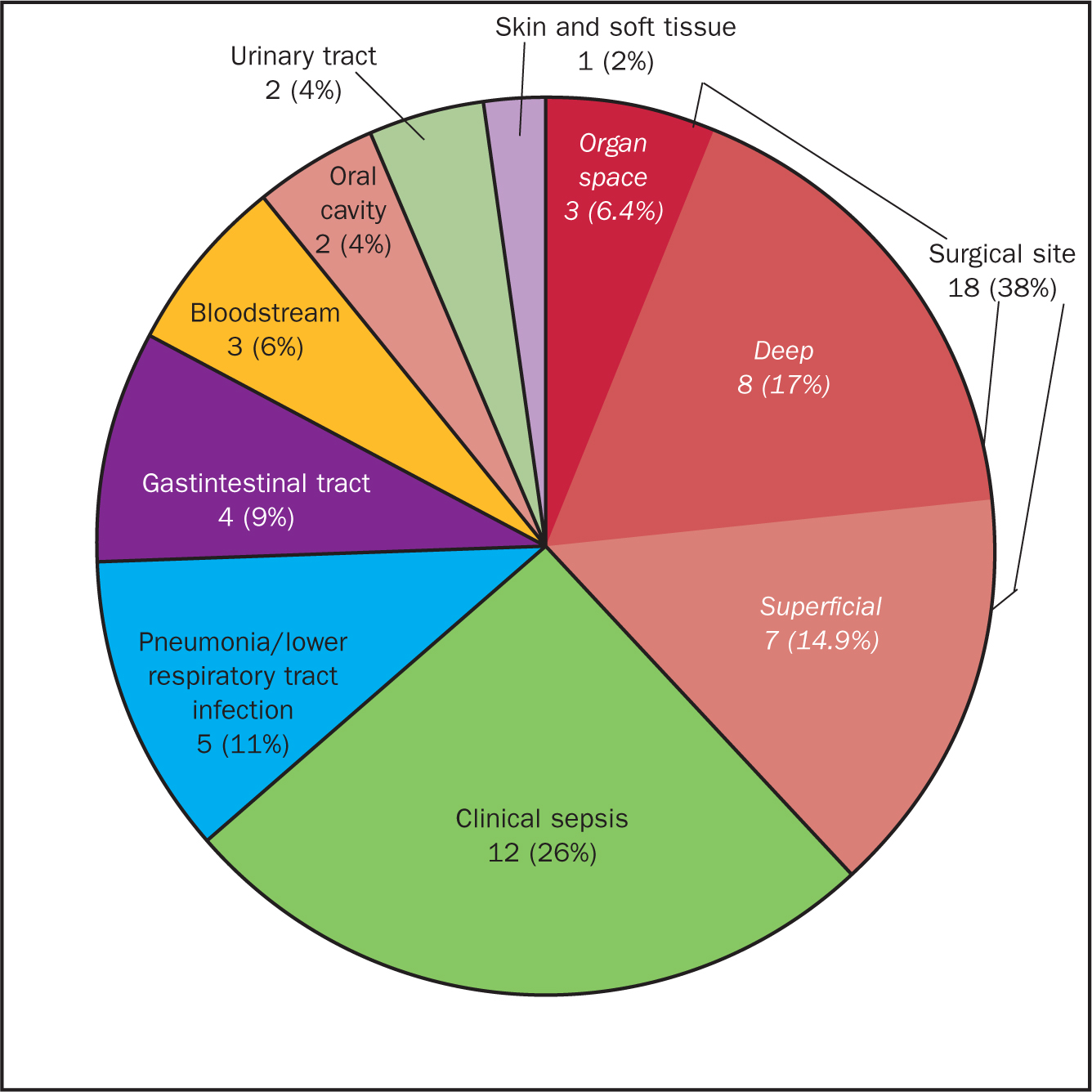
That point prevalence survey was repeated in June 2018. This found that 19.9% of Trust patients had a urinary catheter but only 1% of the Trust's HAIs were UTIs (NNUH internal unpublished report, 2018).
NNUH has seen an increase in patients with urinary catheters between 2011 and 2018 and yet they have also seen a dramatic decrease in HAI UTIs. The only change in care has been the introduction of Instillagel for all catheterisations. These results show the effectiveness of Instillagel in helping to prevent CAUTIs. NNUH has seen a more than 50% fall in the rates of CAUTIs. NHS Improvement aimed for a 50% reduction in Gram-positive and Gram-negative bloodstream infections by 2021 (DH, 2013; NHS Improvement, 2017), and CAUTIs are a large cause of bacterial bloodstream infections.
Using Instillagel
The epic 3 guidelines (Loveday et al, 2014) recommends using a sterile, single use, anaesthetic gel when catheterising. The RCN guidelines state that a sterile anaesthetic gel should be used (RCN, 2019). NICE guidelines state that ‘an appropriate lubricant from a single-use container’ should be used (NICE, 2017). Instillagel contains lidocaine hydrochloride (a local anaesthetic) 2% and chlorhexidine gluconate solution (an antiseptic) 0.25% (CliniMed Ltd, 2020). The catheter gel comes in a single-use, designated container designed to aid administration.
Local anaesthetic
The urethra is not a smooth, rigid tube, it is a ‘ribbon-like structure’ that dilates only when urine is passing through it (Kyle, 2011). When the bladder is not emptying, the urethra lies flat, like a deflated fire hose. Passing a catheter through the urethra can damage its lining and can be painful (Kyle, 2011). Using a catheter gel with a local anaesthetic will help dilate the urethra, opening it out, reducing trauma to the urethra, and reducing infection because it helps maintain the protective barrier of the urethra lining (Kyle, 2011). It will also desensitise or numb the urethra, preventing discomfort, thus easing the pain of catheterisation (Kyle, 2011).
The female urethra is about 3-4 cm long while the male urethra measures around 18-22 cm (Kyle, 2011). In the past, health professionals have been taught that, because the female urethra is much shorter than that of the male, women only required a simple lubricant, such as sterile water, to catheterise them (Doherty, 1999). The first author was taught this as a student nurse. But trauma can happen at any stage of catheterisation, and a short urethra does not prevent this (Kyle, 2011). Therefore, anaesthetic gel should be used when catheterising both women and men (Kyle, 2011). It is also not acceptable to deny a person the pain relief of an anaesthetic at catheterisation just because of their sex. This is why a local anaesthetic is so important in a catheter gel, and one of the reasons Instillagel was chosen for the Trust.
Lidocaine can cause a passing stinging sensation as it anaesthetises the urethra, and patients need to be warned about this (Kyle, 2011).
Antiseptic
Chlorhexidine is widely used as a topical antiseptic in healthcare. It acts on both Gram-positive and Gram-negative bacteria, the main causes of CAUTIs (Kyle, 2011).
There have been questions raised about the safety of chlorhexidine in some articles in nursing journals, claiming that hypersensitivity to it is rising (Williams, 2017). On closer inspection this is based on questionable evidence. Williams (2017) does not provide any evidence or figures to support this claim. The main thrust of the argument seems to be based on sources such as Stewart and Lenaghan (2015) and Gould et al (2009). Stewart and Lenaghan (2015) described a case study of only one patient and yet draw universal recommendations from it. Gould et al (2009) made only a passing reference to chlorhexidine being ineffective. The authors of the present article were not able to find any peer-reviewed articles that provide evidence of an increase in chlorhexidine sensitivity.
The Royal College of Anaesthetists found the incidence of reaction to chlorhexidine to be 0.78 per 100 000 exposures and therefore is such a low risk that is not considered one of the main causes of perioperative anaphylaxis (Garcez, 2018). A urinary catheterisation and a surgical operation are not the same clinically, an operation provides a much higher risk of a substance causing a reaction.
Kyle (2011) quotes an audit by Kambal et al (2004) of patients undergoing gynaecological surgery. A catheter gel using chlorhexidine was used to catheterise, reducing CAUTIs by 50%.
A randomised controlled trial in Australia, involving 21 hospitals and 1642 participants, found a 74% reduction in catheter-associated asymptomatic bacteriuria and a 94% decrease in CAUTIs, with no adverse events reported when products containing chlorhexidine were used at catheterisation (Fasugba et al, 2019). The initial rates of both catheter-associated asymptomatic bacteriuria and CAUTIs were both low before the study began, but this degree of reduction is still impressive.
Packaging
Suitable packaging can make a product practical, easy to use and keep it sterile. Instillagel is supplied in a sterile, single-use syringe (CliniMed Ltd, 2020). Single-use syringes keep the gel sterile, free from contaminates, and so reduce the risk of infection from contaminated gel. Multiple-use tubes of lubricant could result in the gel becoming contaminated. The syringe applicator means the nozzle can be gently inserted into the urinary meatus. If catheterising a female patient, who may have a urinary meatus that is difficult to find or distinguish, once it has been found and the gel has been instilled, the nozzle can be left in the urinary meatus to mark the position of the meatus ready for catheterisation (Wilson, 2013).
In a clinical review, Tyler-Murphy and Whitling (2017) found the packaging of Instillagel was superior to other products. Over a period of use they identified the following qualities:
The right packaging can make a product clinically safe and simple to use and also cost-effective because the maximum number of products purchased are used. Products that are packaged well are less likely to have to be discarded because the packaging is damaged, therefore compromising sterility, or the product itself is broken.
Conclusion
Reducing catheterisation has been beneficial in reducing CAUTIs (HIN, 2017) but there are still patients who will need catheterisation and for them the ‘no catheter’ approach is not an option (Box 1).
NNUH has shown that there is a different approach to reducing CAUTIs. From 2011 to 2018 it reduced the HAI UTI rate from 17% of all HAIs down to 1% by changing the catheter gel used to one containing both lidocaine and chlorhexidine (NNUH, 2018 internal unpublished report).
CAUTIs should never be seen as an occupational hazard, they should always be seen as preventable infections. There will always be patients requiring urinary catheters, therefore there should be more than one approach to reducing CAUTIs.

