The majority (70%) of ostomates experience peristomal complications with the most prevalent being skin damage (Gray et al, 2013). Bianchi (2013) highlighted the importance of clinicians having a good understanding of the cause of skin breakdown and how to treat it; this was followed up with research that showed that repeated application or removal of appliances such as dressings and pouches can strip the skin, causing inflammation, oedema and pain (Bianchi, 2013).
Skin damage
The skin has three layers—the epidermis, dermis and subcutaneous tissue—which all absorb, excrete, protect, secrete, thermoregulate, produce pigment, perceive senses and provide a safe environment.
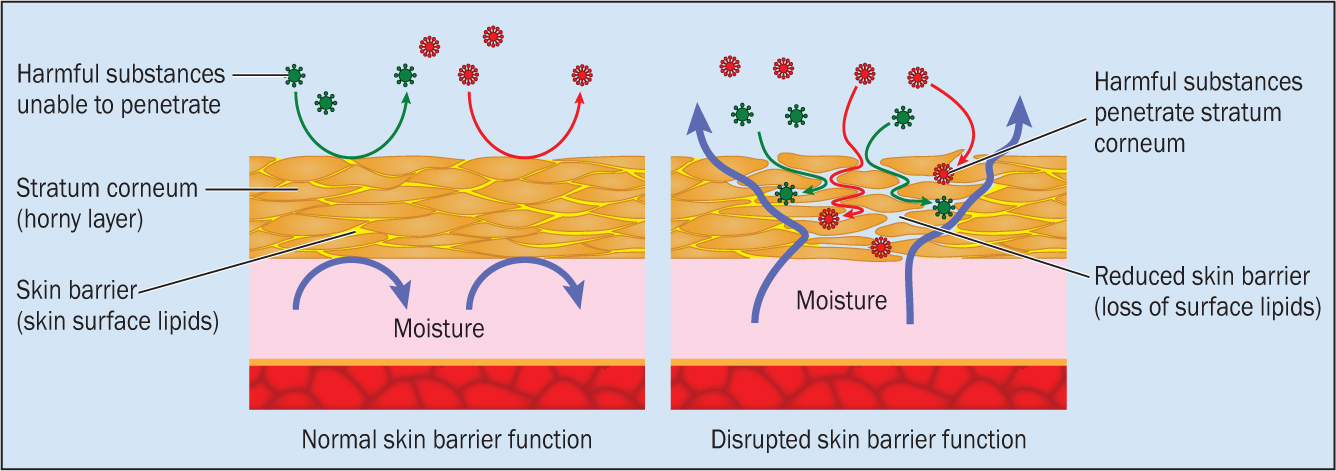
Transepidermal water loss (TEWL)—water transferred from the body to the environment, e.g. perspiration—can increase when skin dysfunction such as skin stripping, infection or eczema occur, causing difficulty with pouch adherence. TEWL is not always visible so patients may be unaware there is an impaired barrier function.
The stratum corneum of the epidermis, the skin's uppermost layer, provides a physical barrier against the external environment (Figure 1). Maintenance of this barrier is essential to protect the skin because disruption, such as that caused by dryness or overhydration, predisposes the skin to breakdown (Figure 2) and makes it more susceptible to damage by friction or shearing forces such as an incorrect pouch size (Hahler, 2006).
Moisture-associated skin damage (MASD) is defined by Voegeli (2013) as skin damage that occurs as a result of prolonged exposure of the skin to moisture such as that from stool, urine, perspiration and exudate. It is characterised by inflammation of the skin with or without erosion or a secondary cutaneous infection. Four of the most common conditions that result from MASD are:
Certain factors can contribute to skin breakdown; these are commonly classified as intrinsic and extrinsic factors.
Intrinsic factors include ageing skin with thinning of the epidermis, loss of dermal matrix and subcutaneous tissue, reduced vascularity, elasticity, strength and moisture, and comorbidities of diabetes, renal failure, hypertension and immunosuppression (Boyles and Hunt, 2016).
Rudoni (2008) and Cronin (2008) described extrinsic factors as:
Boyles and Hunt (2016) stated more recently that certain ethnic groups have been shown to be more prone to skin injury, as darker skin has a higher degree of rigidity. This is an important factor when assessing patients.
For the purpose of this supplement, this article will focus on peristomal skin.
The stoma
A stoma is an artificial opening, surgically created as a means of diversion for faeces or urine; it can be temporary or permanent (Kelly O'Flynn, 2018). There are three types of stoma:
There is no gold standard for changing ileostomy and urostomy pouches but manufacturers recommend changing them every 3 days.
The importance of maintaining skin integrity through ensuring pouch appliances and accessories are the correct size to prevent effluent leaking onto the skin was highlighted in Boyles and Hunt's (2016) discussion. They also discussed complications after stoma formation, which can occur at any stage; these include stoma retraction, stenosis, prolapse, parastomal hernia, mucocutaneous separation and pyoderma gangrenosum. These can prevent the pouch from adhering to the skin effectively, so extra accessories or an alternative pouch may be required to ensure an effective seal. These complications are described in Table 1.
| Condition | Definition | Intervention |
|---|---|---|
| Mucocutaneous separation | The stoma separates from the skin, leaving a visible gap of tissue; it is caused by bowel tension, infection, malnutrition or steroid use | Prevent leakage to prevent infection. It is typically treated with protective powder, then a barrier cream/film seal to protect surrounding skin. Alginate/hydrofiber dressings may be required |
| Retraction/flush stoma | The stoma retracts into the abdomen; this is caused by a change in the size or shape of stoma as a result of loss or gain in weight, tension in the bowel or ischaemia | Convex appliances assist with creating a seal and preventing leaks; a barrier film should be used to protect skin integrity and close observation is required to check any ulceration caused by the extra pressure of convexity |
| Stenosis | The stoma opening narrows making it difficult to pass the stool; it is caused by ischaemia, stool retraction, Crohn's disease and radiation treatment of intestine | The spout can be widened with a method of dilation performed by a stoma care nurse or the surgical team. In severe cases, surgical revision of the stoma may be required |
| Prolapse | The stoma protrudes further out than when formed; this is caused by weakened muscle wall secondary to stoma formation, ongoing constipation or chronic coughing | Pouch and accessory sizes should be assessed to ensure an effective seal. Barrier film should be used to ensure protection of skin and aid of appliance adherence |
| Parastomal hernia | The patient feels a dragging sensation but usually no pain. A bulge can be observed behind the stoma, which is secondary to a complication of stoma formation, being overweight, heavy lifting or strenuous exercise | Ostomates should be advised to avoid heavy lifting and wear supportive clothing/hernia belts. Surgical intervention is carried out only if the bowel is obstructed |
| Granulomas | These red nodules around the stoma can bleed but are not normally painful; they are caused by friction of effluent or irritation of incorrect pouch size | Assess for cause; silver nitrate treatment may be required to shrink them. Apply protective powder and barrier film/cream to ensure protection and a seal may also be required |
| Pancaking | This is a common occurrence in colostomists; a bowel motion gets stuck around stoma and can irritate the skin, | Ostomates should be advised to increase fluid intake, take bowel softener, and create weight in pouch (for example, by putting a screwed-up piece of tissue/baby oil inside) to aid motion to slide in and prevent vacuum of pouch. Barrier film/cream should be applied to protect skin integrity from effluent if it pancakes onto the skin |
| Peristomal pyoderma gangrenosum | This affects 50% of ostomates with inflammatory bowel disease. It accounts for 0.6% of all peristomal skin conditions and is characterised by ulcerative, pustular lesions/crater with extreme pain | Topical steroid treatments as prescribed care under the surgical and dermatology teams |
Stoma appliances
Healthy peristomal skin is essential to ensuring effective pouch adherence, which prevents effluent from seeping onto the skin (Boyles, 2010). The aim of good stoma management is to prevent peristomal skin soreness and, if this is detected, to minimise the effects (Rolstad and Erwin-Toth, 2004; Chandler, 2015).
Following stoma formation and postoperative complications as mentioned above, peristomal skin is at risk of damage from effluent leakage. Cronin (2008) said the following appliances assist in the prevention of leakage:
Peristomal skin damage
Peristomal irritant/contact dermatitis, inflammation and erosion caused by moisture damage (Boyd, 2014) are the most common stomal complications. Herlufsen et al (2006) reported that leakage causes 77% of skin problems with ileostomies and urostomies. Colwell et al (2011) stated that corrosive enzymes from effluent touching the skin increase the possibility of leaks. There are several causes of skin damage, including:
Granulomas—red areas (nodules) that occur around the edge of the stoma—are not normally painful but can bleed or irritate. Boyd (2010) explained they are caused by friction or irritation caused by effluent or incorrect pouch sizing. It is important to contact a stoma care nurse (SCN) who can review a patient with granulomas and assess whether silver nitrate treatment is required to shrink them.
Physical and psychological consequences
Batalla (2016) reports stoma formation as a life-changing event that can reduce quality of life (QoL). Because of anatomical structural changes and altered functional health, patients have to deal with physiological and psychological issues.
Preoperative counselling promotes postoperative recovery and enhances psychosocial adaptation by preparing ostomates to acquire the skills to live with an altered body (Borwell, 2005; Silva et al, 2017). The stoma is oedematous postoperatively and settles in size over a 6-8 week period. Leakage is a common experience among novice ostomists (within the initial 6-8 weeks) and can contribute to skin breakdown (Butler, 2009).
De Campos (2017) found ostomates reported feelings of stigmatisation, embarrassment, fear of the unknown and discomfort with odours and sounds. These are all reported to be exacerbated when leaks are experienced, making ostomates more likely to withdraw from social activities, which shows that leaks/skin integrity affect QoL (Lee and Morris, 2003; Cottam et al, 2007).
Peristomal skin conditions can occur at any stage but are most common in the first year. The importance of ongoing patient education to maintain skin care regimens and self-care in ensuring good clinical outcomes and patient satisfaction is highlighted by the research of Herlufsen et al (2006), which reported that 67% of ostomates experience mild conditions of which they are not aware.
Provision of good, practical, stoma care education to patients improves outcomes, is part of high-quality care and improves efficiency in nursing services. (Williams, 2012).
Assessing peristomal skin
Several assessment tools for peristomal skin, described in the literature, can be used to formulate an assessment protocol but none are universally accepted as the gold standard (Richbourg et al, 2007; Jemec et al, 2011; Haugen and Ratliff, 2013). The SCOR (Skin Care Ostomy Research) assessment (Williams et al, 2010) is a frequently used assessment tool. Burch (2015) highlighted that treatment will be determined by the result of comprehensive assessments.
The assessment should use terminology to describe and document the extent of skin conditions (Burch, 2014). Skin assessment involves:
See Table 2 for a guide on peristomal skin assessment. Liao and Qin (2014) stated that, through interpersonal relationships, communication, counselling, ongoing education, advice and support, nurses empower patients to self-care and be independent, facilitating emotional adjustment with optimum level of health and wellbeing. Preoperative community education programmes have been shown to reduce the length of hospital stay after a stoma procedure, and preparation for discharge with psychological postoperative education supports patients to acknowledge and manage psychological stressors (Foskett, 2012; Ang et al, 2013).
| Document | Assess changes to | Observe for |
|---|---|---|
|
|
|
|
Borwell (2009), Burton et al (2011), Burch and Slater (2012) and Kelly O'Flynn (2015) all found specialist services to be a valuable resource and ideally placed to empower patients and community healthcare staff during the transition period. They found the role of the SCN assisted psychological adjustment, through clinical expertise, patient education, consultancy and research, preventing hospitalisation of ostomates who presented with complications after discharge, for consolidated teaching (reinforced education).
Treatments
Chandler (2015) reported that early detection prevents unnecessary physical discomfort and reduces more serious complaints. There are no universally agreed treatment algorithms and management is guided by SCNs' experience and opinion (Burch, 2014). Gray et al (2011) stated there are four stages in prevention and treatment:
Treatment strategies are essential to the maintenance of good skin care so it is important to have care pathways to ensure this. Peristomal skin should be inspected regularly for any signs of damage and appropriate cleansers should be used. Rubbing and friction should be avoided when cleaning and drying the skin and the use of barrier creams or films ensuring skin barrier protection should be encouraged. Table 3 describes peristomal skin conditions and how to treat them.
| Condition | Treatment |
|---|---|
| Skin creases | Cleanse the skin, ensure creases are dry, apply barrier cream or film. Fill with paste, strip paste or a seal |
| Leak caused by creases | Cleanse the skin, apply barrier cream/film and level the skin with paste or seals before applying pouch |
| Leak caused by parastomal hernia | Cleanse the skin, apply barrier cream/film, level the skin, and use flexible, convex appliances and hernia support |
| Leak owing to a retracted stoma | Cleanse the skin, apply barrier cream/film, use convex appliances to prevent leaks |
| Skin stripping | Use adhesive removers to prevent irritation to peristomal skin, assess patient's technique and educate, apply barrier film to protect the skin |
| Sore skin | Use protective powder as first line, dusting off excess powder, then use a barrier film or cream. Resize aperture and check patient technique |
| Wet skin | Use protective powder to dry the area, use a cool hairdryer at a distance if very wet to ensure effective adherence of pouch, apply barrier film |
| Folliculitis | Use an adhesive remover and shave the area regularly |
| Pyoderma gangrenosum | Steroid treatment and/or a dermatology review |
Nix (2000) argued the wide range of products available can make it difficult for clinicians to select the optimal one. The consequences of this were highlighted by Hughes (2016), who described patient reports of several products being used, showing inconsistencies in practice with overuse and misuse of products, which can lead to undue expense for the NHS and could lead to poor patient outcomes.
Educating clinicians, patients, their families and carers will help to ensure good skin care management. Voegeli (2012) reported that investing in education for staff on the practice and development of clean skin care protocols can improve patient experience, clinical outcomes and QoL. Table 4 details skin care products and how to use them.
| Product | Use |
|---|---|
| Specialist/protective powder | Dries moist skin, provides protective layer to broken, wet or oozing skin, aiding adhesion of pouch |
| Paste and seals | Mouldable seals are convenient, strip pastes are pliable, pastes are pliable but can sting as they contain alcohol. These aid adhesion, reduce leaks and extend wear time |
| Barrier cream | Prevents skin excoriation by hydrating the skin and restoring skin integrity |
| Barrier film | Creates protective layer for skin by restoring the skin barrier |
| Silicon adhesive remover | Minimises/prevents skin stripping by removing the bond without leaving a residue |
| Hydrocolloid wafer | Absorbs moisture for large excoriated areas |
| Flexible hydrocolloid flanges | Minimise skin maceration protecting skin and absorbs moisture |
| Flange extender | Aids adhesion; not to be used to stops leaks as effluent will gather underneath |
| Stoma collar | Forms a leak-proof barrier around the stoma |
| Convex appliances | Reduce leaks from poorly spouted stomas as they push them into the abdominal wall so the stoma sits further into the pouch |
| Calamine lotion | Soothes sensitive or itchy skin |
| Hairdryer | Dries moist or wet skin before adherence appliance; use a cool setting at a distance |
Peristomal skin protection
Using skin cleansers and barrier films and creams ensure protection against subsequent moisture contact. Barriers form a thin layer, repelling moisture and potential irritants, thus protecting the skin.
Callaghan et al (2018) stated barrier products should be durable, easy to apply, non-sting, gentle on the skin, not interfere with absorbency of pouches, dressings or incontinence wear, have rapid absorption and drying time and be cost effective by minimising product use, resources and time.
A study by Dykes et al (2012) compared two barrier films and found both had a protective effect by delaying the removal of stratum corneum, provided a protective transparent coating that was quickly absorbed while not affecting adhesion of dressings or pouches, and resulted in reduced erythema, excoriation, maceration and reduced pain for patients.
Dykes and Bradbury (2017) and Hughes (2016) highlighted the potential cost-effectiveness of barrier protection because of their durability as effective moisture barrier protection and being wash-off resistant. This would prevent hospitalisation or the need for more healthcare support, while also empowering the ostomate to self-care.
It is important that practitioners become familiar with any products and the manufacturers' guidelines before educating patients on their use.
Conclusion
The aim of good stoma management is to prevent peristomal skin soreness. A majority (70%) of ostomates experience peristomal complications with the most prevalent being skin damage, and healthy peristomal skin is essential for pouch adherence and prevention of effluent leakage.
It is important that practitioners have a good understanding of skin breakdown and how to treat and prevent it. Comprehensive assessment of the skin is used to determine treatment required and early detection prevents unnecessary physical discomfort and reduces more serious complaints.
A wide range of products are available, which can make it difficult for practitioners to select the optimal ones. Misuse of products can affect clinical outcomes, patient satisfaction and QoL and add to the financial burdens to the NHS.
Ongoing education and support should be provided to clinicians, patients, families and carers to assist in maintaining skin care regimens and self-care, ensuring good clinical outcomes, patient satisfaction and QoL, and lower costs.

