The provision of elective surgery has changed in response to increased demand and a reduction in the availability of hospital beds, with patients routinely admitted on the day of surgery (Mayhew et al, 2021). Day-case admission plays a key role in UK health policy and is now the norm for a range of surgical procedures (Bailey et al, 2019). The COVID-19 pandemic severely impacted the delivery of elective procedures and day-case surgery has the potential to help address the resulting backlog (McWhinnie et al, 2021).
However, day-case surgery has resulted in a transfer of the burden of care to patients and their carers (Sokol and Neerukonda, 2013). Individuals admitted for day-case and same-day surgery must ensure they have complied with the required pre-operative instructions and preparations (Gilmartin and Wright, 2008). This includes pre-operative fasting, which is necessary to mitigate the risk of pulmonary aspiration (Rawlinson and Minchom, 2007).
European pre-operative fasting guidelines require adults to abstain from food for 6 hours and clear fluids for 2 hours (Smith et al, 2011; National Institute of Health and Care Excellence (NICE), 2020). Anecdotal evidence and published studies indicate that many patients admitted on the day of surgery have either not fasted for long enough (inadequately) or for longer than necessary (excessively) (Cantellow et al, 2012; Lim et al, 2014; El-Sharkawy et al, 2021). Cancellation of surgery due to inadequate fasting has cost implications for organisations, and social, psychological and emotional costs for patients (Brady et al, 2003; Lim et al, 2014). Excessive fasting occurs more frequently than inadequate fasting and is associated with adverse physiological outcomes, such as dehydration, metabolic stress and insulin resistance, which may all contribute to increased length of hospital stay, morbidity and mortality (El-Sharkawy et al, 2021).
Previous studies demonstrated that patient recall of fasting instructions is poor (Walker et al, 2006; Cantellow et al, 2012). In addition, the lack of understanding of the rationale for fasting has been shown to result in patients underestimating the importance of doing so and, consequently, affected adherence to fasting instructions (Walker et al, 2006; Lim et al, 2014). These studies also found that patients were more likely to be dishonest about their fasting status when they did not know why they were fasting. Other studies have suggested that health professionals think that patients fail to adhere to fasting instructions because they do not understand the reasons for doing so (Baril and Portman, 2007; Cantellow et al, 2012). Guidance, such as that outlined in the Royal College of Anaesthetists (RCoA) (2023) patient information leaflet clearly outlines the rationale for fasting; however, such advice is not always included in information provided to patients.
Pre-operative assessment has developed in line with the move to same-day and day-case admissions (Mayhew et al, 2021). Its purpose is to identify medical, social and psychological issues that may affect patient safety in the peri-operative period, and take steps to address them (Jaensson et al, 2019; Mayhew et al, 2021). According to the NICE (2020) guideline, a key role for staff is to provide information to support patients in planning successfully for their surgery, which includes fasting.
Aims
The aims of this study were to:
Methods
Methodological approach
A qualitative study was conducted using interviews to explore fasting decisions in single day-case unit in a large NHS teaching hospital. A single clinical setting was chosen with the objective of improving pre-operative communication within that unit. Since the aim was to gain insights into patient experiences, qualitative description provided the methodological approach (Neergaard et al, 2009; Willis et al, 2016): this provides a framework to summarise and organise data, using language reflecting that used by participants, without the need for an underlying theoretical framework (Sandelowski, 2010; Willis et al, 2016).
Sample
Participants with experience of making pre-operative fasting decisions were purposively selected using the following inclusion and exclusion criteria (a purposive sample) (Ritchie et al, 2014).
Inclusion criteria:
Eligible patients (n=37) were identified at pre-operative assessment between October 2017 and January 2018 and were sent participant information sheets outlining the study along with their appointment letters. On the day of surgery, patients were approached and written consent was obtained from those interested in participating (n=21).
Data collection and analysis occurred concurrently and, once there was consistency across the data with no new findings, recruitment was discontinued, and no further interviews were conducted.
Data collection
Semi-structured interviews were carried out by telephone at least 1 week post-operatively. An interview guide based on the research aims, clinical experience and the literature provided a framework for interviews. This was to ensure that core concepts could be captured and to allow participants to discuss factors important to them (Patton, 2002; Britten, 2006). The use of the interview guide developed and in later interviews acted as a prompt for further exploration of topics brought up in earlier interviews. For example, participants in earlier interviews discussed the importance of receiving information in different formats, and this was explored in subsequent interviews. During the interview, follow-up questions were used to make sure that the researcher had correctly understood the participants’ meaning and to allow the participant to elaborate on their answers. The interviews were audio recorded.
Data analysis
The interviews were transcribed verbatim and anonymised. Thematic analysis employing the six steps outlined by Braun and Clarke (2006; 2022) was used to analyse the data (Table 1). Themes relating to factors that influenced pre-operative fasting decisions were identified and their relationships analysed. Transcripts and coding were checked by an independent, experienced researcher. The researcher is an integral part of data collection and analysis in qualitative research, so a reflexive journal was kept enabling the researcher to acknowledge the influence of their role on the research process (Ormston et al, 2014).
| Step | Actions | Examples |
|---|---|---|
| 1. Data familiarisation | Transcription | Transcription involved listening to the interview repeatedly. It allowed the data to become familiar and for points of interest to be identified and noted |
| Actively reading transcripts and reflexivity | Active reading considered the data from several points of view. Reflexivity included taking notes immediately after each interview, for example noting my impressions of each participant and their attitudes to preparing for the operation. I also noted my a priori understanding around pre-operative fasting and the importance of explaining the rationale, and how this might influence data collection and analysis | |
| Noting initial ideas and points of interest | Initial ideas: considered patient journey through the process, communication, routine, trust, the participants’ previous experience, the patient role | |
| 2. Generation of initial codes | Inductive codes (data driven) | Inductive codes: wanting/not wanting information; older people more trusting/younger people less trusting of health care; individual approach to planning for the operation (eg whether they changed their usual routine to accommodate fasting) |
| Deductive codes (derived from interview guide and a priori ideas) |
Deductive codes: previous experience of pre-operative fasting; knowing/not knowing the rationale; need to know/do not need to know rationale; information about pre-operative fasting and what to do |
|
| 3. Generation of initial themes | Codes reviewed and collated |
Initial analysis grouped the codes into two overall themes:
|
| 4. Review of themes | Themes reviewed. Do they work in relation to coded data? |
The themes were reviewed in the context of the whole experience/journey taken by the patient from referral through to the operation and recovery. Themes were reorganised to better represent the data |
| 5. Themes defined and named | Themes reviewed and refined |
‘Going in for an anaesthetic is definitely something that’ on your radar’: the operation as a serious event |
| 6. Report preparation | Final analysis, quotes chosen, relation of findings to literature and research question | The process of writing up allows for consideration of the themes within a wider context, such as the existing literature, and the research question |
The table summarises the steps taken as part of thematic analysis, using examples from the study to illustrate how the process was applied in this project. Reflexivity was the process of acknowledging the author's own role in data collection and analysis
Based on Braun and Clarke, 2006; Vaismoradi et al, 2013
Ethical approval
Ethical approval and permissions were granted through the Health Research Authority, NHS Research Ethics Committee, the University of Leeds and the local NHS trust. Audit and research governance were overseen by the University of Leeds and the NHS trust.
Findings
Of the 21 patients initially recruited, 10 agreed to participate and were interviewed. The remaining 11 patients declined to take part for the following reasons:
The final number of patients (n=10) is an appropriate sample size for this type of study (Braun and Clarke, 2006; 2022). Participants were aged between 18 and 55 years: 18–25 years (n=1), 26–35 years (n=7), 36–45 years (n=1), and 46–55 years (n=1). Interviews lasting between 6 and 20 minutes took place a mean of 20 days (10–28 days) postoperatively.
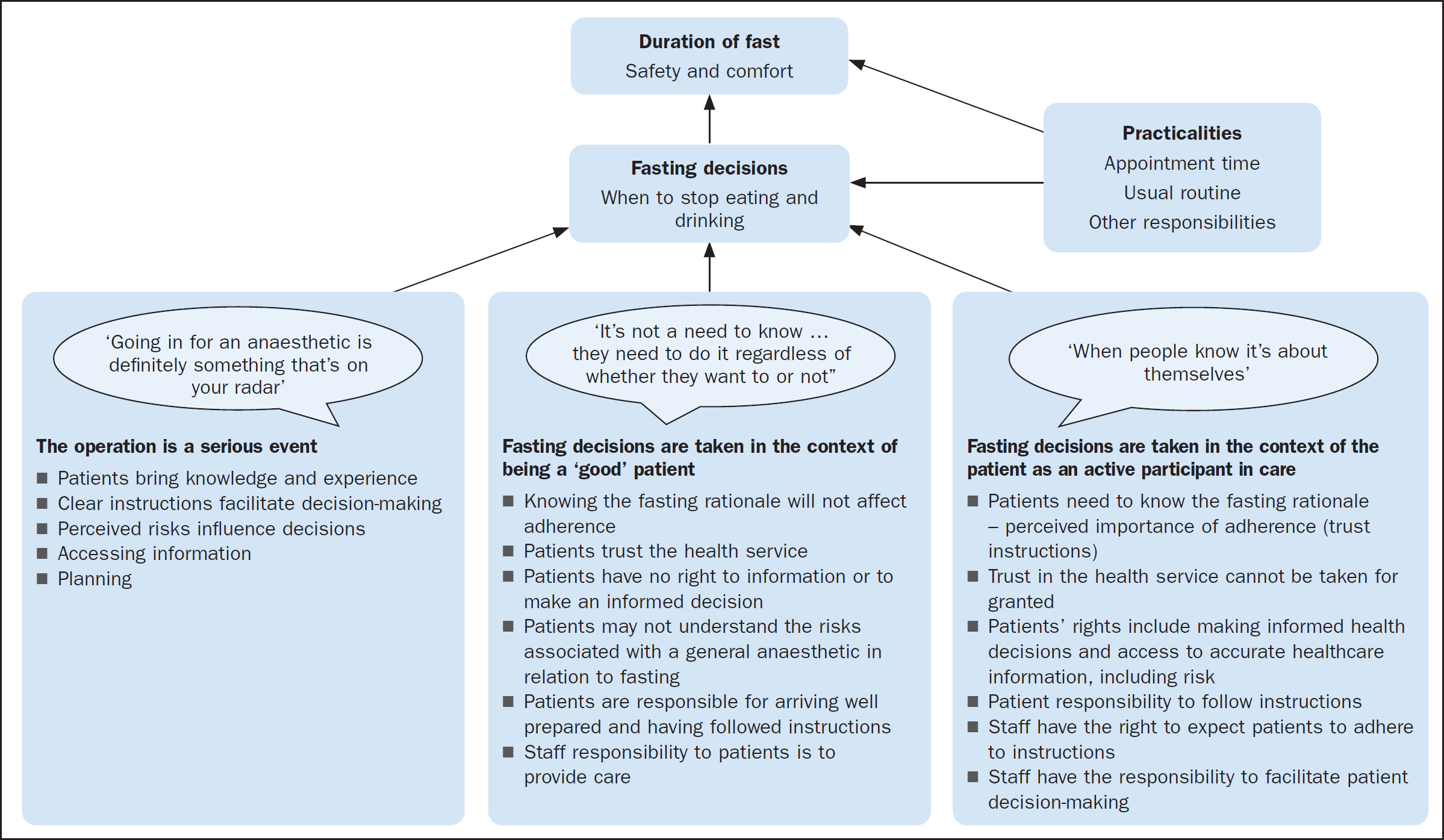
Participants’ understanding of the reason for pre-operative fasting varied (Box 1). Despite this, all had fasted at least adequately (Table 2) and their surgery had gone ahead as planned. Fasting duration depended on fasting decisions (when to stop eating and drinking) and practicalities such as appointment time (Table 2 and Figure 1). The thematic analysis resulted in the generation and naming of three themes (Table 1: step 5) to describe the factors that contributed to fasting decisions:
Participant knowledge of the rationale for fasting
| Explanations for pre-operative fasting given by participants | |
|---|---|
| Rationale known | ‘So it reduces anaesthetic complications… you can get reflux into your lungs … you can get… aspiration pneumonia’ (participant 2) |
| Rationale partially known | ‘I think it's because you could be sick’ (participant 3) |
| Rationale not known | ‘I don't actually know the reason why, no’ (participant 9) |
| Appointment time | Last food (time) | Last drink (time) | Solid fast (hours) | Fluid fast (hours) | Comments |
|---|---|---|---|---|---|
| Morning appointments | |||||
| 08:00 | 18:00 | 18:00 | 14 | 14 | Woke too late for a drink |
| 21:00 | 06:00 | 11 | 2 | Ate late supper to reduce solid fast time | |
| 21:00 | 03:00 | 11 | 5 | Woke during the night and had a drink | |
| 10:00 | 21:00 | 21:00 | 13 | 13 | Decided not to eat or drink anything in the morning |
| 21:00 | 08:00 | 13 | 2 | Ate a late supper to reduce solid fast time | |
| 18:00 | 23:30 | 16 | 10.5 | Given incorrect fasting instructions | |
| 19:00 | 05:30 | 15 | 4.5 | Deliberately woke early to drink water | |
| 20:30 | 06:15 | 13.5 | 3.75 | Deliberately woke early to drink water | |
| Afternoon appointments | |||||
| 12:30 | 06:30 | 06:30 | 6 | 6 | Given a drink in unit (so fluid fast reduced from this figure) |
| 07:30 | 10:30 | 5.5 | 2 | Solid fast exceeded 6 hours at time of anaesthetic induction | |
The first theme describes the seriousness of having surgery. The second and third relate to the extent to which participants discussed being actively involved in their care.
Theme 1. ‘Going in for an anaesthetic is definitely something that's on your radar’
Patients described having surgery as being serious event.
‘… going in for an anaesthetic is definitely something that's on your radar… “OK this is a big thing that I need to remember to do’’.’
It was also clear that previous knowledge and experience played an important role in decision-making for some participants. For example, two had worked professionally in health-related settings and commented:
‘We did… some harm reduction advice… about eating or not eating and when to stop eating… in case they [the patient] did go unconscious and… were sick… there's a lot of harm reduction around actually not eating.’
‘It [having an empty stomach] reduces anaesthetic complications… you can get reflux into your lungs and… aspiration pneumonia…’
For some patients, previous experience of having had surgery or that of family members influenced their decision to fast:
‘Twelve o'clock the night before I had to not eat from… I know you're allowed a sip of water…’
‘I've always just known you have to [fast]… I've never had a general anaesthetic before, but my [relative] has and I just knew that [they] always had to stop eating and drinking before.’
Clear instructions were a prerequisite for fasting decisions. Participants commented positively on the role of pre-operative assessment and the nurse's role in providing information.
‘The pre-assessment [nurse] was really good, she explained everything really well… ’
‘She told me exactly what I needed to do… ’
Patients also appreciated the opportunity to ask questions and clarify instructions during the pre-operative assessment and in conversations pre-operatively with the nurse:
‘… and I could ask my questions when I spoke to her on the phone as well… how I go about taking medication in the morning if need be …’
Participants described being provided with confirmation in writing of information given verbally and perceived this as being beneficial.
‘It was good to have that reiterated in the letter and with the leaflet… so I felt very prepared going into it which was good… I did feel, like, I could be quite organised because the timings were very specific and they were given to me way in advance…’
Individuals expressed a distinction between needing and wanting to know information:
‘More information is always welcome… I mean for me, personally, knowing what's going to happen would be good…’
However, some participants mentioned that the right to decline information was also important:
‘I didn't know what to expect and, also, I'd rather not know what I was expecting [laughs]… so when the nurse called me beforehand and asked if I wanted her to go through the procedure, I actually asked not to be… the information was offered to me, but I declined it.’
Risk perception also influenced decision-making, with risk of cancellation being a concern for some patients.
‘Well, surgery doesn't normally go ahead if you've eaten… I could have had more [to drink in the morning] but I just didn't want to… I knew there was the operation, so I kind of just wanted to quench my thirst, I didn't want to have loads, just in case.’
Risk of dehydration was mentioned by two patients. They had made deliberate decisions about the fluid fast to mitigate the risk of dehydration, while meeting the requirement for a minimum 2-hour fluid fast:
‘I do drink quite a lot of water, so I was worried about being… dehydrated. I can get quite… headachy. So, I was thinking “I'll just do it” [have a drink] right before I'm not allowed any more and then it should… see me through.’
‘I did get up… earlier in the morning so I could have a drink… I think when you need a drink [and you don't drink] that does make you get… a headache and makes you feel tired…’
The final themes were developed by considering codes – risk, responsibility, rights, and trust – in relation to the importance of patients knowing the rationale for pre-operative fasting (Table 1: step 5). They describe two opposing approaches to the patient role and the relationship between patients and staff.
Theme 2. ‘When people know it's about themselves’
This theme is derived from the notion that patients are more likely to adhere to fasting instructions when they realise that it is related to their own safety and comfort:
‘When they know it's about themselves.’
This theme reflects the situation when it is important for patients to be told the rationale for pre-operative fasting and identifies the underlying assumptions in relation to trust, responsibilities and rights.
A fundamental assumption is that trust in the health service cannot be taken for granted. One patient stated:
‘… and I think that [that] day and age has gone in a sense… people want to know why they want to do things… I don't think they [younger people] are as trusting. I don't know whether older people just do whatever they're told… because they trust more in the health system.’
Furthermore, it was clear from the responses that participants thought that trust needs to be earned. Some expressed the view that the pre-operative assessment may provide an opportunity for trust to begin to develop:
‘[During the pre-assessment] he explained everything really well… I do get quite anxious and I think if it had been… wishy-washy it would have just added to the stress.’
Providing a reason to fast assumes the right of patients to make informed health decisions and the responsibility of staff to provide accurate information. This includes information to enable patients to make a judgement about healthcare-associated risks. For example:
‘Some people don't understand and they're, like, “well, I'm hungry so I'm gonna eat”, and then obviously bad things can happen… it would be beneficial [with] someone… explaining… why you can't eat.’
Patients also have a responsibility to staff to follow instructions, which was acknowledged by some participants:
‘Obviously, the surgery is for my own benefit, so if I wasn't to follow the rules that's putting myself at risk… that would be a silly thing to do when you've been given the advice not to do it. If you went ahead… it's your own health you're putting in danger, and that's not fair on the medical staff who are only there to help.’
This theme illustrated a patient-staff relationship, which showed that patients acknowledged mutual rights and responsibilities.
Theme 3. ‘It's not a need to know… they need to do it regardless of whether they want to or not’
By contrast, this theme is derived from the notion that patients should follow instructions without necessarily knowing why.
‘It's not a need to know… they need to do it regardless of whether they want to or not, or the information you provide to them, as [to] WHY… it needs to happen… ’
Under this theme, the participants’ responses illustrated an assumed trust in the healthcare system:
‘I've never even thought about it [the rationale] actually. I just do as I'm told, basically. I presume [that] if somebody in the medical profession's advised you not to, then, you know, it's for a good reason.’
Under this theme, patients have the responsibility to follow instructions, but not necessarily the right to exercise judgement. Participants described ‘blindly’ following the rules:
‘I just always follow rules, and that's it.’
‘I think, if they tell you not to eat, I just didn't eat.’
A consequence of not needing to know is an assumption that there is no patient right to information or understanding of the risks. This abdicates staff of the responsibility to provide information to facilitate patient choices. Information is described as ‘interesting’ and in the second quote is dissociated from adherence to fasting instructions:
‘It needs to happen, regardless… but I do think it's interesting and I do think if the information is available people would be interested to read it.’
‘I would probably have been interested to know why, but I don't think it would have… made me stick to it more.’
This seems in keeping with the idea that patients do not need to exercise judgement in this respect. This was surprising, but was expressed by participants across the spectrum in terms of surgical experience, gender and age. However, these comments came from patients who did not know the rationale behind the need to fast pre-operatively.
Practicalities
Ultimately, fasting decisions were taken in relation to practical issues. The themes outlined contributed to the decision-making process, but the duration of the fast was determined by the patient's surgery appointment time and factors such as family life and routine. Fasting times were longer for morning appointments due to overnight fasting (see Table 2):
‘I would usually have had a bit of water, but I woke up too late to have some.’
The relative importance of the factors that influenced fasting decisions depended on the individuals involved.
Discussion
Health care is delivered within social interactions in which patients and health professionals each assume roles and responsibilities (Kelley, 2005). The move to patient-centred care relies on patients taking a more active role. This is emphasised in a day-case setting, with patients and carers assuming responsibility for the pre-operative and recovery periods (Sokol and Neerukondo, 2013). However, the findings of this study suggest that there is variation in the extent to which patients wish to take an active role. This is in keeping with research into the impact of day-case surgery which found that some patients adopted a passive role in relation to self-care, preferring to rely on healthcare staff (Mottram, 2011). Patients are more likely to take an active role when they perceive themselves to be at risk and think they can take action to moderate that risk (self-efficacy), as well as to influence events (internal locus of control) (Hayden, 2014).
There are implications for staff in meeting the differing information needs of patients. Previous studies have advocated explaining the rationale to improve adherence to fasting instructions (Walker et al, 2006; Baril and Portman 2007; Lim et al, 2014). The notion that there is a link between knowing the rationale, appreciating the importance of fasting and adherence to instructions (Lim et al, 2014) did not seem to apply to all participants in this study. All had complied with the minimum fasting times (Table 2), regardless of their understanding of the rationale. Furthermore, they made the distinction between wanting and needing information.
Healthcare staff have a duty of care to warn patients of the material risks associated with care (Chan et al, 2017), which includes the consequences of inadequate and excessive fasting (Baril and Portman, 2007). This leads to a tension between the need to respect patient preferences, while meeting obligations to provide information necessary for maintaining safety. The incorporation of RCoA (2023) patient information advice in all pre-operative literature would assist in meeting these obligations, and this should be reiterated verbally. Patient preferences can then be addressed within pre-operative discussions, allowing information to be tailored to an individual patient (Chan et al, 2017). For example, two participants who expressed a preference for minimal information both wanted clear instructions to enable them to make deliberate fasting decisions that suited them. These participants both had solid fasts in excess of 13 hours. One had a fluid fast of 13 hours and the other 3.75 hours (Table 2).
Staff therefore have a supporting role by providing the relevant information and enabling patients to make decisions based on their own values and preferences (Gauthier,2005). The Code (Nursing and Midwifery Council, 2015:7) states that nurses should ‘encourage and empower people to share decisions’ and ‘respect the level to which people… want to be involved in decisions’. Nurses are well placed to ensure that patients have the information they need within the limits of the information they want. Nurses play an important role in supporting patients to prepare for surgery.
Strengths and limitations
The main strength of the study was the use of interviews to explore fasting decisions. This enabled patients to discuss the issues relevant to them. There were several limitations. Non-English speakers are disadvantaged when accessing pre-operative information and excluding them prevented exploration of the experiences and needs of this under-represented population. Similarly, inclusion of those who might fast inadequately pre-operatively would strengthen the study by investigating the specific needs of these patients.
The relative brevity of the interviews may suggest lack of depth in the data. It was anticipated that the interviews would last between 15 and 30 minutes, with most falling within this time frame. One interview took just 6 minutes and was included in the data analysis because the participant provided important insights to their decision-making, understanding of the rationale and how practicalities contributed to length of fast. It was important to include in the data analysis because these insights contributed to the overall data and the way that subsequent interviews were conducted. Interviews in a similar US study took around 15 minutes (Crenshaw and Winslow, 2002). The focus on fasting decisions is narrow and does not lend itself to extremely long interviews.
The use of the telephone to undertake qualitative interviews could potentially negatively impact data quality due to the loss of visual and non-verbal cues. However, telephone interviews can be used successfully to obtain good quality data (Trier-Bieniek, 2012). The clinical setting in which the study took place has routinely carried out pre-operative assessments by telephone for many years (predating COVID-19). The author therefore had experience with clinical interviews by telephone, and was used to listening for non-verbal and other cues. The study participants all had pre-operative assessment by phone before attending the department in person, therefore, some of the potential difficulties of telephone interviewing were mitigated as the process was familiar to both parties.
Further research
The findings of studies exploring the fasting decisions and information needs of non-English speakers, and of patients who have not fasted adequately, could lead to improvements in pre-operative communication with these patients.
Another recommended area for research is to investigate the role of digital media in meeting patients’ pre-operative information needs. This could include the use of mixed media.
Conclusions
Patients in this study approached admission for a general anaesthetic as a serious event that required a degree of planning. Fasting decisions were made within the context of knowledge and experience, and were made easier by the provision of clear information. This enabled individuals to adjust their fluid and food intake to meet the fasting requirements. Patients had differing information needs. Fasting duration was the outcome of fasting decisions and practicalities.
Recommendations for practice
Pre-operative assessment should include a question about admission-specific concerns. This would enable staff to assess specific information needs in addition to the minimum advice required, and to tailor information to each individual. For example, one participant wanted clear instructions about safely taking medication on the morning of surgery. Discussions should be clearly documented: this should include recording risks and alternatives, patient understanding and information preferences, as well as noting cases when information is declined.
The rationale for pre-operative fasting should be explained to all patients, both verbally and in writing (Box 2). This should include the relationship between how long fasting is required and the times patients are asked to stop eating and drinking. Fluid intake should be actively encouraged until the stated time to stop.


