Surgical and preoperative disinfection techniques have evolved over the centuries, from the birth of modern surgery in the early 19th century, to the first use of carbolic acid for disinfecting surgical incisions, helping to prevent surgical site infections in the 1890s, through the discovery of antibiotics in 1928, to the first whole eye and partial face transplant, which was performed in 2023 (Whitlock, 2024). These advances in surgery have led to improved surgical patient outcomes, reduced hospital length of stays and reduced incidences of avoidable infections. Sadly, these advancements are set against a rise in antimicrobial resistance and infectious diseases. This calls for urgent revolutionary strategies to tackle escalating threats to health care and humanity in general.
Published surgical site infection (SSI) guidelines that span the surgical pathway (preoperative skin preparation, appropriate surgical antibiotic prophylaxis, intraoperative practices and postoperative wound care and recovery), are available (Berríos-Torres et al, 2017; World Health Organization (WHO), 2018; National Institute for Health and Care Excellence (NICE), 2020). However, compliance with evidence-based recommendations or bundles has been reported to be poor or actions have not been recorded accurately.
The newly formed global SSI Prevention (SSIP) group (SSIP, 2023) aims to address SSI prevention bundle compliance issues, among other SSI surveillance and prevention priorities, via a proposed SSIP champion model that facilitates dedicated and delegated responsibility for implementing SSI prevention science in all healthcare organisations globally. SSIP proposals support the concept of ‘getting it right first time’ for each surgical patient through a strong emphasis on prevention.
Appropriate surgical patient preoperative preparation, which covers skin preparation, plays a critical role in the prevention of avoidable harm and is an important marker of surgical patient outcomes. Preoperative skin decolonisation or bathing is therefore an important intervention in infection prevention and will be a focus for this article. There is ongoing debate on whether to use antimicrobial agents or just plain soap as a measure to reduce transient microbial flora, which should in turn reduce the incidence of surgical incision contamination, potentially reducing the risk of avoidable infections and, in particular, SSIs.
This article will present an exploration of some of the available evidence with pragmatic recommendations based on the author's experiences of being a global SSI surveillance and prevention champion.
Preoperative bathing
Preoperative bathing is a generally accepted practice within surgery as a measure to reduce the risk of avoidable surgical site infections. Evidence to favour the routine use of antimicrobial agents is weak, a reason why most SSI guidelines such as those from NICE (2020) and WHO (2018) generally do not recommend their routine use.
In the USA, however, antimicrobial agents such as chlorhexidine gluconate (CHG) baths or CHG-impregnated cloths have been widely accepted as part of SSI prevention bundles, as well as part of strategies to tackle multidrug-resistant pathogens and bloodstream infections in intensive care units (Huang et al, 2019). The differences in acceptance of routine use of antimicrobial preoperative skin agents between countries have led to continued debates on whether to use plain soap or antimicrobial agents to decolonise the skin prior to various surgical procedures. An increased focus on patient safety and experience calls for a pragmatic approach when considering adopting cost-effective bundled interventions that have the potential to reduce avoidable harm or the incidence of SSIs and other healthcare-associated infections (HCAIs) in various settings.
A practical example
As an example, Chiwera et al (2018) adopted an SSI prevention care bundle that included the use of preoperative baths/wipes based on local microbiology results from infected adult cardiac surgery wounds, despite weak evidence around the effectiveness of preoperative skin decolonisation with antiseptic agents. This decision may reflect the complexity of cases presenting to a large acute tertiary referral centre in the UK, which supports recommendations to adapt multiple strategies to overcome SSI bundle contextual and implementation barriers (Dukes et al, 2024). Each setting must therefore collect robust SSI data and review microbiology results (antibiograms) accordingly to facilitate prudent decision making.
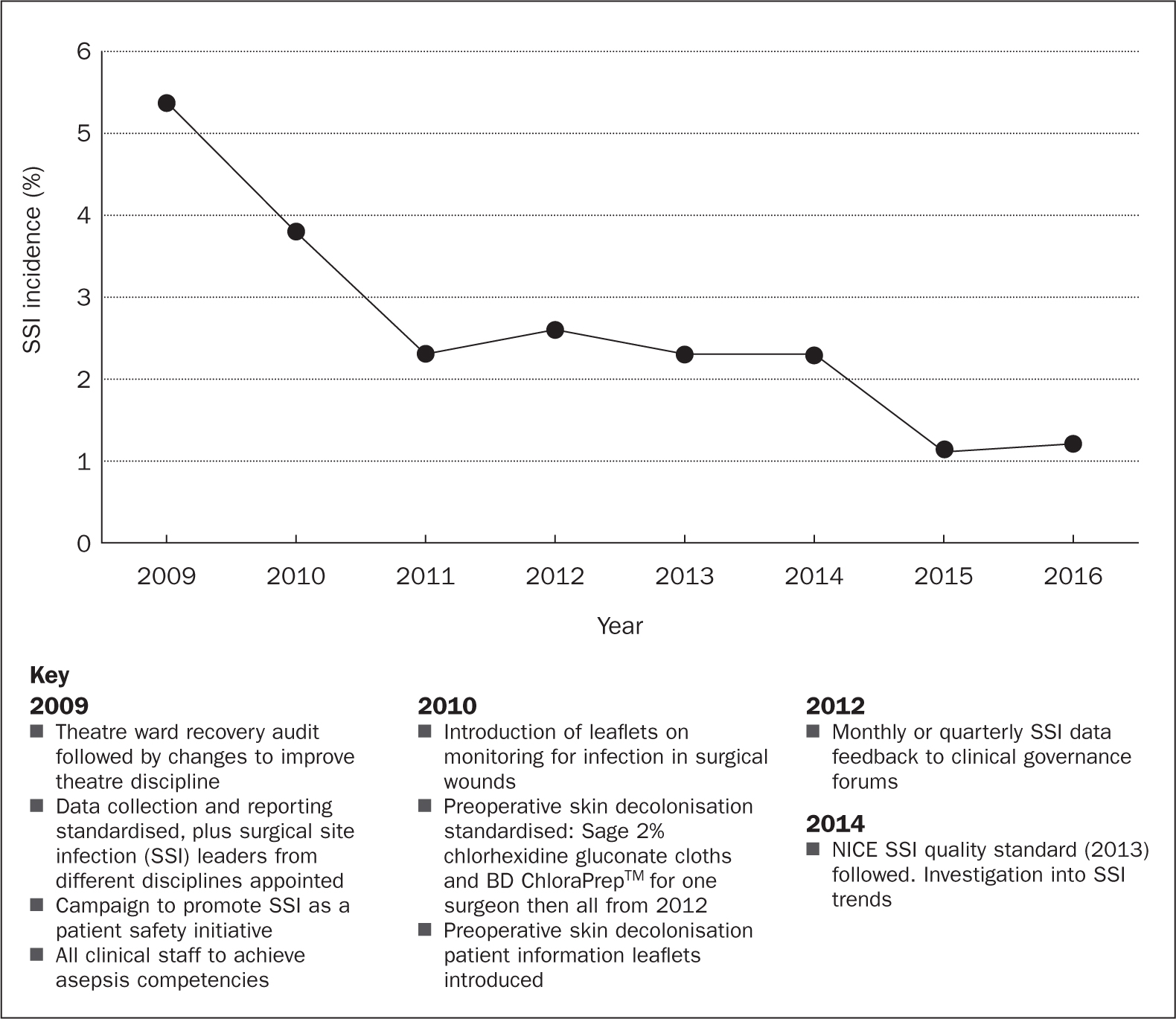
Chiwera and colleagues reported that meticulous attention to preoperative bathing or preoperative skin decolonisation contributed to the overall reduction in avoidable SSIs (Chiwera et al, 2018). The author remembers celebrating with colleagues when they recorded significant reductions (from about 9% to 1%) in avoidable SSIs within adult cardiac surgery within a year of standardising preoperative skin decolonisation. The author had been dreaming of this achievement – reducing avoidable harm for patients because she had always pushed for a zero-tolerance approach to avoidable SSIs (Chiwera et al, 2018). By combining this intervention with other evidence-based SSIP recommendations in line with NICE SSI guidance, the team demonstrated sustainable SSI reductions over several years within cardiac surgery and other surgical specialties using an SSIP champion model, which is now being adopted for the new global SSIP work (NICE, 2013; 2017; Chiwera, 2023) (Figure 1).
The preoperative skin decolonisation bundle used by Chiwera and colleagues (2018) consisted of:
- Preoperative washes with CHG for each cardiac surgery patient on the night before surgery
- A second wash on the day of surgery with CHG washes or wipes
- Preoperative skin decolonisation patient information leaflets or videos with clear easy-to-understand instructions for patients and for staff
- Laminated leaflets displayed in bathrooms to help patients carry out the procedure correctly ie, to start with cleaner areas of the body and finish with the most contaminated parts, such as the groin
- Leaflets were also made accessible via the organisation's intranet pages (internal and public pages) as well as on the trust's SSI pages
- All staff were taught how best to ensure preoperative skin decolonisation was thorough during one-to-one meetings, monthly infection prevention and control (IPC) link practitioner meetings, audit meetings, ward meetings and other relevant forums
- Pre-assessment staff were instructed to give preoperative skin decolonisation instructions to all prospective surgical patients at initial contact, with an emphasis on using the correct technique when washing – ‘starting with cleaner areas of the body and finishing with the dirtiest parts’
- Staff were encouraged to undertake appropriate risk assessments at this stage (pre-assessment) to identify patients who needed support due to their age or comorbidities
- Suppliers of products used for preoperative washes were encouraged to develop easy-to-use instructions or work with the organisation to produce contextual educational material and then help to deliver the required education or support to clinical teams.
It is interesting that Edmiston and Leaper (2017) reported on a similar preoperative skin decolonisation bundle with an emphasis on improving compliance with recommended techniques such as CHG contact time with the skin for optimum effectiveness. Poor SSI prevention bundle compliance appears to limit reproducibility of SSI data in general as it becomes difficult to conclude whether certain interventions that are part of an SSI bundle work (Leaper et al, 2015, Tanner et al, 2016). This may be one of the reasons why, despite it being a widely accepted preoperative intervention, preoperative bathing with antiseptic agents is not currently recommended in published guidelines.
With micro-organisms being ubiquitous in nature, it is important to ensure that skin preparation solutions with 99.999% efficacy are given the best chance of preventing avoidable infections. Reducing bacterial bioburden is therefore of paramount importance for all surgical patients. The higher the bacterial load before pre-incision skin preparation with an antiseptic solution, the higher the chances that one colony-forming unit will potentially cause devastation for surgical patients.
Blanket or targeted approaches
Debates on whether blanket decolonisation is a cost-effective intervention for preventing avoidable infections are ongoing. There is strong evidence to support the use of nasal mupirocin in combination with a CHG body wash before procedures in which Staphylococcus aureus is a likely cause of a surgical site infection or depending on local contextual factors (NICE, 2020). Where indicated, staff must weigh the cost-effectiveness of blanket decolonisation as opposed to targeted screening and decolonisation when contextually appropriate, bearing in mind sustainability, local evidence recorded in antibiograms, resource implications and other identified local risk factors.
Bundled approach interventions with strong leadership/governance focused on embracing preoperative skin decolonisation aspects are needed as a first step in getting it right for surgical patients. For example, results from published adult cardiac SSI prevention data highlight the benefits of standardising preoperative skin decolonisation at the very start of important SSIP campaigns, coupled with other SSI prevention interventions in line with NICE guidance (Chiwera et al, 2018).
It is interesting that studies on the evaluation of preoperative skin decolonisation included in the WHO guideline appear to highlight an important aspect of the care bundle that Chiwera and colleagues (2018) addressed in their work – patient information: ‘Of note, no written instructions were provided to patients in the control group in most studies. This may have potentially resulted in less thorough washing than in the intervention group.’ (WHO, 2018).
CHG-impregnated cloths were shown to be superior to CHG baths, albeit it is acknowledged that washes are better in the presence of organic matter or when patients had opened their bowels, for example. It makes sense microbiologically, although ongoing research is also needed to address potential concerns around antiseptic resistance or allergic reactions. This will be covered under SSIP's new research and innovation proposals (SSIP, 2023).
Patient involvement
Patient involvement is key, as emphasised in the 2023 WHO patient safety campaign ‘Engaging patients for patient safety’ with the theme ‘Elevate the voice of patients’ (WHO, 2023) and a report by The King's Fund ‘Making shared decision a reality: no decision about me, without me’ (Coulter and Collins, 2011).
The government wants to place patients' needs, wishes and preferences at the heart of clinical decision-making, a vision articulated by the phrase ‘nothing about me, without me’ (Department of Health, 2012).
This is also reflected in the adoption of Martha's Rule, which began to be rolled out in England in April 2024 (Graham et al, 2024). The rule places emphasis on patient-centredness, where clinicians, patients or their relatives may seek a second opinion when managing potential or confirmed sepsis or for patients whose condition is deteriorating.
Putting patients at the centre of all decisions about their care should always be bundled with proposed SSI prevention recommendations or other patient safety interventions to optimise outcomes for all patients. Given that most infections that patients present with may be from patients' own bacterial flora, patient washing or hygiene is core to preventing avoidable harm from healthcare-associated and community origin infections, which include sepsis and surgical site infections.
Edmiston and Leaper (2017) argued for the use of preoperative skin decolonisation with an antiseptic solution or cloths and put forward a compelling case for addressing compliance issues with recommended interventions. They highlight a lack of standardisation in studies that have been included in Cochrane collaborations or systematic reviews as a potential setback. It is clear that a few of the SSI studies to date do not include SSI prevention compliance data, as alluded to by Tanner et al (2016). Using CHG washes or cloths pragmatically may be a sensible option in the absence of credible SSI research that includes evidence-based SSI prevention compliance data. Chen and Mont (2023) used CHG-impregnated cloths as one of the fundamental cornerstones for reducing periprosthetic infections after primary lower extremity total joint arthroplasties.
Even with limited evidence to support the routine use of preoperative skin decolonisation with an antiseptic agent solution in surgical patients, recommendations for its use based on local risk assessments appear sound in the absence of compliance data – a common finding in most SSI studies. Adopting a holistic approach to generic HCAI reduction, using antiseptic agents as part of preoperative skin decolonisation regimens, may protect patients from IV line-related bacteraemia caused by skin commensals. Chapman et al (2021) reported on significant reductions in central catheter-associated bloodstream infections through adoption of a standardised CHG bathing programme. Part of the success in these areas may be attributable to good compliance, given staffing in these areas is usually one health professional to one patient.
Benefits are also reported in preoperative patients, where Chapman et al (2021) reported up to 45% HCAI reductions with standardised CHG baths. Furthermore, Chan et al (2019) reported benefits from using CHG washes in clean spinal surgical procedures.
However, no benefit was reported in a cohort of craniotomy procedures (Ammanuel et al, 2021), which may reflect differing benefits depending on the site of procedures.
Other impressive reductions in HCAIs were demonstrated in the same organisation where Chiwera et al (2018) and Tipper et al 2019) reported significant SSI reductions by employing an SSIP bundle that incorporated antiseptic preoperative washes/cloths as part of preoperative skin decolonisation regimens.
The use of bundled approach interventions has been supported by various SSIP literature including a systematic review and cohort meta-analysis of more than 8000 patients by Tanner et al (2015). Only two studies in this analysis evaluated CHG as part of an SSIP bundle, which may limit its applicability to preoperative skin decolonisation. However, in their conclusion, Tanner et al (2015) acknowledged that, even without consensus on what comprises an optimal colorectal surgical care bundle, a multidisciplinary approach, evidence-based core strategies and ‘adjunctive interventions that enhance wound defence mechanisms while limiting exogenous, intraoperative contamination will result in a reduced risk of infection in the colorectal patient population’. The adjunctive interventions can include preoperative skin decolonisation as a means for limiting exogenous contamination, which may not just reduce SSI risk but associated collateral damage such as IV line-related bacteraemia.
A new SSI prevention era with SSIP
SSIP (2023) is a newly formed global SSI prevention patient safety collaborative that will consist of a core group with oversight of planning and delivery of the work programme, various SSI prevention initiative workstreams and members who wish to be part of this important surgical patient safety initiative. After a successful collaborative campaign, the group has now identified five key strategic aims:
- Increasing visibility and activism around SSI prevention
- Improving uptake of evidence-based SSI prevention recommendations in all healthcare and community settings
- Championing dedicated and delegated responsibility for SSI prevention implementation science via an SSIP champion model in all healthcare and community settings.
- Reducing avoidable surgery-related harm in all patients/animals via a ‘one health approach’, which supports robust SSI surveillance and prevention strategies in all settings
- Advancing SSI research and innovation.
The above strategic aims will be achieved via a set of key SSIP objectives:
- Establishing and sustaining annual SSIP events
- Development and introduction of annual SSI prevention appraisal tools (quality improvement/peer review tools) that will be used by SSIP champions to appraise evidence-based SSI prevention measures
- Developing and sustaining an SSIP champion model at local hospital, regional and country level that encompasses a variety of health professionals and consumers of health care.
SSIP proposals derive from the author's SSI surveillance and prevention experiences coupled with relentless campaigns to raise the profile of SSIs globally. Chiwera (2018) highlighted that a bundled approach to interventions works better when a holistic approach to patient safety is adopted. This is achieved by prioritising clinical ownership, embedding recommendations within existing governance structures, incorporating educational elements within organisations' induction and ongoing educational support programmes, including cleaning and decontamination, ventilation, and all aspects of the healthcare environment in surgical patient safety or quality improvement initiatives (NICE, 2017).
SSI prevention bundle compliance and adopting a holistic patient safety approach will be an area of particular focus and further research as part of the newly formed SSIP group's surgical patient safety proposals. The use of an SSIP champion model will facilitate identification and addressing of potential challenges. Dedicated SSIP champions will have responsibility for human factors and implementation science in their organisations. This will involve thoroughly scrutinising surgical governance pathways and associated continual quality improvement programmes. SSIP will collaborate with various healthcare stakeholders and consumers of health care to improve uptake of evidence-based SSI prevention recommendations, of which preoperative skin decolonisation is a big part.
Conclusion
There is no doubt that preoperative skin decolonisation is an important first step on the road to ‘getting it right first time’ for each surgical patient. Context and setting are important considerations and so are human factors and ergonomics. It is clear from published data that bundled approach interventions reduce incidences of HCAI. Preoperative patient preparation, which includes screening for micro-organisms of concern, providing the right antibiotic prophylaxis, and following the correct procedures and behaviours in the operating room, plus the surgeon's technique, and staff and patient education, all play an important part in preventing avoidable harm for surgical patients.
It is hoped that the new SSIP champion model being proposed by the SSIP group will enable thorough evaluations of SSI prevention interventions. Healthcare settings should be able to address SSI bundle compliance issues and improve reporting and appropriate or applicable quality improvement strategies to improve surgical patient outcomes under the proposed model. Digital health technologies will be integral to enhancing compliance and outcomes in relation to SSIP interventions uptake and will be fully explored as part of broader SSIP aims and objectives that all aim to improve surgical patient safety globally.


