Occupational musculoskeletal symptoms are very common among intensive care unit (ICU) nurses. ICU nurses must provide care to their patients while managing physically demanding and complex tasks because of the nature of their work (Ulrich et al, 2014). A study of a stratified sample of 323 nurses working in the ICUs of 17 public, private, and university hospitals in Istanbul, Turkey, reported a 96% prevalence of musculoskeletal symptoms (Sezgin and Esin, 2015). Musculoskeletal symptoms in ICU nurses are related to:
Occurrence of musculoskeletal symptoms in ICU nurses leads to increased absenteeism, a higher risk of burnout, decreased quality of life, and lower job satisfaction (Türkmen et al, 2016; Ulrich et al, 2014; Shidhaye et al, 2011). Moreover, it affects the quality of care provided in the ICUs (Endacott, 2012). Considering the high level ergonomic risks in ICU settings and the link with negative health outcomes, there is a need for interventions aiming at reducing musculoskeletal symptoms in ICU nurses. This would not only aid in reducing absenteeism and the risk of burnout among ICU nurses, but also promote their health and wellbeing (Sezgin and Esin, 2015).
Occupational health services provided in hospital settings are accountable for undertaking regular ergonomic risk assessments of the ICU workforce using standardised and validated assessment tools. In this context, occupational health nurses have responsibilities related to the application and evaluation of risk-management interventions for improving the working conditions of the ICU workforce, as well as monitoring and keeping records of all processes (Esin and Sezgin, 2017). There is a need for more research on managing occupational conditions related to ergonomic risks to assist occupational health nurses.
The Omaha System
The Omaha System is a nursing classification system that has helped to make nursing interventions more visible, using nursing terminology, and supporting the collaboration of nurses working in different settings around the world. The Omaha System was developed in the 1970s in the USA, and was then translated and adapted into many languages around the world (Martin, 2005; Martin and Monsen, 2018a). The system is used to recognise nursing activities, allowing an evaluation of nursing interventions using a standardised and computerised approach. The system can be understood and used efficiently by occupational health nurses practising throughout the world by discussing specific cases selected from working communities from different countries. The number of Omaha System users has been rapidly increasing since the translations of the tool were made available in many countries. The system consists of three main components:
The system can be followed as a roadmap by its users to share a standard terminology through similar problems and conditions (Martin, 2005; Monsen et al, 2006). Use of the Omaha System in occupational health nursing practice to improve the health and safety of one ICU nurse will be described in this article.
Design
The primary purpose of this case study was to investigate the occupational musculoskeletal symptoms-related problems of one ICU nurse by using the standardised terms of the Omaha System.
Case study
A female ICU nurse (AB) was selected for the study after her informed consent was obtained. She worked in a state hospital in Istanbul, the most developed city in Turkey, where many people come to state hospitals to receive healthcare. This particular hospital was chosen because it is one of the busiest, with well-trained staff who provide high-quality and efficient healthcare. The hospital has six ICUs, including four reanimation units, one general ICU and one coronary ICU. AB worked in one of the reanimation units where adult patients receive care within a level 3 intensive care setting. Her unit was one of the most physically demanding settings because it required nurses to provide care to highly dependent patients leading to higher ergonomic risks. For example, nurses working in that unit were responsible for a minimum of three patients, which requires them to reposition their patients at least 18 times and to bend down to measure urinary drainage bags at least 36 times, during a 12-hour shift.
Data collection
The information about AB was gathered in May 2015 using two data collection tools and the computerised version of the Omaha System instrument.
An evaluation of knowledge form was developed by researchers as a self-reported form based on McAtamney and Nigel Corlett's (1993) Ergonomic Risk Assessment Guide, with the aim of gathering demographic, general health, working conditions, ergonomic risks and musculoskeletal symptoms-related data. The form's validity and reliability tests were performed by the researchers. Following confirmation from two academic experts in a university's public health nursing department, the form was accepted as valid (content validity). As the form was recommended for single-item questionnaires in the literature, a test-retest method was used for reliability of the pain intensity-related question. Its coefficient of stability, which varies between 0 and 1, was 0.78 and accepted as reliable since it was above 0.70.
The Rapid Upper Limb Assessment (RULA) tool was used for ergonomic risk assessment, developed by McAtamney and Nigel Corlett (1993) to observe upper limb movements that cause musculoskeletal symptoms. The Turkish validity and reliability tests of the RULA were carried out by Ozturk and Esin (2007). The content validity was performed by collecting individual expert opinions. This also included comparisons between three observers for inter-rater reliability of the tool (Cohen's kappa value was reported as between 0.20 and 0.35). Following these processes, the tool was accepted as valid and reliable (Ozturk and Esin, 2007). The RULA tool provides a quick assessment of muscle loading and body posture through simple observation.
The RULA tool consists of three scoring systems, which are calculated by combining relevant scores on matrix tables provided (McAtamney and Nigel Corlett, 1993):
| RULA total score of 1–2 | Acceptable |
| RULA total score of 3–4 | Further ergonomic analysis and modifications recommended |
| RULA total score of 5–6 | Further ergonomic analysis, modifications and preventive interventions are recommended |
| RULA total score of 7 | Immediate further ergonomic analysis, modifications and preventive interventions are recommended |
Following the Omaha System's Turkish adoption, its validity and reliability tests were carried out by Erdogan and Esin (2006). Its content validity was performed by gathering user feedback and an inter-rater reliability test was conducted with six independent users with median kappa statistics (Erdogan and Esin, 2006).
The Omaha System's three main components ensure that the users can identify actual or potential problems and health promotion needs, plan interventions, and evaluate outcomes at individual, family or community level (Martin, 2005; Erdogan and Esin, 2006; Erdogan et al, 2013):
Ethical considerations
Bezmialem Vakif University Clinical Research Ethics Committee approval was obtained before conducting the study (Ref. no. 28/11/2014-32). The nurse was contacted by one of the authors in person, gave informed consent to participate, and agreed to be investigated as an individual case study. This nurse was selected to be investigated as a case study because she had recently been diagnosed with a musculoskeletal disease.
Results
Evaluation of the case
Nurse AB was aged 28 at the time of the study and held a bachelor degree in nursing. She had been working in a reanimation ICU for the past 4 years. Her height was 165 cm and her weight 67 kg, with a body mass index of 24.60. She did not exercise regularly and her working schedule changed in an irregular order between the shifts 08:00-16:00 and 16:00-08:00.
She reported finding her work ‘quite intense’ and feeling ‘occasionally’ stressed at work. She was ‘somewhat satisfied’ with her salary, and had not attended any training related to management of ergonomic risks in her workplace. She was suffering from intense pain, which she reported as 7.4 out of 10, that was located on her upper back, lower back, legs and shoulders. Although having musculoskeletal symptoms, she continued to work and did not seek medical help until a recent lower back injury.
Ergonomic risks identified by RULA
AB's ergonomic risk scores were assessed during patient repositioning and bending down movements. During the patient repositioning movement, her RULA A score, which is associated with the arm, hand and wrist was 4, and her RULA B score was 5, indicating her neck, trunk and leg scores. The muscle load score of 2 was added, which addresses a repetitive load of 2-10 kg on her upper and lower limbs. According to this, her total RULA score during patient repositioning movement was 7.
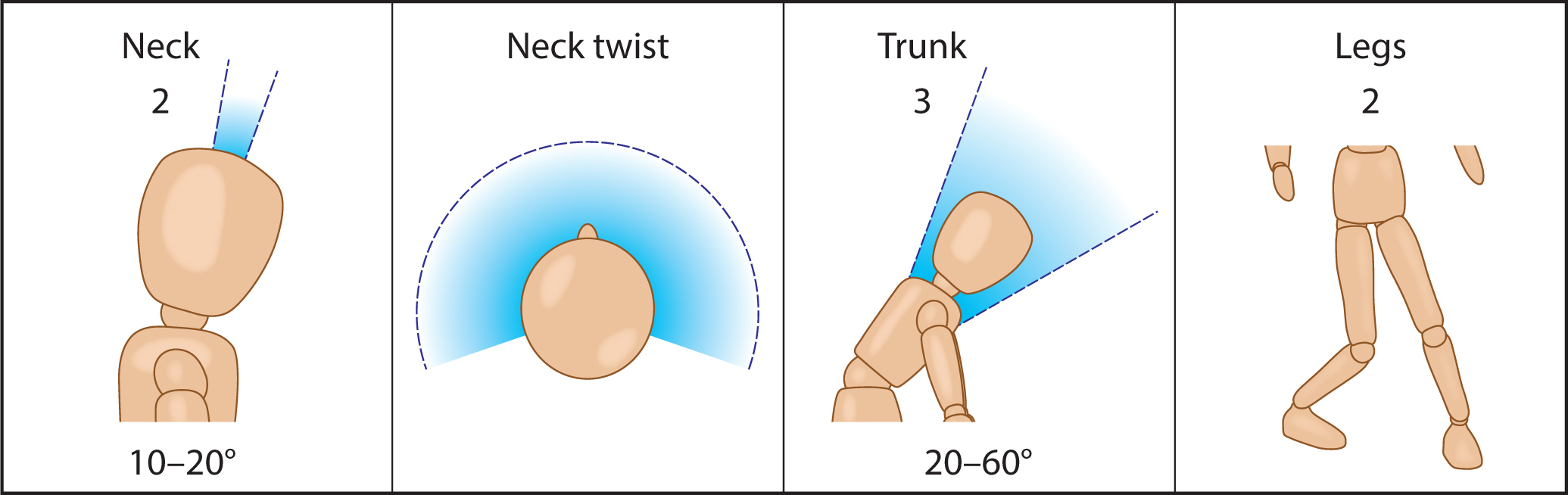
AB's RULA total score during bending down movements was assessed as 5. Her RULA A score was 4, and her RULA B score was 5 (Table 2). There was no muscle load score added, but her lower limb position was found to be inappropriate during the bending down movement which is demonstrated and mapped to the RULA tool (see Figure 1 and Figure 2).

| Score B | Trunk posture score | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 |
|
4 | 5 | 6 | |||||||
| Legs | Legs | Legs | Legs | Legs | Legs | |||||||
| Neck | 1 | 2 | 1 | 2 | 1 |
|
1 | 2 | 1 | 2 | 1 | 2 |
| 1 | 1 | 3 | 2 | 3 | 3 | 4 | 5 | 5 | 6 | 6 | 7 | 7 |
|
|
2 | 3 | 2 | 3 | 4 |
|
5 | 5 | 6 | 7 | 7 | 7 |
| 3 | 3 | 3 | 3 | 4 | 4 | 5 | 5 | 6 | 6 | 7 | 7 | 7 |
| 4 | 5 | 5 | 5 | 6 | 6 | 7 | 7 | 7 | 7 | 7 | 8 | 8 |
| 5 | 7 | 7 | 7 | 7 | 7 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| 6 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 9 | 9 | 9 | 9 | 9 |
Problems identified using the Omaha System
AB's signs and symptoms related to problems mapped to the Omaha System Problem Rating Scale for Outcomes are presented in Table 3. AB's problems were identified as being based on the ‘individual’ level. Potential problems and health promotion-related problems were not included in the care plan because her actual problems needed to be resolved first.
| Domain | Problem | Signs/symptoms | PRS* before interventions (1-5)K/B/S** | Intervention category*** | Target | Client-specific information | Care description | PRS after interventions (1-5) K/B/S** |
|---|---|---|---|---|---|---|---|---|
| Environment | Neighbourhood/workplace safety | Inadequate space/resources to foster health | 3/2/2 | TGC | Environment | Workplace hazards |
Training provided | 4/4/3 |
| Physical hazards | 2/1/2 | TP | Safety | Monitoring safety risks | Ergonomic risk assessment were performed using RULA^ | 4/3/3 | ||
| CM | Environment | Reporting hazards |
Reported to occupational health and safety office | |||||
| S | Safety | Monitoring safety risks |
Follow-up | |||||
| Environment | Providing appropriate/safe environmental conditions | |||||||
| Physiologic | Pain | Compensated movement/guarding | 2/3/2 | TGC | Signs/symptoms-physical | Signs/symptoms: physical (location/left flank, pain scale, vital signs, non-verbal cues) Conditions requiring to call upon help from health professionals | Training provided | 4/3/3 |
| TP | Signs/symptoms: physical | Signs/symptoms: physical (location/left flank, pain scale, vital signs, non-verbal cues) | Physical assessment performed | |||||
| Expresses discomfort/pain | 2/2/2 | CM | Physical therapy care | Coordination between service providers | Physical therapy options | 4/3/3 | ||
| Restless behaviour | 2/2/3 | S | Signs/symptoms-physical | Signs/symptoms-physical (location/left flank, pain scale, vital signs, non-verbal cues) | Follow-up | 3/3/3 | ||
| Neuro-musculo-skeletal function | Decreased muscle strength | 3/2/2 | TGC | Exercises | Recommending exercise programme | Training provided | 4/4/3 | |
| CM | Physical therapy care | Coordination between service providers | Physical therapy options | |||||
| S | Signs/symptoms: physical | Signs/symptoms: physical (location/left flank, pain scale, vital signs, non-verbal cues) | Follow-up | |||||
| Health behaviours | Physical activity | Inadequate/inconsistent exercise routine | 3/2/2 | TGC | Exercises | Recommending exercise programme |
Training provided | 4/3/3 |
| Behaviour modification | Increasing activities | |||||||
| CM | Physical therapy care | Coordination between service providers | Physical therapy options | |||||
| S | Behaviour modification | Maintaining behaviour |
Follow-up | |||||
| Wellness | Evidence of change | |||||||
| Healthcare supervision | Fails to obtain routine/preventive healthcare | 2/2/2 | TGC | Medical/dental care | Following the care plan Protection/maintenance | Training provided | 4/4/3 | |
| Fails to return as requested to healthcare provider | 2/1/2 | Signs/symptoms: physical | Unfulfilled health needs (disregarded medical conditions) | 4/4/3 | ||||
| CM | Medical/dental care | Therapy/treatment | A GP visit recommended | |||||
| S | Wellness | Healthcare | Follow-up |
Key:
PRS: Problem Rating Scale
RULA: Rapid Upper Limb Assessment
K/B/S: Knowledge/Behaviour/Status
Knowledge (ability of the client to remember and interpret information) 1: No knowledge, 2: Minimal knowledge, 3: Basic knowledge, 4: Adequate knowledge, 5: Superior knowledge
Behaviour (observable responses, actions, or activities of the client fitting the occasion or purpose) 1: Not appropriate, 2: Rarely appropriate, 3: Inconsistently appropriate, 4: Usually appropriate, 5: Consistently appropriate
Status (condition of the client in relation to objective and subjective defining characteristics) 1: Extreme signs/symptoms, 2: Severe signs/symptoms, 3: Moderate signs/symptoms, 4: Minimal signs/symptoms, 5: No signs/symptoms
TGC: Teaching, guidance and counselling, TP: Treatment and procedures, CM: Case management, S: Surveillance
The Problem Rating Scale for Outcomes used to evaluate knowledge, behaviour and status (before and after interventions) for the identified signs and symptoms related to problems are indicated in Table 3. For example, ‘knowledge, behaviour and status’ for ‘Expressing pain/discomfort’ sign of the pain problem were ‘minimal knowledge’, ‘rarely appropriate behaviour’ and ‘severe signs/symptoms’, respectively. Following teaching, guidance and counselling, treatment and procedures, case management, and surveillance interventions, nursing outcomes were improved as ‘adequate knowledge’, ‘inconsistently appropriate behaviour’ and ‘moderate signs/symptoms’ when evaluated at the end of a 6-month follow-up period (Table 3).
The care plan designed and implemented using the Omaha System is shown in Table 3, which describes nursing interventions selected from the Omaha System's 75 targets listed on the intervention scheme.
Discussion
This case study described the implementation of Omaha System steps on the identification of ergonomic-risks-related musculoskeletal problems in an ICU nurse and illustrated how the application of interventions improved her physical condition and managed work-related ergonomic risks.
AB's problems related to her workplace safety, pain, musculoskeletal symptoms function, physical activity, and healthcare supervision, which are mapped to the Omaha System terms discussed below.
Workplace safety
Nurse AB had severe ergonomic risks in her workplace environment which were identified using the RULA tool. Her RULA total score of 7 during patient repositioning meant that immediate further ergonomic analysis, modifications and preventive interventions for her working conditions were recommended. AB's bending down movement was scored as 5 using the RULA tool, so further ergonomic analysis, modifications and preventive interventions in the working environment were recommended (McAtamney and Nigel Corlett, 1993).
Intensive care units have the highest risks in terms of workplace safety and ergonomic risks in hospitals (Sezgin and Esin, 2015). A risk assessor is needed in ICU settings to monitor ICU nurses' ergonomic risks for continuous periods. The RULA tool can be used as a valid and reliable assessment approach to identify these ergonomic risks. However, the tool requires a training period for the assessor before application. Following the training, the assessor needs to practise by using the tool numerous times to become a competent RULA assessor (McAtamney and Nigel Corlett, 1993).
The interventions applied to improve ergonomic conditions were related to teaching, guidance and counselling, including a follow-up period of 6 months for surveillance. At the end of the follow-up period, AB reported increased knowledge, and improved behaviour and status was observed in relation to her workplace safety. Nurses caring for patients in ICU settings around the world have serious musculoskeletal symptoms associated with high ergonomic risks. Compared with high-income level countries nurses in developing countries suffer from higher level of ergonomic risks due to limited availability of lifting equipment in their work environments and because they work in under-staffed units (Esin and Sezgin, 2017).
Pain and neuro-musculoskeletal function
AB was suffering from intense pain which she reported as 7.4 out of 10 and also reported decreased muscle strength. A case-management approach was adopted. Following training related to exercises, ergonomic risks, body mechanics, behaviour modification and discussing physical therapy options, her pain was reduced (described as 4.9 out of 10 at the end of the follow-up period). This progress in her condition was mapped to the Omaha System Problem Rating Scale for Outcomes as her pain status was improved from ‘severe sign-symptoms’ to ‘moderate sign-symptoms’.
Physical activity
AB had an inadequate/inconsistent exercise routine as identified on the Omaha System. Training and guidance were provided on the importance of adopting an appropriate exercise routine to strengthen muscles in her back. She was also advised to consider physical therapy options. At the end of the surveillance, she reported that she had begun taking moderate exercise regularly. Research has shown that there is a direct link between doing routine exercise and a reduction in musculoskeletal symptoms (Esin and Sezgin, 2017). Including exercise rooms in workplace settings to help prevent musculoskeletal symptoms would be helpful. However, many nurses do not have such facilities in their workplaces, especially in low-resource settings.
Healthcare supervision
AB was observed to be failing to obtain routine healthcare to manage her symptoms. Training and guidance followed by case management interventions increased her awareness of the importance of self-management of her health and musculoskeletal-related symptoms. The consequences of ignoring her musculoskeletal symptoms and not coordinating with a healthcare specialist regularly were discussed. Following this intervention, AB reported visiting her physician regularly. It was disappointing to observe that AB had not received any routine/preventive healthcare in her workplace, despite the fact that nurses are key members of the healthcare team and management has the responsibility to improve the health of individuals.
Nurses have roles and responsibilities in the prevention of diseases and in promoting the health of individuals, families and communities, providing care for patients with acute and chronic health conditions, and supporting them to use rehabilitation services. Occupational health nurses with a background in public health nursing are key professionals to improve work-related health conditions, especially in work environments with increased health risks as ICU settings. In this context, occupational health nurses have an important role in improving the occupational health-related problems of ICU nurses. In this study, the Omaha System was used to identify and prioritise the ergonomic risk-related musculoskeletal problems of ICU nurses, and to plan interventions and evaluate outcomes.
Conclusion
The Omaha System can be used to identify workplace and ergonomic risks related to the musculoskeletal symptoms of ICU nurses. The authors recommend that occupational health nurses apply suitable interventions related to teaching, guidance and counselling, case management, treatments and procedures, or practise surveillance in accordance with the Omaha System in their ICUs. There is a need to use standardised global nursing terminology and nursing classification systems to make nursing interventions visible, and to collaborate with other disciplines.
Recommendations
Musculoskeletal system symptoms can be prevented by ergonomics training and risk assessments for continuous periods, improvements to working conditions, and implementation of health-promotion activities such stress management and regular exercise.
The Omaha System can be implemented in any nursing area of practice by using its main components: Problem Classification Scheme, Intervention Scheme, and Problem Rating Scale for Outcomes.
The Omaha System enables occupational health nurses to identify, manage, and monitor musculoskeletal system symptoms arising from ergonomic risks in ICU settings.

