Since the 1970s, peripherally inserted central catheters (PICCs) have been used to deliver intravenous (IV) therapy, initially in critical care for patients requiring vasoactive medications, multiple infusions and frequent blood sampling and to reduce needlestick injury (Mielke, et al, 2020). As modern healthcare has adapted and responded to major changes in health trends, the benefits of using PICCs in delivering IV therapies have become well evidenced (Ray-Barruel, et al, 2022; Pinelli et al, 2023a).
PICCs are classified as long-term vascular access devices because they can remain in situ for as long as the patient requires IV access (Moss et al, 2021). They are used in hospital inpatients requiring vesicant medical treatments such as chemotherapy, antibiotic therapy and parenteral nutrition; they are also used to support early discharge from secondary care into alternative community care settings or the patient's home for ongoing IV therapy, commonly referred to as outpatient parenteral antibiotic therapy (Govindan et al, 2021; Clarkson and Snape, 2024).
Despite the widespread use of PICCs, complications can arise, such as catheter exit site bleeding, upper limb thrombosis, catheter-related bloodstream infection, exit site infection, mechanical malposition or dislodgment. These can be painful, uncomfortable and distressing for the patient (Wang and Zhao, 2022; Pinelli et al, 2023b). Managing complications associated with PICCs can be complex and costly (Pu et al, 2020).
Ensuring that the PICC has been inserted in the best possible way, using up-to-date, evidence-based practice, is key to reducing the development of complications in the first instance (Thomsen et al, 2024). Standardisation of practice in vascular access and IV therapy has been shown to improve the patient experience and reduce these complications.
PICC insertion standardisation can reduce complications. This can be achieved by having dedicated vascular access teams who use their specialist knowledge and skills to ensure the procedure is successful and, because the same technique is used for every PICC placement, it is safer (Quinn et al, 2024).
From the vascular access specialists’ point of view, bleeding from the exit site of a newly sited PICC is an unwanted side effect of the insertion procedure (Bertoglio, 2022). Often this bleeding results from the dermatotomy made during the insertion procedure to enable the splittable sheath to be inserted over the guidewire so the PICC enters the vessel smoothly (Grewal et al, 2020). Exit site bleeding can also occur after insertion and during general care and maintenance of the device, but this is less common (Scoppettuolo et al, 2013).
Exit site bleeding can be a significant concern as it can predispose patients to infection as well as cause them considerable distress. Common causes of catheter exit site bleeding are: insertion trauma; coagulopathies; anticoagulation therapy; mechanical factors (improper securement or catheter movement secondary to activities of daily living); and infection (Chopra, 2024).
Exit site bleeding can lead to dressing disruption, which in turn can lead to additional complications such as pistoning of the catheter at the insertion site, thrombosis, phlebitis of the vein and catheter migration or dislodgment (Lui et al, 2023). Repeated removal of the adhesive film dressing can cause issues such as folliculitis and other skin injuries related to medical adhesives, which can be a gateway for bacteria to enter the skin around the catheter site.
When a skin injury extends through the epidermis and into the dermis, bleeding occurs and causes an inflammatory response. Although clotting mechanisms are activated in the first instance, it can take serval hours for an eschar to form to restore the integrity of the epidermis (Brown et al, 2018).
Reducing complications
Adopting practices that focus on reducing exit site bleeding of PICCs and other vascular access devices is a strategy to reduce catheter-related complications (Duwadi, 2019).
Several methods can be used to manage exit site bleeding effectively. It is common practice for a gauze pad to be placed over the exit site of newly sited PICCs for the first 24 hours after insertion. This gauze should then be removed and a transparent film dressing applied. This practice is commonly used because of the absorbent properties of the gauze and ease of application.
Loveday et al (2014) emphasised the critical importance of regularly changing the gauze underneath dressings to prevent infections at the catheter exit site. This study highlighted that gauze dressings can become moist and contaminated with microbial flora, which can increase the risk of infection, and that keeping the exit site dry reduces the potential for microbial colonisation. Jamous et al (2019) also discussed the importance of changing the gauze underneath dressings as it can quickly become saturated with blood or exudate, providing a moist environment conducive to bacterial growth. Additionally, Loveday et al (2014) stressed that dressing integrity must be preserved to protect the site from external contaminants. These two studies reiterate the need for meticulous care and adherence to vascular access device dressing protocols to safeguard patients against infection.
The need to remove the gauze pad 24 hours after PICC insertion puts pressure on nursing resources in both inpatient and outpatient facilities. Patients who have an issue with continuous exit site bleeding may require multiple dressing changes;outpatients may need to make multiple visits to the hospital which can be inconvenient and costly (Dai et al, 2020).
There are some dressings that can be applied over the PICC exit site to control bleeding; these have various levels of success.
Calcium alginate dressings are one such option. Derived from seaweed, they are highly absorbent and promote clotting by interacting with blood to form a gel-like barrier. Their primary actions are to manage wound exudate and promote healing (Qin, 2023). A drawback of calcium alginate dressings is their tendency to adhere to the exit site or wound bed when applied to heavily bleeding sites (Dabiri et al, 2016). This can lead to pain and some trauma when the dressing is removed, potentially causing disruption to the exit site which can restart bleeding. Calcium alginate dressings can become saturated with blood before the mechanism of action has started and, like gauze, can require frequent changing, increasing the risks of exit site exposure and infection (Zhao et al, 2022).
Tissue adhesive has been used for more than 10 years to seal vascular catheter exit sites. Mallory et al (1997) noted it was easy to apply during dressing changes and effective, creating a waterproof seal to reduce the risk of moisture complications. They added, however, that tissue adhesive can cause skin irritation or allergic reactions in some patients and, if not applied correctly, can inadvertently seal the exit site of a catheter, making it difficult to assess this site for early signs of infection or other complications. Pittiruti et al (2022) has published research about the use of cyanoacrylate adhesive to seal vascular access catheter exit sites.
When additional dressings are used to manage exit site bleeding, clinicians should assess the potential for complications associated with infection, skin integrity, dermatological conditions and clinical preferences. These preferences should consider both the patient and the practitioner; the patient may have had previous skin reactions and/or prefer certain dressings, while the practitioner is more knowledgeable in choosing the correct option to minimise complications and ensure optimal care. Therefore, a collaborative approach is essential to minimise catheter disruption and improve patient care.
StatSeal
More recently, a product called StatSeal has been used to manage vascular access catheter exit site bleeding. StatSeal is becoming increasingly recognised as a preferred solution for managing exit site bleeding in central venous access catheters. Published evidence shows its effectiveness for rapid and effective haemostasis after PICC insertion (Biolife, 2024).
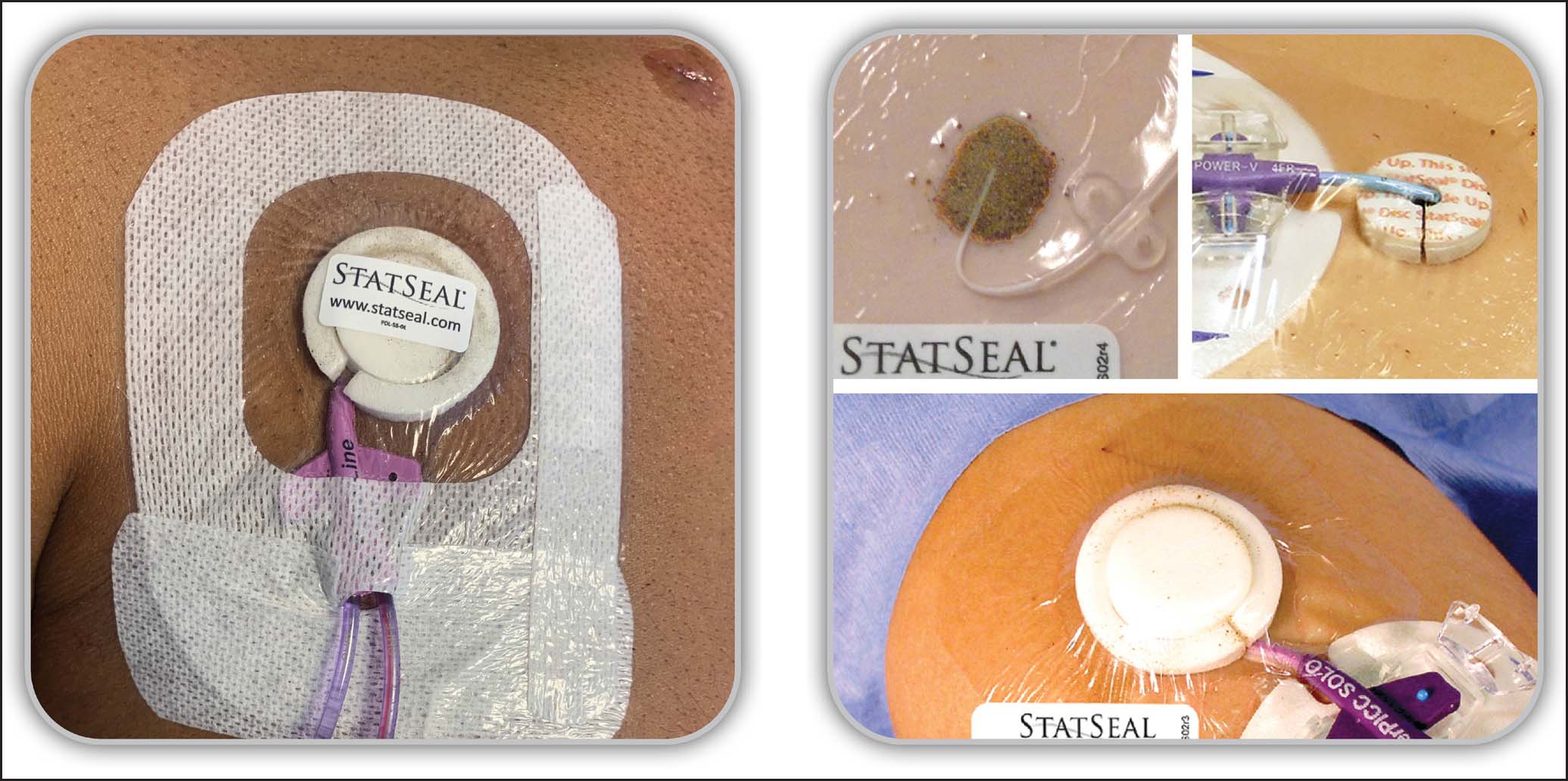
StatSeal (Figure 1) contains a hydrophilic polymer that rapidly dehydrates blood and absorbs exudate, stacking up desiccated blood solids beneath the catheter at the exit site to form a seal. Potassium ferrate binds the blood solids and proteins together, so the seal sticks to the exit site to stop bleeding and oozing (Blough et al, 2010).
Beneath the seal, the pH remains neutral, as the blood solids and proteins continue to stack naturally, reinforcing the seal around the catheter. Above the seal, the hydrophilic polymer exchanges protons for cations, resulting in desiccation, which changes the pH to ~2, creating a hostile barrier to microbial penetration (Biolife, 2024)
In addition to immediate haemostasis minimising the risk of infection, the seal keeps the PICC stable and reduces the need for dressing changes, with the first dressing change being required at day 7.
StatSeal is available as a powder that can be applied to the exit site inside a foam-bordered ring, and as a disc made from compressed powder that can be used on vascular access devices or to seal arterial or venous puncture sites in interventional cardiology or radiology procedures.
StatSeal is compatible with most dressings and easy to apply, which makes it suitable for any healthcare setting. Rapid haemostasis and reduction in dressing disruption and catheter manipulations improve patient outcomes and mean fewer vascular access complications. The inconvenience and potential complications associated with recurrent hospital visits illustrate the importance of effective management at the point of PICC insertion and the use of advanced haemostatic solutions such as StatSeal to control bleeding immediately and remove the need for additional and unnecessary clinic attendance (Mielke et al, 2020).
Specialist vascular access team
The vascular access service team (VAST) at Frimley Health NHS Foundation Trust is a well-established team that operates 08:00–20:00, 7 days a week. This dedicated team of specialist nurses and technicians ensures patients receive timely and expert care for the insertion, maintenance and troubleshooting of all vascular access devices. There is a focus on continued education for staff in the care and maintenance of vascular access devices to reduce harm and provide positive patient outcomes.
Historically, VAST members have found managing exit site bleeding during and after the insertion of vascular access devices a significant challenge, especially with PICCs. They found that exit site bleeding was compromising the sterility of catheter sites, posing a risk to the health of patients who are already vulnerable and affecting the functionality of the catheter, sometimes delaying treatment.
The vascular access team began reviewing literature related to exit site bleeding to investigate what options there were to reduce this complication to zero if possible. Seminal UK studies such as the Matching Michigan programme (Bion et al, 2013) and Richardson et al's (2015) evaluation of central venous catheter dressing durability significantly contributed to their understanding of complications associated with dressing longevity and the impact on reducing complications around catheter associated-infection, pistoning, catheter migration, and medical adhesive-related skin injury (MARSI) in relation to the patient's clinical journey as well as costs implications. Hitchcock et al (2021) also examine MARSI.
Factors contributing to dressing disruption were identified within both projects by Bion et al (2013) and Richardson et al (2015), including patient-specific variables, dressing materials, insertion techniques and staff training. A comprehensive assessment tool and staff training programme were implemented to ensure best practices in all aspects of device care and maintenance. By applying evidence-based interventions, such as standardised dressing protocols and emphasising the importance of educational initiatives for healthcare providers, both projects succeeded in reducing catheter-related bloodstream infection rates. These efforts led to improved patient outcomes and enhanced infection control practices nationwide. Additionally, significant advancements were made in the management of vascular access placement and maintenance.
With all this in mind, the Frimley team was looking for an additional strategy to include in the care and maintenance of vascular access devices that would reduce exit site bleeding and protect the exit site from infection (Giustivi et al, 2024).
StatSeal trial
Implementing StatSeal into the care and maintenance bundle was considered by the Frimley team.
A trial of the product was conducted in the infusion and vascular access unit at Frimley Health from 20 February 2023 to 31 July 2023; the aim was to evaluate the efficacy and safety of StatSeal for haemostasis following PICC line insertion. The trial was conducted on adult inpatients requiring a PICC or outpatients requiring a PICC for chemotherapy or home IV antibiotics.
Sample, assessment and consent
All patients were considered; the only exclusion criterion was a known allergy to the properties of the product. The control group were those not using the StatSeal.
Before PICC placement, all patients underwent thorough assessments for the requirement of a PICC, drug and duration of treatment, and their medical history, including anticoagulation use, dermatological conditions, allergies and any past complications related to PICC insertion, was taken. This meticulous pre-screening process allowed potential risk factors to be identified and ensured patient safety throughout the trial. The trial's protocol emphasised a patient-centred approach, prioritising individualised care and risk assessment to optimise outcomes and minimise adverse events associated with PICC insertion and haemostasis management using StatSeal.
All patients who qualified for StatSeal use were informed about the use of the product and their participation in the trial. After giving consent, they underwent a further assessment to determine the most appropriate StatSeal product, whether this was the disc or powder. This choice depended on the type of PICC securement device being used. Outpatients had a subcutaneous mechanical securement device which is not fully compatible with the StatSeal disc; in these cases, the powder is more effective. For inpatients, PICCs are usually secured using an adhesive device, which is compatible with either preparation.
Ethical approval for the trial of Statseal was not obtained, given that the dressing was already in use in the cardiac catheterisation laboratory at the Wexham Hospital site post angiogram. The trial involved the introduction of a different-sized dressing for central devices post insertion, which necessitated patient consent rather than full ethical approval. This approach ensured compliance with ethical guidelines while facilitating the evaluation of the dressing's efficacy in a clinical setting.
Patient and practitioner education
To ensure proper implementation and use of StatSeal, the first 2 weeks of the trial involved StatSeal clinical staff providing onsite training and support to the vascular access clinical nurse specialists. This included hands-on sessions, with simulation arms and clinical support during PICC insertion.
Patients were given verbal and written information about StatSeal and had the opportunity to ask questions before the product was used.
Face-to-face training sessions were organised for all unit staff in areas where StatSeal would be used for inpatients and outpatients so PICC care and maintenance were consistent. This training and support aimed to enhance clinician confidence and competence in recognising that StatSeal was in use or to use it for reapplication if necessary.
Patient monitoring
During the initial weeks of the trial, all inpatients underwent a comprehensive review 24 hours after PICC line insertion by the VAST to assess the site for any signs of complications or dressing disruption.
For the outpatient oncology or home infection management patients, telephone follow-up was conducted after 24 hours to monitor outcomes, ensuring timely intervention if needed. Subsequently, patients attended the chemotherapy day unit after 48 hours to start treatment, allowing for close monitoring and prompt management of any issues.
All dressing changes within the first 4 weeks were performed by the VAST, ensuring continuity of care and adherence to standardised protocols. After then, all inpatients with PICCs and StatSeal had their dressings changed weekly by the ward/unit nurses. This transition was monitored by theVAST by reviewing the patients’ electronic record and auditing any issues with the PICCs and StatSeal remotely. This systematic approach to follow-up and documentation ensured comprehensive monitoring of patient outcomes, adherence to trial protocols throughout the duration of the study and accurate data collection.
Data collection
Data were collected from each patient where StatSeal was used. This included information on:
Patients were categorised as reported, qualified and disqualified:
Results
During the trial period, 303 patients had PICCs placed. Of these, 96 were disqualified because of death, application error, early discharge/transfer, catheter no longer needed or by patient request. This resulted in 207 qualified patients. Of these 207 qualified patients, 117 (58%) received a StatSeal disc, 60 patients (29%) received StatSeal powder and 30 (14%) did not receive StatSeal (Table 1).
| Patients: inpatient and outpatient | With StatSeal | Without StatSeal | ||
|---|---|---|---|---|
| Disc | Powder | Total StatSeal | ||
| Total patients (n=303) | 179 | 89 | 268 | 35 |
| Qualified patients | 117 | 60 | 177 | 30 |
| Disqualified patients | 62 | 29 | 91 | 5 |
| Reason for disqualification | ||||
| Patient deceased | 11 | 2 | 13 | 0 |
| Application error | 3 | 3 | 6 | 1 |
| Early discharge/transfer | 3 | 1 | 4 | 1 |
| Catheter no longer needed | 43 | 23 | 66 | 0 |
| Patient request | 2 | 0 | 2 | 3 |
Of the qualified patients, 116 (99%) with StatSeal disc had dressings within a 7-day period can be considerable. Given the dressings that lasted 7 days and 60 patients (100%) with StatSeal powder had dressings that lasted 7 days. Only two (7%) whose did not receive StatSeal had dressings that lasted 7 days (Table 2).
| Patients: inpatient and outpatient | With StatSeal | Without StatSeal | ||
|---|---|---|---|---|
| Disc | Powder | Total StatSeal | ||
| Total qualified patients (n=207) | 117 | 60 | 177 | 30 |
| Number that lasted 7 days | 116 | 60 | 176 | 2 |
| Percentage that lasted 7 days | 99% | 100% | 99% | 7% |
Data analysis
The data indicate the effectiveness and reliability of StatSeal in reducing bleeding at the catheter exit site as well as reducing the number of dressing changes required within the initial 7-day care and maintenance cycle.
It was observed that 99% of StatSeal dressings lasted 7 days, and only 1 patient with the StatSeal dressing had an unplanned dressing change due to bleeding. According to Richardson et al (2015), clammy skin and a lack of dressing adherence are more common reasons for unplanned dressing changes. The results may indicate that StatSeal's desiccant properties are also positively impacting these variables and the resulting lack of unplanned dressing changes.
Most dressings that were not in place for the whole 7 days were removed as they were no longer needed and the PICC line was removed (66 cases). They were used for short-term administration of total parental nutrition, vesicant medications or for iloprost infusions (which required an indwelling PICC for 5 days). In addition, 13 patients died.
The data highlight the effectiveness of StatSeal in planned dressing changes and that dressings using StatSeal were more likely to last for 7 days than those without.
Cost analysis
Based on our data, there are potential cost benefits associated with using StatSeal to reduce dressing changes.
The cost of a dressing change includes the cost of supplies and nursing time. We estimated that the cost of supplies for each dressing change (PICC dressing, the dressing removal product, sterile liquid film skin barrier, skin decontamination product, adhesive securement device and a dressing pack) totals £15.24. We also estimated the total cost of nursing time, which includes 30 minutes taken by a band 5 nurse for each dressing change (cost £10.78) and 30 minutes of band 7 nurse time for patient monitoring (cost £15.41). Based on this analysis the total cost of each additional dressing change equals £41.43 (Table 3).
| Nurse band level | Nursing time | Cost | |
|---|---|---|---|
| Dressing change | 5 | 30 min | £10.78 |
| Patient monitoring | 7 | 30 min | £15.41 |
| Dressing change kit | N/A | N/A | £15.24 |
| Total | N/A | 60 min | £41.43 |
Implementing StatSeal into insertion protocols at a cost of £20 per patient eliminates the cost of extra supplies and nursing time, providing a cost savings of at least £21.43 per catheter. From the authors’ experience, many catheters without StatSeal are likely to require multiple unplanned dressing changes.
StatSeal can reduce the risk of central line bloodstream infection, which can incur high - financial costs and the patient's ability to recover by significantly reducing unplanned dressing changes and keeping the sites dry and intact until the scheduled dressing change (Biolife, 2024).
Additional potential cost saving
There are other considerations regarding the use of StatSeal to reduce the number of dressing changes within the 7-day period. Transport costs for outpatients to attend healthcare facilities or for community nurses to travel to patients’ homes to change dressings within a 7-day period can be considerable. Given the varying costs of petrol, public transport, and taxis across the country, accurately totaling these additional expenses is challenging. The use of StatSeal to reduce the number of dressing changes within the 7-day period has significant implications. A reduction in required dressing changes, can minimise the need for patients to travel to clinic appointments, thereby reducing their travel costs and the associated mental and physical burden. Additionally, it frees up district nurse time, allowing for more efficient allocation of healthcare resources. It is important to consider these factors, which contribute to an improved patient experience by decreasing the time patients spend traveling or in hospitals, and by avoiding additional financial burdens on top of their illness
Additional reductions in potential complications
Central line bloodstream infection can incur high financial costs and negatively affect the patient's ability to recover. StatSeal can reduce the risk of this by significantly reducing the need for unplanned dressing changes and keeping the sites dry and intact until the scheduled dressing change (Biolife, 2024). Fewer dressing changes can reduce the risk of skin stripping, MARSI and other complications (Hitchcock et al, 2021).
Conclusion
Using StatSeal improved patient outcomes and reduced the number of dressing changes required in a 7-day period, saving time and money. StatSeal is a reliable, valuable product for the management and control of vascular access catheter exit site bleeding.


