Peripheral vascular catheters (PVCs) are the most commonly used vascular access devices in hospital. They are fundamental for administration of medication and fluids as part of the treatment and management of most patients, and it is estimated that around 70% of hospitalised patients require a PVC (Marsh et al, 2018); in the UK, 1 in 3 will have at least one PVC (Zhang et al, 2016). Inserting a PVC is a painful experience for the patient, and can lead to increased anxiety and stress, with the risk of associated complications such as haematoma, phlebitis, infiltration/extravasation injury and bloodstream infection. Because of the potential risks and associated complications, guidelines for prevention and management were developed in the USA (O'Grady et al, 2002) and these recommended that PVCs should be replaced every 72-96 hours and removed sooner if no longer needed. Available evidence at the time suggested that routine replacement reduced the risk of phlebitis and bloodstream infection. However, in 2002 the US Healthcare Infection Control Practices Advisory Committee/Centers for Disease Control and Prevention (CDC) tempered this with:
‘If sites for venous access are limited and no evidence for phlebitis or infection is present, peripheral venous catheters can be left in place for longer periods, although the patient and the insertion sites must be closely monitored.’
Based on the 2002 guidelines (updated in 2011 but keeping the 72–96 hours timeframe for PVCs in adults (O'Grady et al, 2011) the policy in the authors' hospitals up to October 2017 was to routinely remove PVCs after 72-96 hours to reduce risks and complications. Updated guidelines (Loveday et al, 2014) now recommend that PVCs should only be re-sited when clinically indicated and not routinely, unless device-specific recommendations from the manufacturer indicate otherwise; the guidelines recommend duration of 7-10 days for PVCs. The standards from both the Royal College of Nursing (2016) and Infusion Nurses Society (2016) endorse this recommendation.
A recent Cochrane review of the available evidence found no clear difference between clinically indicated removal and routine replacement in rates of bloodstream infection from any cause, including catheter-related bloodstream infection (CRBSI), and phlebitis (Webster et al, 2019). The review also noted that replacement may not be necessary if the PVC is functional and there are no signs of complications. In addition, a study by Marsh et al (2018) found that PVCs are associated with a pooled proportion for phlebitis of 36% and CRBSI of less than 0.1%. Implementing clinically indicated removal would spare patients unnecessary pain and discomfort and provide cost savings because the costs associated with routine replacement can be considerable (Rickard et al, 2010; Loveday et al, 2014; Webster et al, 2019).
As a result of the 2014 epic 3 recommendation (Loveday et al, 2014) a policy change was approved, and clinically indicated removal of PVCs was implemented in the authors' hospitals, in October 2017 at Princess Royal University Hospital (PRUH) and January 2018 at the King's College Hospital Denmark Hill site (DH). Between March and July 2019—18 months after implementation at PRUH and 15 months after at DH—500 PVCs were audited to evaluate the impact of the change by looking at a number of care elements (Box 1) but focusing on:
Method
In 2015, before the policy change, a proposal was presented to the intravenous (IV) catheter steering group to seek agreement for a small-scale trial of clinically indicated removal, the aim of which was to determine whether there was an increase in phlebitis/infection rates or other complications related to clinically indicated versus routine removal/re-siting of PVCs. Subsequent meetings and discussions were held with other stakeholders to formulate a plan of action with a view to implement if the outcome of the trial was favourable. A 28-bed ward in the surgical division was identified for the trial, and two point prevalence audits were conducted on separate days within a 2-week period during November 2016. A total of 30 PVCs were audited of which 93% (n=28) had a VIP score (Jackson, 1998) of 0, and 7% (n=2) had a score above 0; one on day 1 (VIP 2) and one on day 5 (VIP 3). VIP is a tool used in practice to monitor PVC sites every shift for signs of phlebitis and facilitates timely removal when complications arise. All staff in the surgical division were fully informed, and the trial took place over a 3-month period (December 2016 to March 2017).
Results and details were collated by the surgical matron and a report presented to the IV catheter steering group in April 2017. The report was subsequently presented to the Trust hospital-acquired infection operations committee with recommendations for approval to implement on the PRUH site, and after 6 months at the main DH site if there was no reported increase in complications. In October 2017 the IV policy for removal/re-siting was changed from 72–96 hours to 240 hours' duration and implemented at the PRUH, and 3 months later at DH. This was on the condition that three criteria were all met: the PVC is patent, has a VIP score of 0 and is still needed. If the PVC is still needed after 240 hours, the dwell time can be extended if the first two criteria are met. In addition, the Vessel Health and Preservation (VHP) framework was launched trust-wide in the first quarter of 2018 to increase staff knowledge and improve patient experiences and outcomes. VHP is a vascular access selection and decision-making framework that provides timely intentional IV access for patients in the first 24 hours, followed by insertion of a clinically appropriate device within 48 hours (Hallam et al, 2016).
Over a 5-month period (5 March to 31 July 2019), 500 PVCs (250 for each site) were audited on non-consecutive weekdays across a range of departments/specialities including surgery, medicine, renal, cardiac, critical care and haematology/oncology at the PRUH and DH sites. The aim was to capture a sufficient quantity of PVCs to represent dwell-time range for better comparison, and to assess the efficacy of the change from routine removal/re-siting to clinically indicated removal in relation to complications, primarily phlebitis using the VIP scoring tool.
Results
In all, 500 PVCs were audited and grouped into number of days in situ (0-3, 4-7, 8-10, >10), actual and documented VIP score (0, 1, >1) and need for the device (Table 1). Of the 500 PVCs 31% (n=155) were in situ for more than 3 days with a range of 4-22 days; 92% (n=460) were visually observed and assessed to have a VIP score of 0. However, only 72% (n=360) were documented with a VIP score of 0, and 84% (n=420) had an identified clinical need.
| Duration | VIP score/clinical need/dressing | Actual | Documented |
|---|---|---|---|
| 0–3 days (n=345) | VIP 0 | 323 | 239 |
| VIP 1 | 12 | 1 | |
| VIP >1 | 10 | 0 | |
| VIP not recorded | 105 | ||
| Needed | 307 | ||
| Not needed | 38 | ||
| Compromised dressing | 55 | ||
| Optimal dressing | 290 | ||
| 4–7 days (n=119) | VIP 0 | 107 | 95 |
| VIP 1 | 8 | 0 | |
| VIP 1> | 4 | 0 | |
| VIP not recorded | 24 | ||
| Needed | 94 | ||
| Not needed | 25 | ||
| Compromised dressing | 26 | ||
| Optimal dressing | 93 | ||
| 8–10 days (n=25) | VIP 0 | 20 | 20 |
| VIP 1 | 3 | 1 | |
| VIP >1 | 2 | 0 | |
| VIP not recorded | 4 | ||
| Needed | 13 | ||
| Not needed | 12 | ||
| Compromised dressing | 7 | ||
| Optimal dressing | 18 | ||
| >10 days (n=11) | VIP 0 | 10 | 6 |
| VIP 1 | 1 | 0 | |
| VIP >1 | 0 | 0 | |
| VIP not recorded | 5 | ||
| Needed | 6 | ||
| Not needed | 5 | ||
| Compromised dressing | 3 | ||
| Optimal dressing | 8 |
Duration
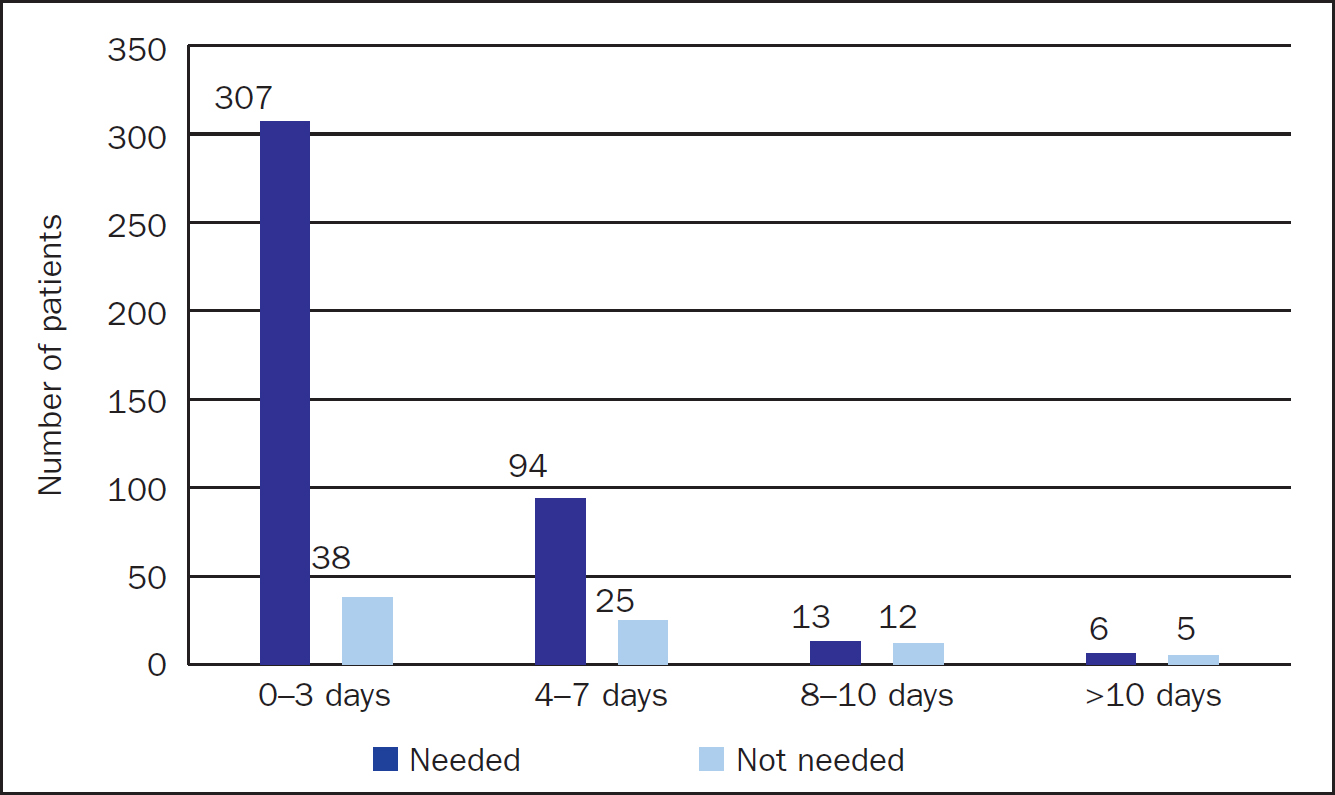
To align with current guideline recommendations, the policy was changed from 72–96 hours (3–4 days) to 240 hours (10 days) but stipulates removal when no longer needed (therapy is completed), or when there is a clinical indication (VIP score >1). As shown in Figure 1, 69% (n=345) of the PVCs audited were in situ for up to 3 days, 24% (n=119) for 4-7 days, 5% (n=25) for 8-10 days and 2% (n=11) for more than 10 days, with a range of 11-22 days. The longest duration of 22 days was at the PRUH and 19 days was the longest dwell time at DH; both had a VIP score of 0.
VIP score
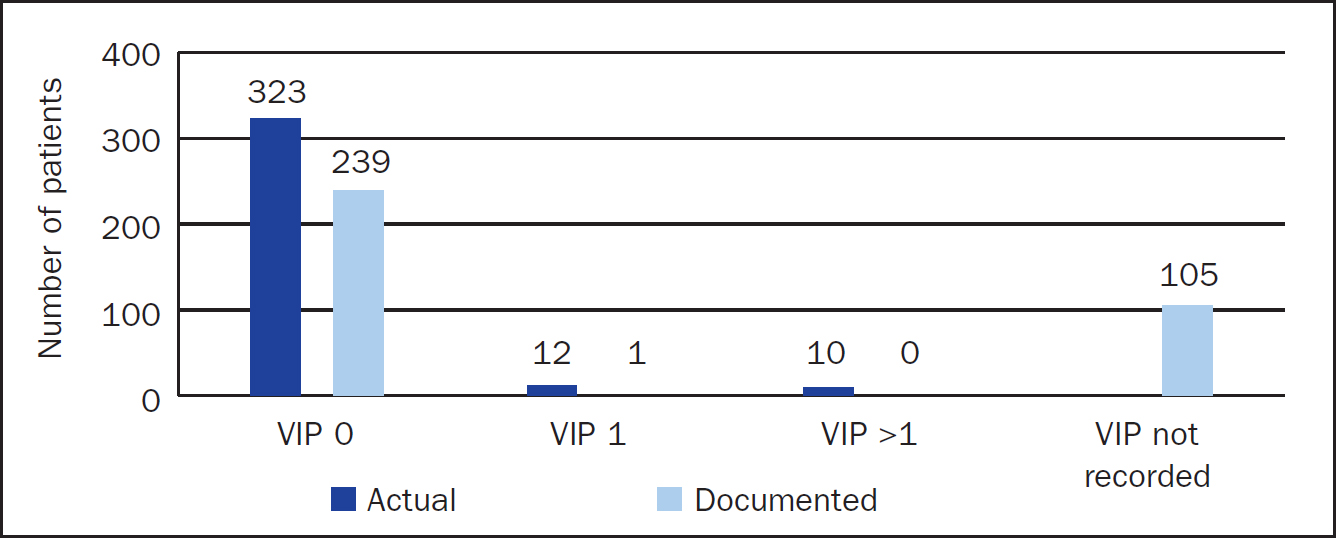
Assessment and monitoring of PVCs is important in recognising early signs of phlebitis and other complications, which should be recorded using the VIP scoring tool. Of the numbers of PVCs audited, 92% (n=460) were observed to have a VIP score of 0, 4.8% (n=24) had a VIP of 1 and 3.2% (n=16) a VIP of >1 (range 1-2) (Figure 2). However, only 72% (n=360) of the PVCs had a VIP score of 0 documented on the electronic patient record (EPR) system, and 0.4% (n=2) a VIP of 1. The remaining 27.6% (n=138) did not have a VIP recorded on EPR, which would indicate that PVCs were not documented at time of insertion on the system to generate an observation form, or they were not monitored consistently.
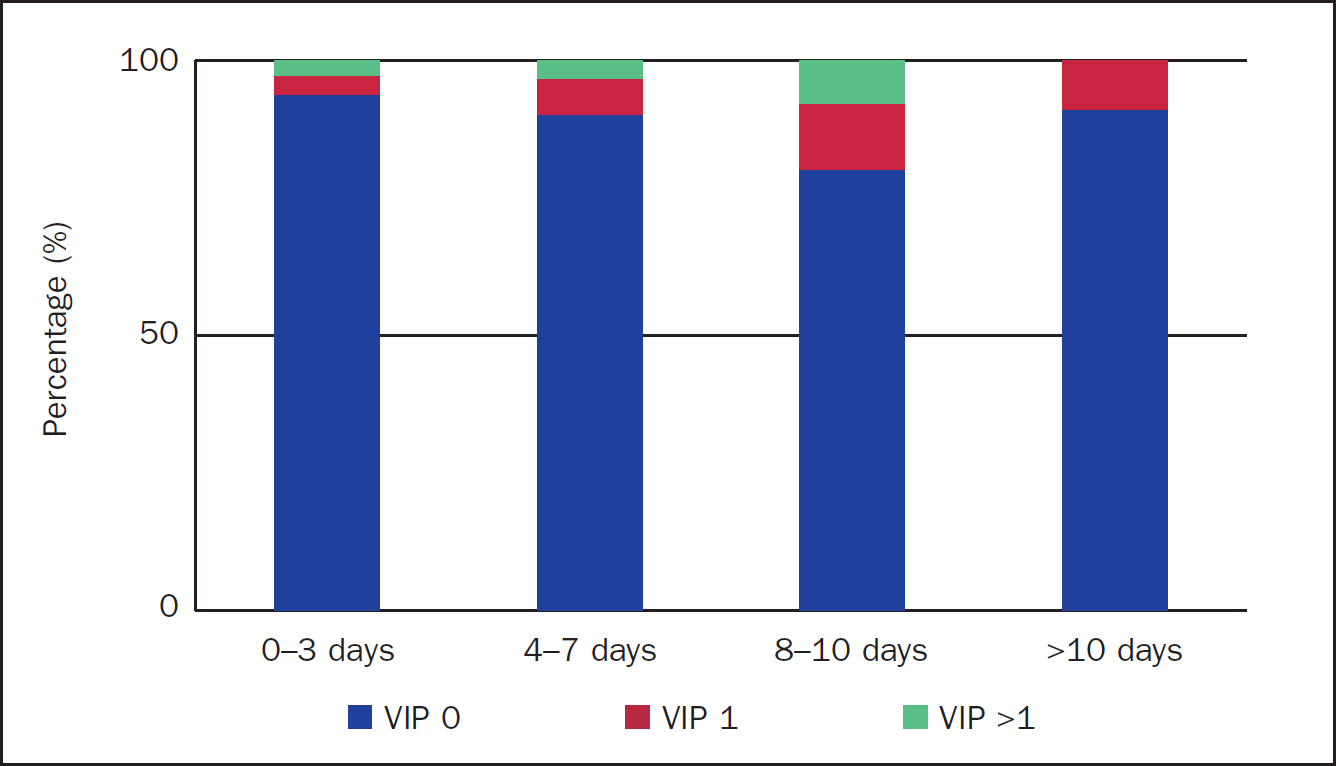
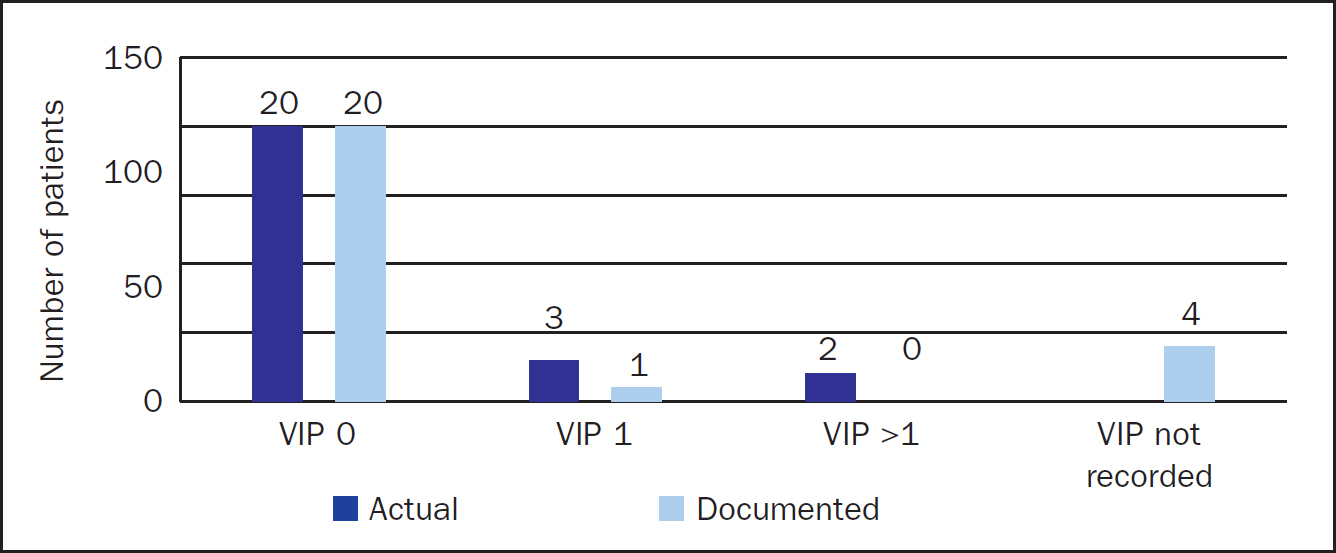
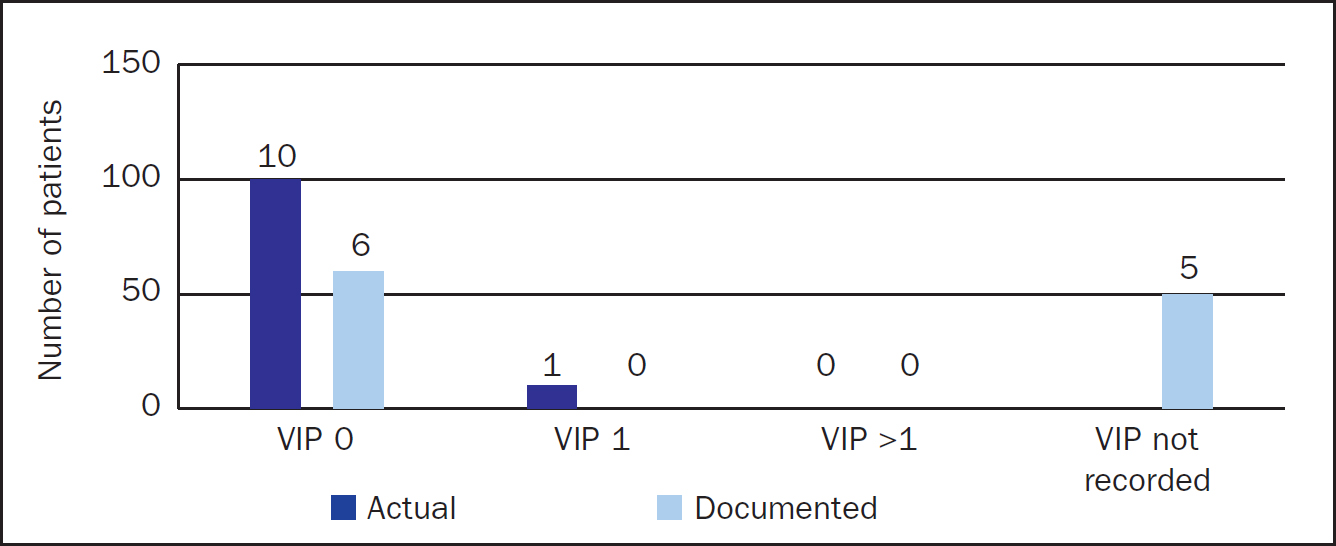
Focusing on actual VIP scores, 93.6% (n=323) of PVCs in the 1-3 days group had a VIP score of 0, 3.5% (n=12) VIP score of 1 and 2.9% (n=10) VIP score of >1 (Figure 3). PVCs in the 4-7 days group had 89.9% (n=107) with VIP 0, 6.7% (n=8) with VIP of 1 and 3.4% (n=4) with VIP >1 (Figure 4). PVCs in the 8-10 days group had 80% (n=20) with VIP of 0, 12% (n=3) VIP 1 and 8% (n=2) VIP >1 (Figure 5). Interestingly, of 11 PVCs in the >10 days group, 91% (n=10) had a VIP 0 and 9% (n=1) VIP 1; none had a VIP >1 (Figure 6).

Need for device
Current evidence-based guidelines recommendations and hospital policy state that PVCs should be removed as soon as they are no longer needed. Although 84% (n=420) of the PVCs audited were needed, 16% (n=80) had no indicated need and should have been removed. The audit found that 89% (n=307) of PVCs in situ for 0-3 days and 79% (n=94) those in situ for 4-7 days were still needed (Figure 7). However, only 55% (n=19) of those in situ for more than 7 days were needed, with 47% (n=17) not needed.
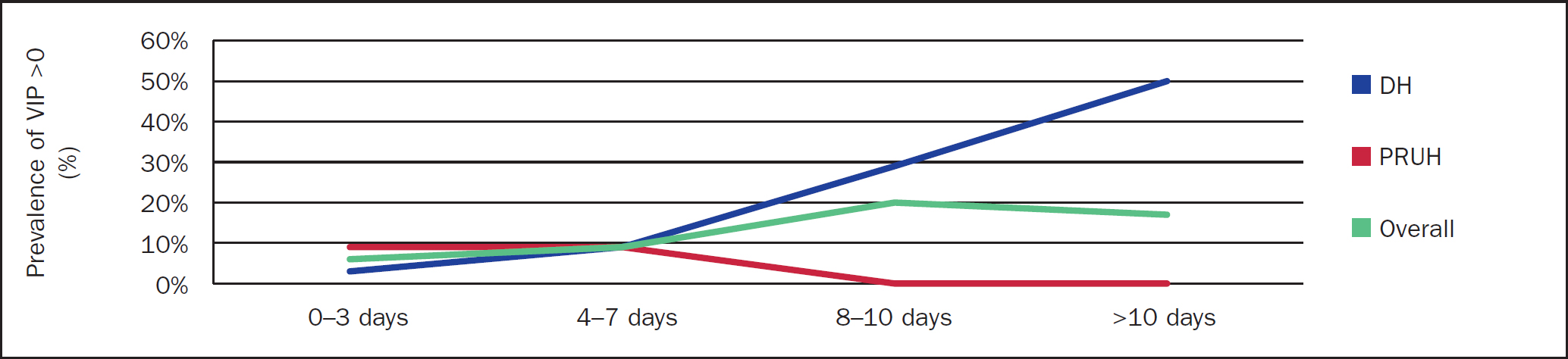
Comparison between sites
The overall prevalence of phlebitis was 8% (Table 3), but when analysed by site the trend varies. The overall prevalence is similar on both sites (7% and 9% respectively), with a wide variation for PVCs in situ for 8 days or longer (Tables 4 and 5). The combined overall analysis indicates that the longer dwell time increases prevalence of a higher VIP score (Figure 8).
| Days in situ | VIP>0 | VIP 0 | % |
|---|---|---|---|
| 1–3 | 22 | 323 | 6% |
| 4–7 | 12 | 107 | 10% |
| 8–10 | 5 | 20 | 20% |
| >10 | 1 | 10 | 9% |
| Total | 40 | 460 | 8% |
| Days in situ | VIP>0 | VIP 0 | % |
|---|---|---|---|
| 1–3 | 17 | 163 | 9% |
| 4–7 | 5 | 49 | 9% |
| 8–10 | 0 | 8 | 0% |
| >10 | 0 | 8 | 0% |
| Total | 22 | 228 | 9% |
| Days in situ | VIP>0 | VIP 0 | % |
|---|---|---|---|
| 1–3 | 5 | 160 | 3% |
| 4–7 | 6 | 58 | 9% |
| 8–10 | 5 | 12 | 29% |
| >10 | 2 | 2 | 50% |
| Total | 18 | 232 | 7% |
Discussion
It is estimated that more than a billion PVCs are used globally each year and, although it is difficult to fully understand the impact of negative patient experiences and overall cost, it is important to take steps to minimise both. It is recommended that hospitals consider implementing clinically indicated removal, which would allow 1 in 2 patients to complete a course of treatment with a single PVC, as opposed to 1 in 5 with routine replacement (Loveday et al, 2014). The recent systematic review of clinically indicated removal versus routine replacement (Webster et al, 2019) found no clear difference in complication rates between clinically indicated removal and routine replacement. The reviewers also found that cost can be significantly reduced and patient satisfaction increased when hospitals move from routine replacement to clinically indicated removal.
The combined results of this prevalence audit (undertaken at the authors' hospitals to evaluate the move to clinically indicated removal) suggest that a longer PVC dwell time increases the prevalence of a higher VIP score. However, there is a wide variation in trends when the data are analysed for the individual sites. At the PRUH site there is no difference in the prevalence of VIP scores >0 between 1-3 and 4-7 days (9%), and for PVCs >7 days (range 8-22) the prevalence was 0%. This would suggest that on this site the risk of phlebitis/complications decreased when routine replacement was replaced with clinically indicated removal—consequently, a better experience for patients. Conversely, at the DH site the trend shows longer dwell time is more likely to have an increased prevalence of a higher VIP score; this trend is linear and strong. However, the prevalence is lower for shorter dwell time at 3% for PVCs in situ for 1-3 days, and 9% (similar to the PRUH) for those in situ for 4-7 days.
It is difficult to determine what influences the variation in results, but factors that could be considered include assessment and monitoring, patient demography, medical condition/diagnosis, type of IV therapy etc. Despite the wide variation in the results, the overall prevalence of a VIP score is similar on both sites at 7% and 9% respectively, with a combined prevalence of 8%. This overall result would suggest that patients are not seeing worse outcomes if PVCs are changed based on clinical indication and not routinely. According to Morrison and Holt (2015), clinically indicated removal does not increase patients' risk of complications when compared with routine replacement, which would confirm that the risk is increased by the overall exposure to the use of PVC. Results from the PRUH site are similar to those from a study by Pasalioglu and Kaya (2014), who found significant difference in PVC phlebitis stage distribution with lowest rates in the group with a dwell time of 97-120 hours, decreased rates in the group with dwell time of 49-96 hours and highest rates in those with a dwell time of 48 hours or less. A global prevalence study of over 40 000 PVCs (Alexandrou et al, 2018) found no association between dwell time and phlebitis rates.
Phlebitis (inflammation of the vein) is generally associated with PVC use, and is caused by factors including catheter size and type of material, site of insertion, stabilisation of the device, concentration of medication and mechanical irritation. Rickard et al (2010) reported that patients most likely to develop phlebitis will do so between 24 and 48 hours because this time is associated with the time taken by the body to mount a biological response after the start of therapy. Therefore, regular monitoring and surveillance using the VIP tool, which has a range of 0-5 (0 indicates no sign/symptoms of phlebitis and 5 advanced stage of thrombophlebitis), helps to ensure timely identification of phlebitis/complications and removal with re-siting if necessary. Of the PVCs audited, 16 (3.2%) had a VIP of 2, indicating the first stage of phlebitis; this is lower than the benchmark of 5% set by the CDC (Gallant and Schultz, 2006). Phlebitis can contribute to failure of PVCs leading to delayed therapy, increased length of hospital stay and cost, yet it is an under-reported complication. However, the VIP tool (when used appropriately) is very effective in the monitoring and observation of PVCs to reduce these complications. All PVCs that were assessed as having a score >1 were removed and re-siting recommended if there were still a clinical need. None of the 500 PVCs observed/assessed had any complications beyond erythema and/or tender on palpation (early stage of phlebitis).
In this audit, the authors found 16% of the PVCs overall did not have a clinical need; this proportion of unused PVC increased the risk of infection and other complications. Of the 36 PVCs in situ for more than 7 days, 19 had a clinical need and 17 were not needed. Based on this almost 50-50 split (53%/47%) in this group, the overall number of ‘idle’ PVCs and the guideline recommendation of 7-10 days, it may be prudent to revise the dwell time down from 10 days (240) to a duration of 7 days (168 hours). However, any decision should take into consideration the total numbers (16) in relation to degree of complication, venous access site and clinical need. It is also worth noting that for 81.8% of the PVCs observed, the dressings were optimal (clean, dry and intact) while 18.2% were suboptimal with one or more deficit—for example, loose, wet, soiled or the insertion site obscured. Dressings should be kept dry and clean and allow visualisation of the insertion site to reduce risk. Optimal dressings were observed in 84% of those PVCs in situ for 0-3 days, 78% of the 4-7 days group and 72% of PVCs in situ for more than 7 days.
Although guidelines recommended clinically indicated removal, implementation was not without resistance, primarily from an infection prevention and control perspective due to the ‘unknown’. It took 3 years from initial introduction of the guideline recommendations to policy change and implementation. Nevertheless, implementing clinically indicated removal has resulted in better patient experience with fewer PVCs for a course of treatment, which has led to better patient safety and satisfaction. Case in point: the patient with the PVC in situ for 22 days was able to complete 3 weeks of IV therapy with a single PVC. The implementation has also resulted in cost avoidance/savings for the Trust with a notable decrease in the number of PVCs used. A total of 67 373 were recorded on the EPR system between January and December 2017 and 49 809 for the same period in 2018. This is a reduction of 17 564 PVCs (26%) with an approximate cost saving of £70 000 based on equipment cost of around £4 per insertion assuming only one attempt at cannulation per patient. PVC insertions are time-consuming procedures that are performed multiple times daily by clinical staff. Studies have found that thousands of hours in staff time could be saved, and cost avoided, by moving to a policy of replacement only when clinically indicated (Rickard et al, 2010; Bolton, 2015; Morrison and Holt, 2015;).
The cost savings noted above only account for the DH site because the transition from paper documentation to EPR at PRUH was not fully implemented until the third quarter of 2018. To provide a comprehensive report on usage and actual/potential cost savings, the authors intend to conduct further data collection and analysis in conjunction with the procurement team.
Conclusion
Although there is a risk of phlebitis with longer PVC dwell times, the degree of complication remains low even when PVCs remain in situ for more than 7 days. However, as almost 50% of PVCs in situ beyond 7 days had no clinical need, the authors recommend considering limiting dwell-time to 7 days with the option to extend based on assessment, clinical need and suitable veins for access. The audit shows that clinically indicated removal promotes the Vessel Health Preservation Framework and helps in avoiding additional pain and discomfort due to unnecessary reinsertions of PVCs, leading to better patient experience, satisfaction and outcome. Clinically indicated removal also helps save staff time that otherwise would be spent on re-siting PVCs. In addition to these benefits, clinically indicated removal can provide significant, and perhaps undervalued, device-related cost savings for organisations. There is currently a host of evidence to support the implementation of clinically indicated removal, ensuring patients receive timely, safe and high-quality care.
Implementing change (whether big or small) is challenging but necessary; maybe more so within the NHS where demands, pressures and need for efficiency are constant. Nevertheless, health professionals must adopt and innovate to meet demands and provide exemplary care for patients. To achieve this, consistent review is needed to ensure improvements are maintained, and to sustain improvements, exemplary leadership, vigilance and support is pivotal.

