Within the Therapeutic Apheresis Services (TAS) of NHS Blood and Transplant (NHSBT), specialist nurses are required to complete on-call work in addition to their weekly working week of 37.5 hours. The on-call nurses respond to medical emergencies that occur overnight and at weekends within their region. This requires completing lifesaving apheresis interventions for paediatric and adult patients.
On-call working exposes nurses to being at risk of working up to 24 hours in one set period, which in turn increases their likelihood of experiencing fatigue (Domen et al, 2015). The British Medical Association (BMA) (2018) has stated that fatigue associated with long working hours, particularly that which interferes with natural circadian rhythms, has negative implications both professionally and personally for the health professional, and, importantly, also for patient safety. Further to this, fatigue has been closely linked to increased risk of burnout, cardiovascular disease, dementia and certain cancers such a breast and prostate cancers (Wong et al, 2019).
Due to historically low retention rates within the TAS specialist nursing workforce, and anecdotally reported low morale around the topic of on-call working, it is important that measures are taken to improve such a significant and vital area of TAS. Through the implementation of a fatigue-identification tool for nurses who are on call, NHSBT can work towards a culture that retains a happy and healthy workforce despite the unique nature of the TAS specialist nurse role. NHSBT can then work with its workforce to enhance safety practices while protecting the nurses from the risk of fatigue and its negative implications for their health and wellbeing (Ramdan, 2019).
Methods
In order to complete a thorough evaluation of the service, both a literature search and a range of data collection methods were used.
Literature search
A literature search was completed specifically around the topics of fatigue and on-call working within nursing, using the medical databases CINAHL, Embase, Medline and Cochrane. Results were limited to the past 10 years to ensure up-to-date and relevant information. Full-text, peer-reviewed and English-language literature was searched; time constraints would not have allowed for translation services.
Further techniques such as proximity searching were used to narrow down the search. Proximity searching gave results that had the terms ‘on-call’ and ‘fatigue’ next to, near or within the same sentence. The use of both the AND and OR Boolean operators were used for both comprehensive and specific search results (Polit and Beck, 2010). The key words used were ‘on-call’ AND ‘nursing’ as well as ‘on-call’ AND ‘fatigue’, giving results that had all the key words used, even if they were not next to each other or in the same sentence. It was also beneficial to search the key words ‘nursing’ OR ‘doctors’ to help generate relatable results from other health professionals who are likely to also complete on-call work. The decision to include global results enabled comparative literature to be reviewed with the possibility of new perspectives to be identified. Alongside this, searches outside these databases were also completed, looking at a variety of non-medical industries whose staff also complete on-call work and how they manage/prevent the effects of fatigue related to working on call.
Data collection
Following the completion of the literature search, a variety of data were collected to gain an understanding of the current landscape in TAS with reference to fatigue and on-call working.
The first stage of data collection involved reviewing existing data available from TAS nurse exit interviews. When reviewing these it was identified that all respondents had highlighted ‘support when on call’ as a contributing factor to leaving. Furthermore, when collating the national TAS specialist nurse sickness records for the preceding 12 months, it was found that there were 25 individual incidences of absence that were related to ‘anxiety/stress/depression/other psychiatric illnesses’. Although these findings cannot be attributed directly to fatigue, it is a potential contributing factor. In addition, on-call data were collected to ascertain how many on-call hours the nurses had completed in addition to their contracted hours.
Identification tool creation
In order to inform the creation of a fatigue-identification tool, a survey was designed to gather a baseline of health and wellbeing information on the four North unit teams in England. Piloting a survey in a small sample of intended respondents can be a useful way to identify any formatting or content issues before its dissemination to a wider group (O'Connor, 2022). Following this pilot, no changes were made to the survey. The survey consisted primarily of closed questions. Although using closed questions allows for a timelier analysis of the data and ensures that participants have the same frame of reference when choosing their answers (Colosi, 2006), there would be no capacity for respondents to describe their own experiences or include additional information. Therefore, three open questions were added to the survey to allow the nurses to provide their insights on the topic in question.
As a result of the data collected, an evidence-based fatigue-identification tool was created in Microsoft Forms. The draft tool was then introduced to a focus group that had been further reduced to two North unit teams. This decision was made to ensure there was the opportunity to engage fully with the teams and build a reciprocal relationship, encouraging full participation and a greater understanding of the topic. This enabled the collection and analysis of data in accordance with the time frame of the project. After introducing and explaining the draft tool to the teams, it was then implemented over 31 days, requiring participants to complete it at the end of every working shift and at the start of every on-call shift. This resulted in 36 respondents taking part.
Results
For each of the four units considered, the total number of on-call hours worked in addition to contractual working hours was collated for 6 months. The data are displayed in Table 1, which shows the number of staff per unit, per month.
| Date | North unit 1 | North unit 2 | North unit 3 | North unit 4 | ||||
|---|---|---|---|---|---|---|---|---|
| Hours | Number of nurses | Hours | Number of nurses | Hours | Number of nurses | Hours | Number of nurses | |
| February 2023 | 69.50 | 8 | 20.50 | 5 | 50.50 | 7 | 90.50 | 8 |
| March 2023 | 61.75 | 8 | 58.75 | 5 | 78.50 | 7 | 23.50 | 8 |
| April 2023 | 70.25 | 8 | 27.25 | 5 | 90.00 | 7 | 86.00 | 8 |
| May 2023 | 78.75 | 8 | 52.75 | 5 | 47.50 | 7 | 42.50 | 8 |
| June 2023 | 50.50 | 8 | 58.50 | 5 | 85.00 | 7 | 25.00 | 8 |
| July 2023 | 94.50 | 8 | 53.25 | 5 | 105.75 | 7 | 48.00 | 8 |
Note: on-call hours are in addition to the contracted 37.5 per nurse
A health and wellbeing baseline questionnaire was then sent out to all the units; 19 staff members out of a total of 31 responded, giving a 61% response rate. The baseline questionnaire identified key findings within the teams and highlighted that 68% of respondents lose concentration when at work due to being on call. Reasons for this included working hours that extend into the night, a lack of opportunity to take sufficient breaks and being overstimulated from nursing patients with complex conditions. No respondents selected that they ‘always’ get their specified rest break, with 17 respondents stating that they either ‘always, often, or sometimes’ have experienced a colleague showing signs of tiredness during their shift.
Furthermore, 47% of respondents identified that personal circumstances, including health conditions and child care, prevent them from getting adequate rest when off work. To help reduce fatigue within the workplace, respondents recommended reviewing the on-call patterns, travelling times, staff retention and workloads to ensure adequate rest periods.
The fatigue-identification questionnaire was then piloted in two of the above units. It required completion at the end of every contractual shift and at the start of each on call mobilisation (that is providing care rather than being on call at home) over a 1-month period. In total, 36 responses were received, with 90% of them being completed at the end of a shift and 10% being completed at the start of an on-call mobilisation. The results are shown in Figures 1 to 4.
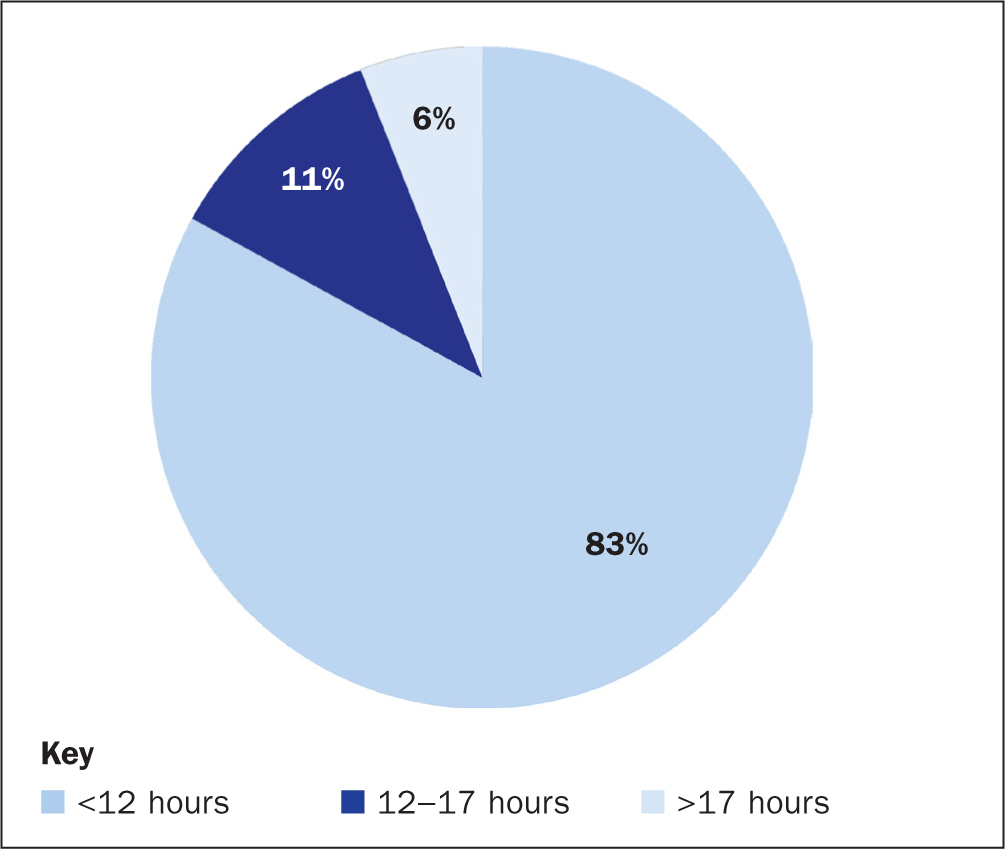
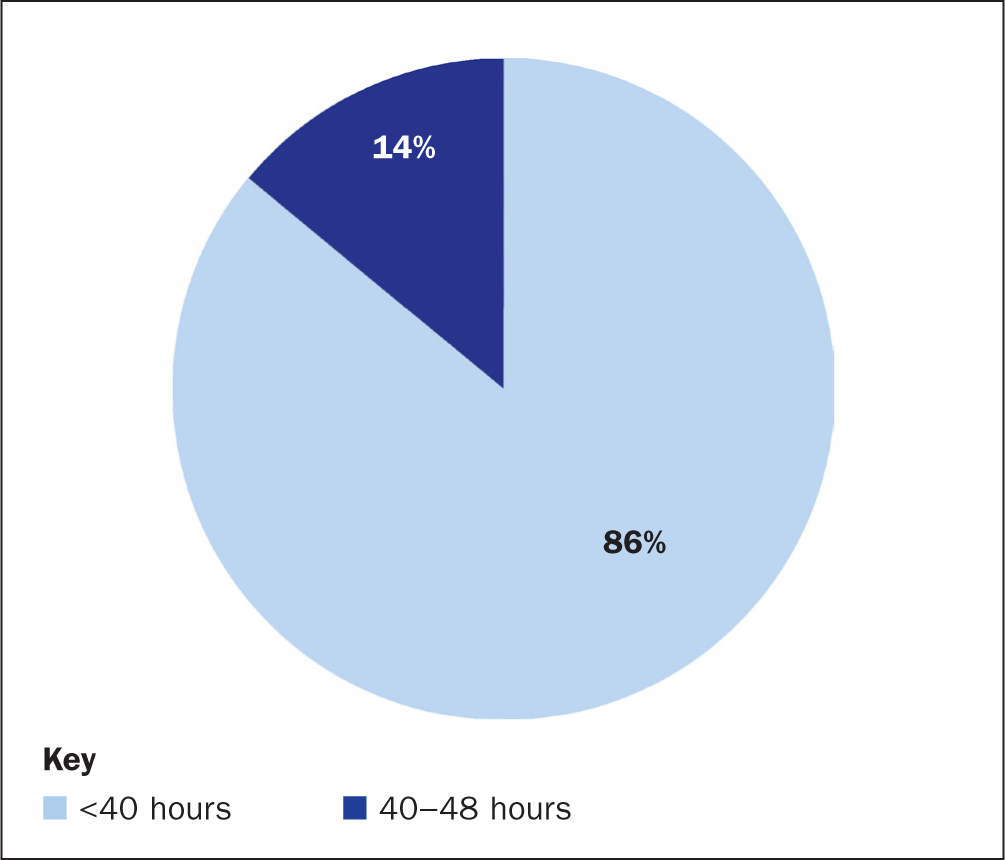
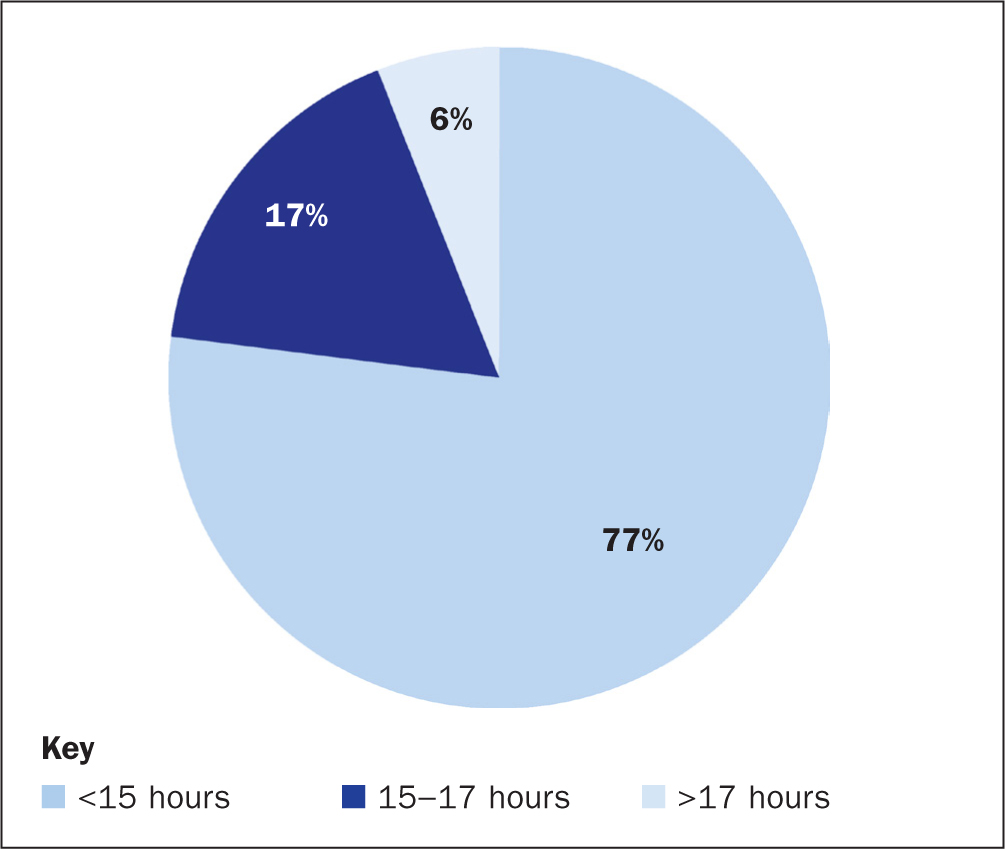

Figure 1 highlights that, whereas most respondents worked less than 12 hours, 11% worked between 12 and 17 hours and 6% worked more than 17 hours. Figure 2 demonstrates that 86% of the respondents worked under 40 hours within 7 consecutive days and 14% worked 40 to 48 hours. In addition, 40% of respondents stated that they had had less than their ideal amount of sleep in the preceding 24 hours. Furthermore, Figure 3 shows that 77% of respondents had an ‘awake window’ of less than 15 hours, whereas 17% had an awake window of between 15 and 17 hours and 6% of more than 17 hours. It is interesting that 14% of the respondents claimed to not have had a break, leading to 34% having inadequate food and hydration during their shift.
Figure 4 captures 40% of respondents stating they feel alert, whereas another 40% felt effort was required to stay alert, and 20% had difficulty staying alert. Respondents also reported being ‘very tired mentally and physically’ and being ‘emotionally exhausted’.
Discussion
The fatigue-identification questionnaire aimed to explore whether the use of an early warning tool would help identify risk factors that contribute to staff experiencing fatigue when on call. The data captured highlighted that 17% of staff had worked more than 12 hours. According to Querstret et al (2020), they were at an increased risk of experiencing fatigue due to the length of their shifts. They were also at a 27% increased risk of an injury or accident compared to those who work 8-hour shifts (Pickup, 2023). Domen et al (2015) stated that this extended shift length is associated with poor performance, reduced reaction time and decreased vigilance. Similarly, it has been reported that clinicians who work longer than 13-hour shifts have more instances of patients experiencing dissatisfaction with their care (Stimpfel et al, 2013).
It was also found that 17% of respondents had been awake for 15-17 hours, which has been associated with significant reduction in the quality of performance, including memory and decision-making (Caldwell et al, 2019). A further 6% of respondents reported being awake for more than 17 hours. It has been found that such workers have a similar performance level to those who have 0.05% alcohol in their blood. This rises to 0.10% for those who have been awake for 24 hours or more (Williamson and Feyer, 2000). To put this into context, in England, Wales and Northern Ireland, the maximum drink driving limit is 0.8% and 0.5% in Scotland, compared with 0.5% in most of Europe and 0.2% in Norway, Sweden and Poland (European Transport Safety Council, 2021).
It is therefore crucial to understand that some nurses completing the questionnaire at the start of their on-call mobilisation were going to exceed an awake window of 24 hours, with the expectation that they would be providing life-saving treatment. An example of this can be seen from a respondent who stated they were still not home at 06:00 the following morning after their usual working shift of 08:00 to 18:00. It is therefore unavoidable that acute fatigue will be experienced due to disturbance of their natural circadian rhythms (Sprajcer et al, 2022).
Looking at a 7 consecutive day period, it was found that 14% of respondents had worked between 40 and 48 hours. This has been reported to increase the health and safety risks associated with workers and a higher prevalence of fatigue, job stress and depression (Caruso et al, 2022). Similarly, Hoedl et al (2021) reported that 15% of nurses who work more than 40 hours in 1 week experience high levels of stress. Stress has been found to be consistently associated with fatigue (Kop and Kupper, 2016). As an attempt to countermeasure this, workers are more likely to have poor health behaviours that include smoking, increased alcohol and/or food intake, short sleep durations and low physical activity (Caruso, 2014).
Those who are on call but not yet mobilised are restricted in their location and activities, which may interfere with their work-life balance. This has been found to impact their ability to psychologically detach from work and makes it difficult to optimally direct their attention to either work-related or home-related tasks (Ziebertz et al, 2015). This can contribute to impaired recovery from fatigue but also generate further fatigue due to the lack of opportunity to completely detach from work. One respondent stated that they have had multiple work-related telephone calls during their on-call shift, which disturbed their sleep and left them feeling ‘anxious’, ‘drained’ and ‘exhausted’ in case a decision was made to be mobilised. Such sleep disturbance has been found to be a major causal factor for developing depression, emotional distress and mood disorders (Medic et al, 2017).
Although individual sleep needs vary in relation to duration, quality and timing, it has been reported that not achieving adequate sleep will contribute to experiencing fatigue (Pastier et al, 2022). From the data collected, 40% of respondents stated that they had received less than their ideal amount of sleep at the time of completing the questionnaire. It could therefore be argued that those respondents are at an increased risk of experiencing fatigue.
Furthermore, 14% of respondents identified that they had not received a break, which can be an effective strategy in lowering fatigue and aiding in acute fatigue recovery (Sagherian et al, 2021). Therefore, if staff are not provided with the opportunity of a break, this could be a contributing factor to their heightened risk of fatigue. It was also highlighted that 34% of respondents felt they had not received adequate hydration or food during their shift. Inadequate nutrition is claimed to invoke mechanisms of fatigue and lower alertness. However, sufficient water consumption helps improve cognitive performance and mood, as well decrease the risk of fatigue (Liska et al, 2019). It is not clear whether staff are aware of the importance of adequate hydration in relation to fatigue management.
Taking into consideration the risk factors associated with fatigue, it is reasonable to consider that these have contributed towards 40% of respondents selecting, ‘effort required to stay alert’ and 20% selecting ‘difficulty staying alert’ (Figure 4). It is therefore questionable whether staff have an awareness of strategies to promote alertness and countermeasures to improve performance (Gupta et al, 2022). This has also highlighted that appropriate escalation of this subject is needed to ensure the safety of staff and patients.
Limitations
Owing to the subjective nature of fatigue, challenges around interpretation and differentiation arise that may limit successful data analysis. However, to reduce the effects of this, objective methods of data collection were also used. Due to the time constraints surrounding the project, only two TAS units were sampled, which could hinder obtaining a representative sample of TAS nurses. Future iterations of this project could be conducted if necessary to rectify this.
Recommendations
From the findings, it is recommended that an NHSBT fatigue-management policy would be beneficial for all staff throughout the organisation. This would identify what fatigue is and raise awareness of the need to prevent and manage instances of fatigue. Leading on from this, the introduction of the fatigue-identification tool for those who complete on-call work would enable direct management, monitoring and escalation for those at risk of experiencing fatigue and decrease the risks of patient safety incidents. As a result of this, a more open and honest culture around fatigue is likely to be encouraged and championed throughout TAS. Similarly, it is recommended that ‘human factors’ training is promoted and prioritised as an attempt to increase awareness and knowledge around different factors that can affect human performance. This should also be shared with other areas of NHSBT who participate in on-call work.
Conclusion
The data collected highlights the crucial relationship between working on-call hours and the increased risk of experiencing fatigue. Similarly, the literature reviewed demonstrates the significant negative implications that fatigue has on staff wellbeing, which in turn jeopardises patient safety. Recognising fatigue as a health-and-safety hazard and implementing measures to reduce its incidence will in turn generate a healthier workforce who provide safer patient care.


