Healthcare uniforms vary both globally and within the UK. Scotland, Wales and Northern Ireland introduced national uniforms between 2010 and 2011, and NHS England has been consulting with staff for years over potentially introducing a national uniform (NHS Supply Chain, 2021). On unveiling the designs of these uniforms in 2023, a common criticism was that nursing roles were poorly delineated within the 15 colourways presented by NHS England (Church, 2023). Due to a similar issue, NHS Scotland introduced a new uniform for nurse leaders or nurse managers in 2018, yet there is still not a specific uniform for advanced nurse practitioners (ANPs) (Scottish Government, 2018).
Uniforms in advanced nursing roles
The argument has been made that distinct uniforms for nurses in advanced roles such as ANPs are of value (Bryson, 2016), and research involving clinical nurse specialists (CNSs) suggest that they prefer not to wear the same uniforms as staff nurses (Timmons and East, 2011).
Uniforms are a visual signifier of occupational boundaries and hierarchical position. This is important in nursing, because there are key role differences between the registered nurse (RN) and the nurse working in advanced clinical practice roles. Formal preparation for these advanced roles, which must include evidence of additional postgraduate (ie masters-level) study and clinical practice aligned to core advanced capabilities, are required across the UK (Health Education England et al, 2017; Scottish Government 2017; 2021; Department of Health Northern Ireland, 2018; Health Education and Improvement Wales, 2023). This may amount to a further 2–3 years of study over and above pre-registration training. Therefore, a distinct uniform may aid role recognition for those working at advanced clinical practice level. There are some examples within the UK where uniforms for specialist nurses and ANPs have been introduced, but this is far from universal. There is a need then, for clarity around how ANPs and other practitioners in advanced roles should be attired.
Aims
As the first phase in a larger programme of work that seeks to evidence the need for clarity around ANP uniforms, this review explores what is already known about people’s perceptions of healthcare uniforms. This includes the following specific objectives:
- To describe the state of the research conducted in this area, including the methods used and the professional roles which have been involved
- To identify common themes in relation to preferences about healthcare uniforms.
Methods
Design
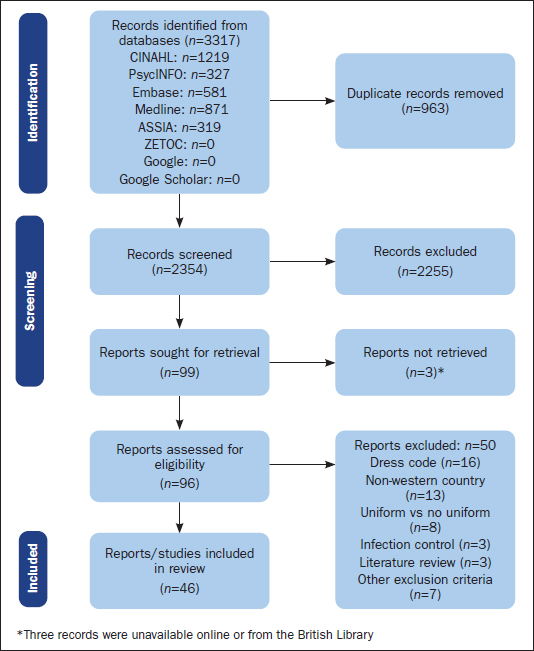
A mixed-methods scoping review following the Joanna Briggs Institute (JBI) guidance (Peters et al, 2020), and reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidance (Page et al, 2021) extension for scoping reviews (Tricco et al, 2018).
Data sources
CINAHL, ASSIA, PsycINFO, and EMBASE were searched from inception in August 2022. The search used key words and MeSH headings combined using Boolean logic. Terms included ‘uniform’, ‘dress code’, ‘clothing’, ‘professional image’, ‘social comparison’,‘social identity’’,‘professional image’,‘professional competence’,‘interprofessional relations’, and ‘social perception’. Retrieved citations were de-duplicated and uploaded to Rayyan (Ouzzani et al, 2016) to facilitate screening and data management. Rayyan is a cloud-based tool that can be used to automate and augment the process of screening citations, although for this review it was used simply to manage citations and log author decisions.
ZETOC (British Library general database), Google Scholar, and Google were also searched for relevant articles using similar terms to those used in the structured searches.
Eligibility criteria
Primary peer-reviewed research using qualitative, quantitative or mixed methods to explore people’s perceptions with different uniforms for registered health professionals were eligible. The authors restricted this to studies undertaken in the Western world (see rationale below) and published in the English language.
Studies that examined the physical properties or design of uniforms or whose primary focus was on infection control were excluded. Similarly excluded were studies that looked at religious and military uniforms, operating theatre wear, and those exploring the effect of uniforms on blood pressure, white coat ceremonies, studies that compared wearing uniform with not wearing uniforms, staff preferences of what to wear, and studies solely focused on dress code. News articles, opinion pieces, editorials and anecdotal accounts were also excluded.
Terminology and definitions
The definitions used here were agreed by consensus among the authors in advance of the study’s commencement.
Uniform
In this review, a uniform is defined as an identifying outfit worn by a health professional in the clinical setting that has been issued or approved by their organisation or employer.
Western world
The term Western world typically refers to countries in Europe, North America, Australia and New Zealand, who have many shared cultural, political and economic characteristics.
A pragmatic decision was taken not to include Türkiye in this review, although it is part of Europe, owing to the wide range of both European and Arab cultural influences that may affect how uniforms are perceived. Some definitions of Western world may include countries in Africa or South America, however the authors restricted the definition to the countries listed above. There is no unifying definition of the Western world, and any such definition is constructed with reference to countries that are not included (ie the ‘West vs the rest’) (McNeill, 1997). This debate is beyond the scope of this project, therefore the authors adopted alternatives pragmatic definition to satisfy the aims of the review.
Study selection process
Rayyan (Ouzzani et al, 2016) was used to manage and screen citations. Following a pilot test, titles and abstracts were screened by three authors, who each independently applied inclusion/exclusion criteria. Full-text papers were retrieved for all eligible records. Disagreements regarding inclusion were discussed among authors and a consensus decision made.
Results
Search outcome
The search outcome is detailed in Figure 1. Forty-six reports were included in the review.
Overview of the included studies
The studies included in the review are summarised in Table 1. They were published between 1991 and 2021; most (70%, n=32) were conducted in North America and the remainder in Europe, including the UK (n=11), Italy (n=2), and Switzerland (n=1).
| Study/location | Professional group | Patient group |
|---|---|---|
| Aitken et al, 2014, UK | Doctors | Adult: outpatients |
| Au et al, 2013, Canada | Doctors | Adult: inpatients |
| Bauer et al, 2020, USA | Doctors | Paediatric: outpatients |
| Cha et al, 2004, USA | Doctors | Adult: outpatients |
| Cham et al, 2023, USA | Doctors | Paediatric: Inpatients (views of parents only) |
| Del Rey and Paul 1995, USA | Doctors | Paediatric: outpatients (emergency department, views of parents only) |
| Gherardi et al, 2009, UK | Doctors | Adult: outpatients |
| Jennings et al, 2019, USA | Doctors | Adult: inpatients |
| Lands et al, 2019, USA | Doctors | Adult: outpatients |
| Lightbody and Wilkie, 2013, UK | Doctors | Adult: inpatients and outpatients |
| Petrilli et al, 2018, USA | Doctors | Adult: inpatients and outpatients |
| Xun et al 2021, USA | Doctors | Adult: general population |
| Zollinger et al, 2019, Switzerland | Doctors | Adult: outpatients |
| Clarke et al, 2019, UK | Doctors/nurses | Paediatric: outpatients (emergency department) |
| Albert et al, 2008, USA | Nurses | Adult and paediatric: inpatients and outpatients |
| Campbell et al, 2000, UK | Nurses | Paediatric: outpatients (only clinical staff and families involved) |
| Clavelle et al, 2013, USA | Nurses | Adult: inpatients |
| Festini et al, 2009, Italy | Nurses | Paediatric: inpatients |
| Kaser et al, 2009, USA | Nurses | Adult: inpatients |
| Lehna et al, 1999, USA | Nurses | Nurses (one student and one patient) |
| Livingston 1995, UK | Nurses | Paediatric: inpatients and outpatients |
| Mangum et al, 1991, USA | Nurses | Adults: inpatients |
| Mangum et al, 1997, USA | Nurses | Adults: inpatients and outpatients |
| Meyer 1992, USA | Nurses | Paediatric: outpatients |
| Miller et al, 2010, USA | Nurses | Adult: inpatient |
| Newton and Chaney 1996, USA | Nurses | Nursing faculty and students |
| Pearce et al, 2014, USA | Nurses | Inpatients: unclear if exclusively adults |
| Porr et al, 2014, Canada | Nurses | Adult: inpatients |
| Rowland 1994, UK | Nurses | Adult and paediatric: primary care |
| Sanna et al, 2020, Italy | Nurses | Paediatrics: inpatients and outpatients |
| Shaw and Timmons 2010, UK | Nurses | Nursing students only |
| Skorupski and Rea 2006, USA | Nurses | Adult: inpatients |
| Sutherland et al, 2013, Canada | Nurses | Adult and paediatric: inpatients and outpatients |
| Thomas et al, 2010, USA | Nurses | Adult: inpatients |
| West et al, 2016, USA | Nurses | Adult: inpatients and outpatients |
| Windle et al, 2008, USA | Nurses | Adult: inpatients |
| Wittmann-Price et al, 2011, USA | Nurses | Adult: inpatients |
| Wocial et al 2014a, USA | Nurses | Unclear: described as ‘healthcare consumers’ |
| Wocial et al 2014b, USA | Nurses | Nurses only: working across adult, paediatric, inpatient and outpatient settings |
| Wocial et al, 2010, USA | Nurses | Paediatric: inpatients and outpatients |
| Baxter and Pride 2008, UK | Midwives | Adult: inpatients (postnatal) |
| Timmons and East, 2011 UK | Nurses/ allied health professionals | Clinical staff from adult and paediatric settings. Patients only adults from hospital patient involvement group |
| Ingram et al, 2011, USA | Physiotherapists | Adult: inpatients and outpatients |
| Tadros et al, 2021, USA | Dietitians | Adult: general population |
| Kelly et al, 2014, USA | Dentists | Paediatric: outpatients (orthodontic clinic, parents provided responses) |
| Mistry and Tahmassebi 2009, UK | Dentists | Adult and paediatric: outpatients (dental clinic) |
NB. Full details of the studies included are available online
Three-fifths of studies examined or included nursing uniforms (n=28), one third involved medical staff (n=14), and a small number explored uniforms for other healthcare staff (dentists/dental students, n=2; midwives, physiotherapists, dietitians, n=1 each). One study examined non-medical staff (nurses, midwives and allied health professionals (AHPs)).
Most studies focused on uniforms worn by clinicians working with adults (n=25), a smaller number were based in paediatric settings (n=11), and four studies covered both adult and paediatric settings. The remaining six either did not specify the age of the patient group or were limited to other groups such as nursing students or nursing faculty. There was a more even spread between inpatient (n=15), outpatient (n=12), or combined settings (n=10), with the remainder being either non-specific or set in primary care or the general population.
Most studies employed quantitative (n=33) or mixed-methods approaches (n=5). Of these, 30 involved rating standardised photographs of practitioners in different uniforms, occasionally using validated scales such as the Nurse Image Scale or a modified version of it (n=4).
Nurses
Twenty-seven studies explored nursing uniforms (Table 1). These studies used diverse methods, although around half (n=13) used standardised photographs within the study design.
Being able to identify a nurse by what they wear was seen as important (Lehna et al, 1999; Campbell et al, 2000; Shaw and Timmons, 2010; Clavelle et al, 2013; Sutherland et al, 2013; Pearce et al, 2014; Sanna et al, 2020), as was being able to differentiate the nurse-in-charge (Campbell et al, 2000). Participants in one study felt nurses were sufficiently identifiable due to a large print ‘RN’ (registered nurse) badge/tag (Albert et al, 2008).
Patients often did not mind what nurses wore (Windle et al, 2008; Miller et al, 2010; Pearce et al, 2014), although white uniforms were preferred in seven studies (Mangum et al, 1991; Livingston 1995; Mangum et al, 1997; Skorupski and Rea, 2006; Albert et al, 2008;Wittmann-Price et al, 2011; Porr et al, 2014); this preference sometimes increased with participant age (Newton and Chaney, 1996; Skorupski and Rea, 2006; Albert et al, 2008). Conversely, patients in one study (Clavelle et al, 2013) were found to be not in favour of all-white uniforms and agreed that nurses should be allowed to wear any colour.
A traditional uniform (eg dresses, occasionally caps) was popular with participants in older studies (Mangum et al, 1991; 1997; Rowland, 1994; Newton and Chaney, 1996); however, scrubs or tunic tops were preferred by respondents in more recent studies (Kaser et al, 2009;Thomas et al, 2010; Pearce et al, 2014; West et al, 2016).
Pearce et al (2014) found that nurses had a preference for navy blue uniforms (71%); although patients in this study did not have a strong preference, the most popular colour was blue (22%). In another study, navy blue scrubs were preferred over other options (West et al, 2016). In another study (Wocial et al, 2014a) the colour red was preferred, although this was probably related to the corporate branding of the hospital. Red was the least preferred colour for patients in another study (Kaser et al, 2009).
A context where differences may exist are mental health inpatient units. Miller et al (2010) found that this patient group did not have a strong preference for the type of attire worn by staff. However, identification of nurses was important, and 29% of respondents thought that street clothes made the nurse less approachable.
Several studies involved children. In one study from the 1990s, 41% of children found the traditional white uniform frightening (Meyer, 1992). In contrast, a UK study found that both parents and children preferred the traditional white uniform (Livingston, 1995), although parents were more accepting of alternatives. In more recent studies, children and adult visitors stated a preference for uniforms consisting of a boldly printed top and blue or white trousers (Wocial et al, 2010) or multicoloured uniforms (Sanna et al, 2020).
Only one study made specific mention of clinical nurse specialists, and none discussed nurse practitioners or advanced nurse practitioners. This study, by Timmons and East (2011), involved 30 patients, nurses, physiotherapists and occupational therapists in a focus group with the aim of analysing a change of uniforms in one hospital. Ward nurses were generally comfortable with the change, but the clinical nurse specialists thought it was an attack on their status.
Doctors
Fourteen studies explored physician attire (Table 1).All of these studies involved a survey in which respondents were asked to rate standardised photographs of staff in different clothing, with the exception of one study that explored both nursing and medical attire (Clarke et al, 2019). In the studies that looked solely at doctors’ attire, the subjects were depicted in the photographs both with stethoscopes (Del Rey and Paul, 1995; Gherardi et al, 2009; Au et al, 2013; Jennings et al, 2019) and without (Cha et al, 2004; Lightbody and Wilkie 2013; Aitken et al, 2014; Petrilli et al, 2018; Lands et al, 2019; Zollinger et al, 2019; Bauer et al, 2020; Xun et al, 2021; Cham et al, 2023).
Most studies found that people preferred medical staff to be in a white coat (Del Rey and Paul, 1995; Gherardi et al, 2009; Au et al, 2013; Lightbody and Wilkie, 2013; Aitken et al, 2014; Petrilli et al, 2018; Lands et al, 2019; Zollinger et al, 2019; Bauer et al, 2020; Xun et al, 2021; Cham et al, 2023). However, scrubs were seen as an acceptable alternative in certain settings, for example where clinical procedures were performed (Del Rey and Paul, 1995; Cha et al, 2004; Gherardi et al, 2009; Au et al, 2013; Lightbody and Wilkie, 2013; Petrilli et al, 2018; Clarke et al, 2019; Jennings et al, 2019; Cham et al, 2023). White coats worn with scrubs were preferred in inpatient settings (Cha et al, 2004; Lightbody and Wilkie, 2013; Zollinger et al, 2019).
Bauer et al (2020) reported that children and parents did not have a strong preference towards surgeon’s attire, but (in keeping with other studies) there remained a general preference for doctors to wear white coats (Del Rey and Paul, 1995; Clarke et al, 2019). This ‘uniform’ for doctors was associated with qualities such as competence, confidence, feeling safe, caring, trustworthiness, and feeling comfortable (Bauer et al, 2020), while scrubs were generally perceived as friendlier and less formal (Clarke et al, 2019).
Doctors were not always easily recognised as doctors when wearing scrubs (Lightbody and Wilkie, 2013). Parents did however prefer scrubs for when children had surgical emergencies and in neonatal critical care where clinical procedures were routinely performed (Del Rey and Paul, 1995; Cham et al, 2023).
Allied health professionals
Ingram et al (2011) looked at 193 patients’ preferences for the uniforms of physical therapists in terms of practicality and patient confidence: they found that patients preferred their physical therapists to wear less formal and more practical attire. The impact of dietitian attire was explored by Tadros et al (2021). The study concluded that type of attire and white coat did not influence overall perceived professionalism of a dietitian.
One UK study that involved several professional groups, including physiotherapists and occupational therapists, explored a recent move by one health board to standardised uniforms (Timmons and East, 2011). Allied health professionals felt that these uniforms were an attack on their identity, and led to misidentification. This study was conducted in England, although it is worth noting that all allied health professionals in Scotland wear variations on two similar shades of blue as national uniform policy.
Dentists
Two studies examined dentists’ attire (Mistry and Tahmassebi, 2009; Kelly et al, 2014), with the overall conclusion that patients prefer formal attire. Kelly et al (2014) asked parents (n=77) whose children were attending an orthodontist for the first time to rate their preference for clinical attire. The results found that casual dress without a name tag was the least preferred, and that either formal attire (eg a buttoned blouse or shirt, and a tie for men) or scrubs (both with a name tag) were the preferred styles.
Mistry and Tahmassebi (2009) assessed child (n=100) and parental (n=100) preferences for dental attire. A significant difference was noted, with parents preferring formal attire and children informal clothing.
Midwives
A single study explored uniforms for midwives (Baxter and Pride, 2008). Fifty-three percent of the women in postnatal care agreed that how the midwife dressed was important. The women favoured a nurse-type uniform in postnatal care (42%), the midwives own clothes in antenatal care (45%), and scrubs during labour (64%).
Discussion
Preferences in relation to healthcare uniforms are diverse and depend on context. Taking the example of white uniforms (and coats), there are examples of adults responding positively and negatively to this colour, with a similar diversity noted for children. The formality of a uniform is more clearly divided by age, with adults preferring formality and children more casual attire. For doctors, the white coat remains the general preference in the eyes of patients. In the USA, the white coat is a powerful symbol of seniority among medics. On graduating from medical school, doctors in their first year of practice wear a short coat, aspiring to the longer white coat of senior colleagues (Hochberg, 2007); however, some training programmes are moving away from this tradition (Mahoney, 2018). Differentiating nurses from other professions is important, but so is identifying the nurse in charge and nurses in advanced practice roles, where both fundamental and advanced nursing care may be provided by one individual.
Patients want uniforms that allow easy identification of the different professions, and both patients and nurses want to be able to identify seniority among nurses. On a basic level, it could be argued that, once the fundamental needs of comfort, hygiene and practicality have been met, the sole purpose of a clinical uniform should be to allow such distinction of roles to be made. Reflecting on the more immediate challenges faced by healthcare services, Oliver (2021) argues that uniforms are of relatively low priority.
Yet symbols matter in healthcare, otherwise why would patients have a preference for white coats, or clinical nurse specialists feel undermined by being made to wear the same uniform as staff nurse colleagues? Neither uniform materially changes the wearer, nor does a uniform possess physical properties that are essential to the task at hand (such as a soldier’s camouflage or a firefighter’s helmet). A healthcare uniform permits instant identification of the wearer’s status and is a symbol of training and competency. As seen in several studies, patients associated positive attributes with certain uniforms, such as competence, trustworthiness or friendliness (Clarke et al, 2019; Bauer et al, 2020).
In a busy clinical area, the ability of uniforms to quickly and subtly communicate professional role and status may often go unnoticed. This cognitive shorthand relies on the observer drawing on their social and cultural experiences, and to have a concept of ‘nurse’ or ‘doctor’ that they can compare with the individuals they encounter. There are a few areas where clarity is more important, for example in the case of newer and less familiar roles, such as ANPs.
Implications for practice
Individuals who are required to wear uniforms have little influence over their attire. However, being aware of what this attire is communicating to patients and colleagues is important. People’s perceptions of what healthcare uniforms convey should be taken into account when uniforms are introduced or changed.
Implications for research
Most of the research was carried out in the USA and is arguably out of date. Given that preferences in relation to uniforms are contextually dependent and likely to be shaped by sociocultural factors, the importance of locally relevant and up-to-date research is clear. More methodological diversity was present in studies of nursing uniforms than in those that explored uniforms for other professions, and the subjective nature of individual preferences is particularly suited to triangulated mixed methods, where the underlying qualities of quantitative values can be interrogated. Such approaches should be adopted in future.
The issue of badges also merits further attention: one study found that large badges were an effective tool for identification of nursing staff (Albert et al, 2008). Campaigns such as ‘Hello, my name is…’ (which aimed to encourage health professionals to introduce themselves before providing care, including by wearing name badges) have been widely adopted throughout the NHS (Kmietowicz, 2015). The effect of these interventions on the perceptions of patients and colleagues merits further exploration.
Strengths and limitations
The scoping methodology employed in this review is a strength. Inclusive eligibility criteria ensured that a wide variety of clinical settings were represented, as was a range of stakeholders. However, the interpretation of these findings should take into account two limitations: the age of the evidence and the context in which the studies were conducted. The majority of studies (74%) were carried out in North America, where white coats are much more commonly worn than in the UK, where infection control policies have all but removed them from practice entirely. In addition, given that most studies were more than 10 years old, it is important to reflect on how attitudes change over time and whether standards of formality may have shifted. For example, before the coronavirus pandemic, the attire of GPs in the UK was generally formal, but has since moved towards wearing scrubs for reasons of infection prevention and control. More recently, the issue of physician associates – and whether the public can distinguish them from doctors – has also been debated extensively in the media and among professional groups in the UK. Neither of these contemporary issues were identified in this review, but they will be important to future research in this field.
Conclusion
Healthcare uniforms fulfil many roles: they should be comfortable, practical, hygienic, and allow patients and colleagues to identify the profession and role of the person wearing the uniform. Yet opinions on the style, formality and colour of these uniforms is extremely varied. The way uniforms are understood is likely to be contextually dependent and culturally mediated, and practitioners should be mindful of how this may affect communication. Decisions about what health professionals wear should in part be based on what the uniform communicates to others, both colleagues and patients.
KEY POINTS
- Standardised uniforms have or are being introduced within the NHS across the UK
- Healthcare uniforms help people to identify different roles
- Varied findings suggest that preferences for healthcare uniforms may be context specific and people associate trust, confidence and competence with different uniforms
- It is important to consider how the attire worn by health professionals is perceived by others
CPD reflective questions
- Do you associate different characteristics with people based on what they wear?
- What assumptions do you think that people make when they at look the clothes you wear at work?
- How easy do you find it to identify different roles in a healthcare setting, ie which roles wear different uniforms in your own workplace?
- If you wear a uniform what does your uniform mean to you?


