Many terms are used to define the extent to which individuals take their medication as prescribed (Cramer et al, 2008). The most common of them are ‘adherence’ and ‘compliance’ (Osterberg and Blaschke, 2005; Aronson, 2007). Although the appropriate term has not been agreed, there is much research interest on the level of adherence to medication regimens, especially among patients with chronic diseases such as hypertension. The study of adherence is important since low levels of adherence are associated with high risks of mortality, deterioration in quality of life and increases in costs of health care (Cutler et al, 2018; Burns et al, 2019).
However, there are many tools for assessing the level of medication adherence and researchers must consider the validity and reliability of each scale to determine which is the most appropriate to be used in each study. In addition, researchers need to decide whether they want to use disease-specific or generic scales. For example, the Hill-Bone scale is a specific tool assessing adherence in treatment for hypertension (Kim et al, 2000), whereas the Morisky and A-14 scales are generic tools (Morisky et al, 1986; Jank et al, 2009). The choice of scale is further complicated by different tools using the same or similar questions.
Aims
The purpose of the present study was to translate and validate the Hill-Bone and A-14 scales. In addition, the researchers' aim was to compare the mean scores of the Morisky Medication Adherence Scale (MMAS), Hill-Bone and A-14 scale between two groups. Finally, to compare the mean scores of items with similar meanings. The above tools were chosen because they are the scales most often used for assessing adherence levels.
Methods
Participants
This methodological study was conducted at a general hospital in Athens, Greece. The evaluation of the scales was based on data collected from hypertensive and non-hypertensive patients. Researchers recruited 34 hypertensive participants by random sampling from those who visited the clinical hypertension unit between 10 February 2016 and 20 March 2016 and met the following inclusion criteria: they were at least 18 years of age, of Greek nationality, with knowledge of the Greek language, were able to communicate verbally, and had used antihypertensive medication for at least 1 year.
The non-hypertensive participants (n=34) were selected from those who visited the hospital for routine or disease-specific blood tests and met the following inclusion criteria: they were at least 18 years of age, of Greek nationality, with knowledge of the Greek language, were able to communicate verbally, and had not used antihypertensive medication. Both groups were standardised for sex, age and educational level.
Ethical considerations
Permission to use the Hill-Bone scale and A-14 scale was obtained from the developers before the start of the study, while permission to use an existing Greek translation of the eight-item MMAS was provided by Elpen Pharmaceutical Company (3 March 2015). The study was approved by the hospital Ethics committee (17929/19-7-13). A written consent form was received from all participants.
Data collection
Demographic and socioeconomic data were collected using a questionnaire. There were eight questions that asked about age, gender, education level, employment status, current marital status, inheritance of hypertension and lifestyle (sedentary or active).
Hill-Bone scale
The Hill-Bone scale consists of 14 items asking about dietary intake of salty foods (three items), appointment keeping for doctor visits and prescription refill (three items), and medication taking (eight items). For evaluation, each item used a Likert scale with answers ranging from ‘all the time’ (4) to ‘never’ (1). The maximum score was 56 and the minimum was 14 (Kim et al, 2000). A lower score indicated a higher level of adherence. The scale is characterised by a significant Cronbach's alpha value of 0.84 (Kim et al, 2000).
Morisky scale
The MMAS consists of eight items (Morisky et al, 2008). The first seven items require a ‘yes’ or ‘no’ response, whereas the final item is answered using a five-point Likert scale (‘never’ to ‘all the time’). Each ‘no’ and ‘never’ answer is encoded with 0 points, whereas all other answers are encoded with 1 point. The highest score is 8 and the lowest is 0. A lower score indicates a higher level of adherence to the medication regimen.
A-14 scale
The A-14 scale consists of 14 items with responses given using a five-point Likert scale from ‘never’ (0) to ‘very often’ (4) (Jank et al, 2009). The total score ranges from 0 to 56. Patients with a score between 50 and 56 are characterised as being 90% adherent, while those with a lower score are characterised as being non-adherent. The items explore five different domains of adherence: patients' ability to remember to take their medicines (question 13); patients' adaptations to medication for reasons of safety and efficacy (questions 1–4, 6 and 7); patients' lifestyle including economic burden and duration of treatment (questions 5, 8–10 and 14); and patients' attitudes to their medication (questions 11 and 12).
It is important to mention the similarity between questions across the tools. The question ‘Do you forget to take your medicines?’ is the first question in all questionnaires. In addition, the question ‘Do you miss taking your pills when you feel better?’ is found as Q11 in Hill-Bone, Q6 in MMAS and Q7 in A-14. Q4 in MMAS and Q5 in A-14 scale ask ‘Do you forget to take your medicines when you travel or leave home?’ and Q9 in Hill-Bone and Q10 in A-14 ask ‘Do you run out of antihypertension medications?’.
The Hill-Bone and A-14 instruments were translated from English to Greek according to international guidelines as follows (Wild et al, 2005): first, the scales were translated from English to Greek by two qualified independent translators, both of whom were native speakers of English and Greek. Each translator produced a translation independently. Second, reverse translation from Greek to English was carried out by another translator. After the acceptance of the English version by the scales’ developers, the Greek version of the questionnaires was distributed to 10 Greek patients who answered and commented on it. These people were excluded from the study. The researchers discussed the comments of these patients. Then, the final version of the Greek questionnaire was available for distribution. Participants needed 5–6 minutes to answer all tools during face-to-face interview.
Data analysis
Descriptive statistics were used to describe the demographic and disease characteristics of patients. Percentages and frequencies were used for categorical variables, while means and standard deviations were calculated for continuous variables. Internal consistency was assessed using Cronbach's alpha. A Cronbach's alpha value of >0.50 and <0.95 was considered acceptable (Cam et al, 2010). The criterion for accepting Cronbach's alpha is a score above 0.5 (Wild et al, 2005). The mean scores were compared by t tests. The significance level was set at P<0.05. All analyses were performed using SPSS v20.0 (SPSS, Armonk, NY).
Findings
Sample
The demographic characteristics of each of the validation samples are shown in Table 1.
| Hypertensive group | Non-hypertensive group | |
|---|---|---|
| Age (mean ±SD) | 65.44 ±12.52 | 65.47 ±12.57 |
| Sex (%) | ||
| Men | 56 | 56 |
| Women | 44 | 44 |
| Education level (%) | ||
| Compulsory | 26 | 35 |
| Intermediate | 65 | 56 |
| High | 9 | 9 |
| Occupation (%) | ||
| Housewife | 18 | 8 |
| Manual work | 15 | 15 |
| White collar officer | 15 | 9 |
| Retired | 53 | 68 |
| Marital status (%) | ||
| Married | 88 | 88 |
| Divorced | 3 | 3 |
| Widowed | 9 | 9 |
| Living status (%) | ||
| With family | 91 | 94 |
| Alone | 9 | 6 |
| Inherited high blood pressure (%) | ||
| Yes | 41 | – |
| No | 59 | 100 |
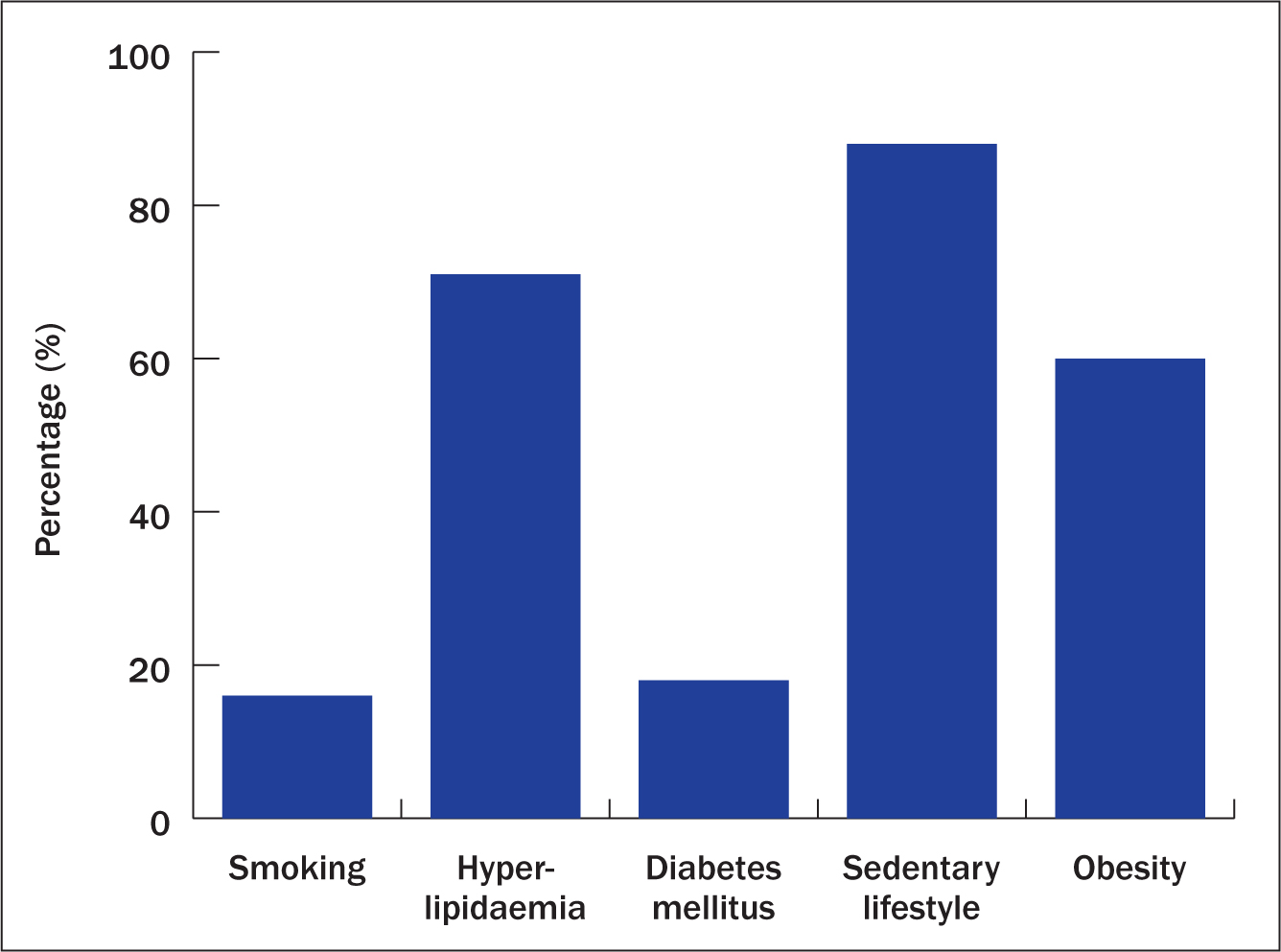
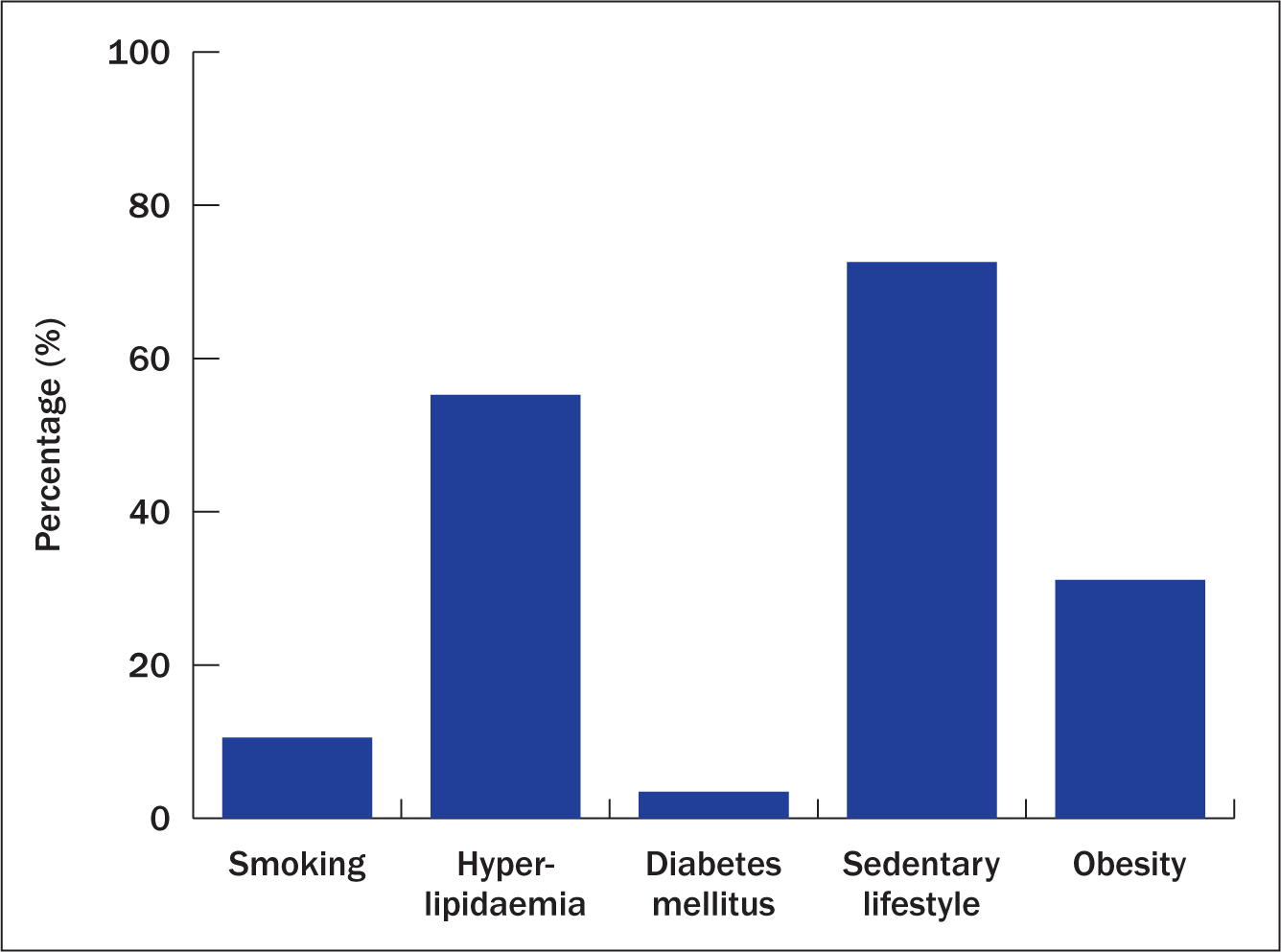
The mean age was 65 years and 56% were men in both samples. Moreover, hypertensive patients had higher systolic and diastolic blood pressures and were characterised by the presence of more risk factors than non-hypertensive patients. The incidence of cardiovascular risk factors is presented in Figures 1 and 2.
Evaluation of the scales
Internal consistency
The Cronbach alpha value in hypertensive patients was 0.76 for Hill-Bone, 0.64 for MMAS and 0.91 for A-14 scale, whereas in non-hypertensive patients it was 0.78 for the A-14 scale and 0.81 for MMAS. The authors did not calculate the Cronbach's alpha value for the Hill-Bone scale in the non-hypertensive group because the scale is a disease-specific questionnaire. In addition, the analysis indicated that there was no variance because all participants responded ‘no’ and ‘never’.
Discriminative validity
The results of the analysis between two groups for all scales are shown in Table 2. The difference in scores between the groups was statistically significant for all scales. Table 3 shows the results of the correlation analysis between similar items in the scales for the hypertensive and non-hypertensive groups.
| Scale | Group | t value | P value | |
|---|---|---|---|---|
| Hypertensive mean (SD) | Non-hypertensive mean (SD) | |||
| Hill-Bone | 20.32 (3.83) | 0.0 (0.0) | 30.89 | <0.01 |
| MMAS | 6.17 (2.72) | 0.0 (0.0) | 13.0 | <0.01 |
| A-14 | 11.41 (8.95) | 4.36 (4.34) | 4.0 | <0.01 |
| Hypertensive | Non-hypertensive | |||||
|---|---|---|---|---|---|---|
| Hill-Bone | MMAS | A-14 | Rho | P | Rho | P |
| Q1 | Q1 | -0.610 | <0.001 | |||
| Q1 | Q13 | 0.189 | 0.284 | |||
| Q1 | Q13 | 0.023 | 0.896 | 0.019 | 0.763 | |
| Q11 | Q6 | -0.732 | <0.001 | |||
| Q11 | Q7 | 0.177 | 0.317 | |||
| Q6 | Q7 | -0.214 | 0.223 | -0.147 | 0.236 | |
| Q9 | Q10 | -0.082 | 0.643 | |||
| Q4 | Q5 | 0.114 | 0.520 | 0.119 | 0.469 | |
Discussion
The present study examined the validity of three different scales to assess medication adherence among hypertensive and non-hypertensive people in Greece. The results indicated that these tools are valid to use in discriminating levels of adherence among both groups. The Cronbach's alpha value for the A-14 scale was 0.91 and 0.78 in hypertensive and non-hypertensive individuals respectively, which are high, since the calculated alpha value in the first validation of the tool was 0.861(Jank et al, 2009). For the Hill-Bone scale, the Cronbach's alpha value was also high at 0.76, compared with 0.80 in Kim et al (2000). However, the Cronbach's alpha value was significantly lower for MMAS in the study here compared with that calculated in Morisky et al (1986). The results of the present study are in concordance with those of Stavropoulou (2012). This finding may be attributed to the small numbers in each group.
The analysis found that the correlation between the items with similar meaning was not statistically significant apart from two questions for the hypertensive group: Q1 in both Hill-Bone and MMAS: ‘Do you forget to take your pills?’; and Q11 in Hill-Bone and Q6 in A-14 ‘Do you miss taking your pills when you feel better?’. The analysis indicated no significant correlation in the non-hypertensive group. The unproved correlation for all other items is associated with the complexity of the questions. Because the questions are not defined exactly in the same way, participants could interpret questions with a similar meaning in different ways. This point confirms one of the main disadvantages of questionnaires as a means for assessing different aspects of patients' lives.
Levels of adherence among hypertensive patients were characterised as moderate by MMAS (mean score 6.17) and low by the Hill-Bone (mean score 20.32) and A-14 scales (mean score 11.66). Therefore, patients with hypertension in Greece are characterised as not being adherent to their medication regimen. This affects the control of blood pressure, mortality rate and adverse clinical outcomes (Abegaz et al, 2017; Calip et al, 2017; Sung et al, 2017). In addition, Kim et al (2016) mentioned that poor adherence in hypertension is associated with higher risk of ischaemic heart disease and cerebral haemorrhage.
From the above, it is necessary to design interventions to enhance the level of adherence to medication regimens. Many studies have examined the effectiveness of such interventions. For example, Hacihasanoğlu and Gozum (2011) tested the effect of educational interventions in medication adherence and lifestyle recommendations among individuals with hypertension. The results indicated an enhancement in levels of adherence, although no difference in systolic and diastolic blood pressure was observed. Patients receiving interventions that were focused on both medication and lifestyle recommendations tended to adopt and follow the recommended behaviours to a higher degree than patients receiving interventions for only medication adherence or no intervention. Park et al (2013) proved that educational interventions resulted in better management of blood pressure and anxiety, and increased levels of adherence to medication and exercise. Finally, they found that the outcomes of the interventions lasted for long periods of time apart from the effect of adherence to antihypertension medication.
Apart from the effectiveness of clinical interventions, higher levels of adherence are associated with lower healthcare costs (Hill-McManus et al, 2018). Lloyd et al (2019) found that a 25% increase in level of adherence was associated with a US$13.7 billion decrease in healthcare costs each year. This saving is attributed to 7 million fewer in-hospital days and 100 000 fewer emergency department visits. Kymes et al (2016) found that the healthcare cost for adherent people with hypertension was US$4423 a year but US$7946 for non-adherent individuals.
Conclusion
The Greek versions of the Hill-Bone, MMAS and A-14 scales will be important tools for physicians and nurses in assessing patients' adherence to their regimens. They will be able not only to provide information for educational interventions to increase adherence levels, but also to assess the effectiveness of the applied interventions. Finally, the study provides further evidence of the applicability of these scales in clinical cardiovascular diseases care services.

