The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England (Health Education England (HEE), 2017). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles (Faculty of Intensive Care Medicine, 2018; Royal College of Emergency Medicine, 2019; HEE, 2020; HEE et al, 2020).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions (Young et al, 2020). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature (Table 1), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
Table 1. The diverse range of terms used to refer to clinical reasoning within the healthcare literature
| Category | Sub-categories | Terms identified in Young et al, 2020 | |
|---|---|---|---|
| Reasoning skills | Clinical skills | Critical thinking | |
| Cognitive skill | Reasoning | ||
| Critical reasoning | Reasoning skills | ||
| Reasoning performance | Expert reasoning | Adaptive expertise | Expert reasoning |
| Cognitive expertise | Expertise | ||
| Diagnostic expertise | Medical expertise | ||
| Reasoning competence | Clinical competence | Diagnostic acumen | |
| Clinical performance | Diagnostic performance | ||
| Competency | |||
| Reasoning processes (components) | Cognitive | Analytic reasoning | Inductive and deductive reasoning |
| Analytical thinking | Intuition | ||
| Backward forward reasoning | Intuitive reasoning | ||
| Backward reasoning | Medical information processing | ||
| Bayesian probabilistic thinking | Pattern matching | ||
| Cognitive processes | Pattern recognition | ||
| Heuristics | ‘Street diagnosis’ or ‘In the blink of the eye’ | ||
| Hypothetico-deductive reasoning | |||
| Metacognitive | Metacognition | Self-monitoring | |
| Reflective thinking skills | |||
| Outcome of reasoning | Errors/failures of reasoning | Cognitive bias | Medical error |
| Error prevention | Premature closure | ||
| Judgement errors | Reasoning errors | ||
| Outcome/aim | Choice of treatment | Differential diagnosis | |
| Classification | Management plan | ||
| Clinical management decisions | |||
| Diagnosis | |||
| Quality of outcome | Accuracy | Diagnostic success | |
| Diagnostic accuracy | |||
| Diagnostic and management quality | |||
| Context of reasoning | Dialectical reasoning | Shared understanding | |
| Informed decision making | Situation awareness | ||
| Participatory decision making | Situational judgement | ||
| Shared decision making | |||
| Purpose/goal of reasoning | Different goals of reasoning | Diagnostic justification | |
| Outcome-focused goal of reasoning | Case management | Patient management | |
| Diagnostic reasoning | Therapeutic reasoning | ||
| Diagnostic thinking | Treatment decision making | ||
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ (Rencic et al, 2020).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors (Hayes et al, 2017). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2. Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research (Norman et al, 2017). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit (Table 3). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Table 2. The characteristics of dual process theory
| Characteristics | |
|---|---|
| System 1 (‘default interventionist’) |
|
| System 2 |
|
Table 3. Five strategies to improve teaching and learning
| Explanation | Relevant psychological and educational theory | |
|---|---|---|
| Step 1: Make the ‘thinking process’ explicit |
|
The revised Bloom's taxonomy contain six levels of the cognitive domain:
|
| Step 2: Discuss cognitive biases and de-biasing strategies |
|
|
| Step 3: Model and teach inductive reasoning |
|
|
| Step 4: Use questions to stimulate critical thinking |
|
|
| Step 5: Assess your learner's critical thinking skills |
|
Milestones of critical thinking (Papp et al, 2014) |
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Table 4. The clinical reasoning process within a consultation
| Presenting complaint |
|
| Consider three or more hypotheses relating to diagnosis | Consider the following:
|
| Refine the diagnosis |
|
| Physical examination |
|
| Relevant investigation |
|
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
The construction of a two-by-two square (2 x 2) table (Figure 1) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows (McGee, 2018):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity, the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
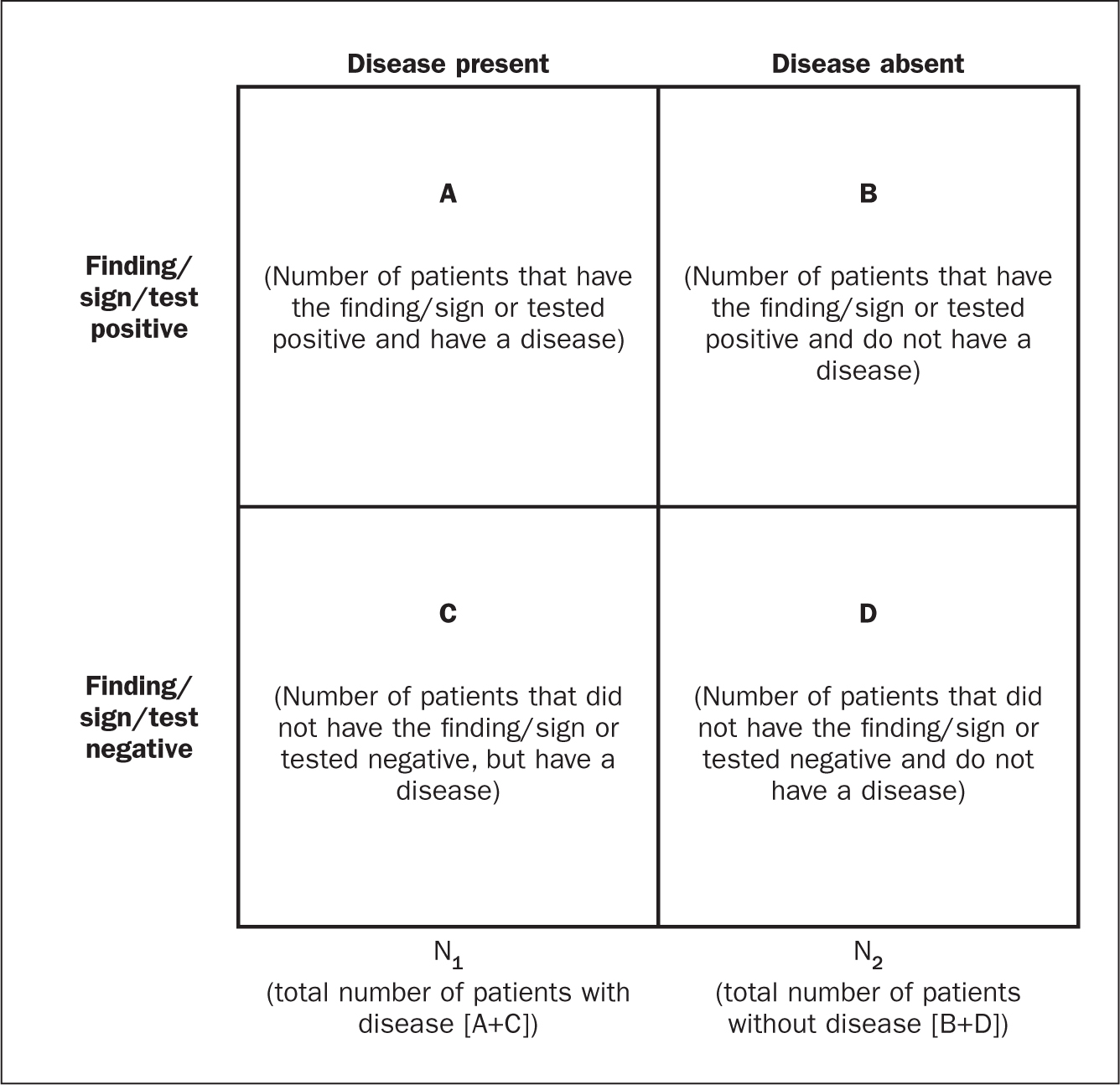 Figure 1. A two-by-two square
Figure 1. A two-by-two square
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
KEY POINTS
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?


