Caring for patients with a neck stoma involves significant clinical complexity for healthcare staff, and is complicated by the fact that most have limited exposure to training on the care of these patients during undergraduate and postgraduate education. This situation is further complicated by the multi-specialty care such patients receive, with no fixed care setting to enable continuity. Safe and effective patient care is dependent on efficient, experienced and confident staff. Landmark studies have consistently highlighted failings in care provision, with themes relating to inadequate staff training, equipment provision and infrastructure, leading to avoidable patient harm and mortality (McGrath et al, 2012). Critically ill patients represent two-thirds of all new tracheostomies performed, with the remaining third undertaken by head and neck surgeons, predominantly for airway obstruction and cancer surgery (McGrath et al, 2012).
Additionally, over the past 15 months or so, global healthcare has experienced an unprecedented surge in the number of critically ill patients with COVID-19 requiring mechanical ventilation as a result of the coronavirus pandemic. The requirement for prolonged periods of ventilation in those who survive, means that many are considered for tracheostomy in order to de-escalate patients from ventilatory support and maximise already depleted resources. The pandemic has also provided additional challenges and concerns through the aerosol-generating nature of neck stomas (Tran et al, 2012). These challenges exist not only during the intra-operative period, but also in the immediate postoperative period.
The ever-evolving pressures on the NHS and demands for intensive care beds both pre- and post-COVID-19, has led to earlier de-escalation of care of neck stoma patients to lower dependency wards. Subsequently, both critical care and ward-based nurses are increasingly required to manage emergency neck stoma-related complications occurring within the immediate postoperative period, with the added risks of contracting COVID-19. Effective management of airway emergencies in such patients requires an awareness of the fundamental anatomical variations between the types of neck stomas, more so during the current pandemic due to increased exposure to neck stoma patients on the wards. Inadequate training and a lack of confidence could result in significant morbidity and potential mortality to both patients and staff.
The authors' novel survey sought to establish perceptions of knowledge and confidence levels relating to the emergency management of neck stomas among nurses within the UK. Additionally, the requirement for further education and the potential for integration of the subject within the undergraduate and postgraduate nursing curricula were explored.
Method
A nationwide prospective survey was formulated and distributed electronically to nurses across all specialties within primary and secondary care. Dissemination platforms included direct contact with hospital trusts and health boards, as well as the Royal College of Nursing and social media. Data were collated over a 2-month capture period between 13 April 2020 and 15 June 2020. Demographic data, previous experience within otolaryngology, completion of advanced life support (ALS) and advanced trauma life support (ATLS), potential areas for development, and knowledge-based questions were also incorporated within the survey (Box 1).
Box 1.Main questions in the electronic survey
- Please state location/hospital; specialty; band
- Do you have any ear, nose and throat (ENT) experience post-qualification? Yes/No
- Are you trained in advanced life support? Yes/No
- Are you trained in advanced trauma life support? Yes/No
- Could you confidently differentiate between a laryngectomy and a tracheostomy patient? Yes/No
- In a tracheostomy patient, how would you administer oxygen?
- Via facemask over the mouth and nose / Via the tracheostomy stoma
- Via both facemask over the mouth and nose and tracheostomy stoma / Unsure
- In a laryngectomy patient, how would you administer oxygen?
- Via facemask over the mouth and nose / Via the laryngectomy stoma
- Via both facemask over the mouth and nose and laryngectomy stoma / Unsure
- Do you feel that you have received adequate training regarding this subject area? Yes/No/Unsure
- Do you feel integrating this subject into the undergraduate or postgraduate curriculum would be beneficial? Yes/No/Unsure
Results
A total of 402 responses were collated over the predefined capture period: 81 from primary care and 321 from secondary care. Respondents were categorised into subgroups based on specialty; 298 respondents included their specialty:
- Head and neck, which included ear nose and throat (ENT) and maxillofacial surgery: n=25
- Accident and emergency: n=43
- Community (general practice, district nursing, and care home nursing): n=81
- Surgery: n=69
- Theatres: n=17
- Intensive therapy/care units (ITU): n=43
- Paediatrics: n=6
- Psychiatry: n=4
- Non-clinical: n=5
- Others, which included nurses working in education, research and corporate roles: n=5.
Respondents were further categorised according to banding: band 5 (n=130); band 6 (n=97); band 7 (n=106); band 8 (n=57) and others, which included nursing students and nurse practitioners (n=12). One hundred and thirty-two respondents cited post-qualification experience within otolaryngology. Advanced life support (ALS) training was completed by 169 respondents (42%) and advanced trauma life support (ATLS) training was completed by 29 respondents (7%).
Perceived confidence in differentiating between tracheostomies and laryngectomies
Overall, 197 respondents (49%) felt they could confidently differentiate between a laryngectomy and a tracheostomy patient. Ninety-two per cent of head and neck nurses (n=23) and 86% of ITU nurses (n=37) felt they could confidently differentiate between a laryngectomy and a tracheostomy patient. Approximately, one third of nurses working in the community, in paediatrics, medicine and other areas (endoscopy unit, resuscitation team, night nurse practitioner) expressed confidence (Figure 1).
 Figure 1. Percentages of nurses in each discipline who were confident in differentiating between different neck stomas
Figure 1. Percentages of nurses in each discipline who were confident in differentiating between different neck stomas
Tracheostomy and laryngectomy care based on specialty and banding
Two questions on administering oxygen to tracheostomy and laryngectomy patients could be scored on a range of 0 to 2. On average, head and neck nurses scored the highest (1.56) on the tracheostomy and laryngectomy knowledge questions. This was followed by non-clinical nursing staff (1.4), theatre nursing staff (1.29), ITU nurses (1.28), surgical nurses (1.26), and A&E nurses (1.12). On average, nurses working in medical specialties (0.99), community (0.9), paediatrics (0.67), and psychiatry (0.5) scored the lowest (Figure 2).
 Figure 2. Total average knowledge scores based on specialty
Figure 2. Total average knowledge scores based on specialty 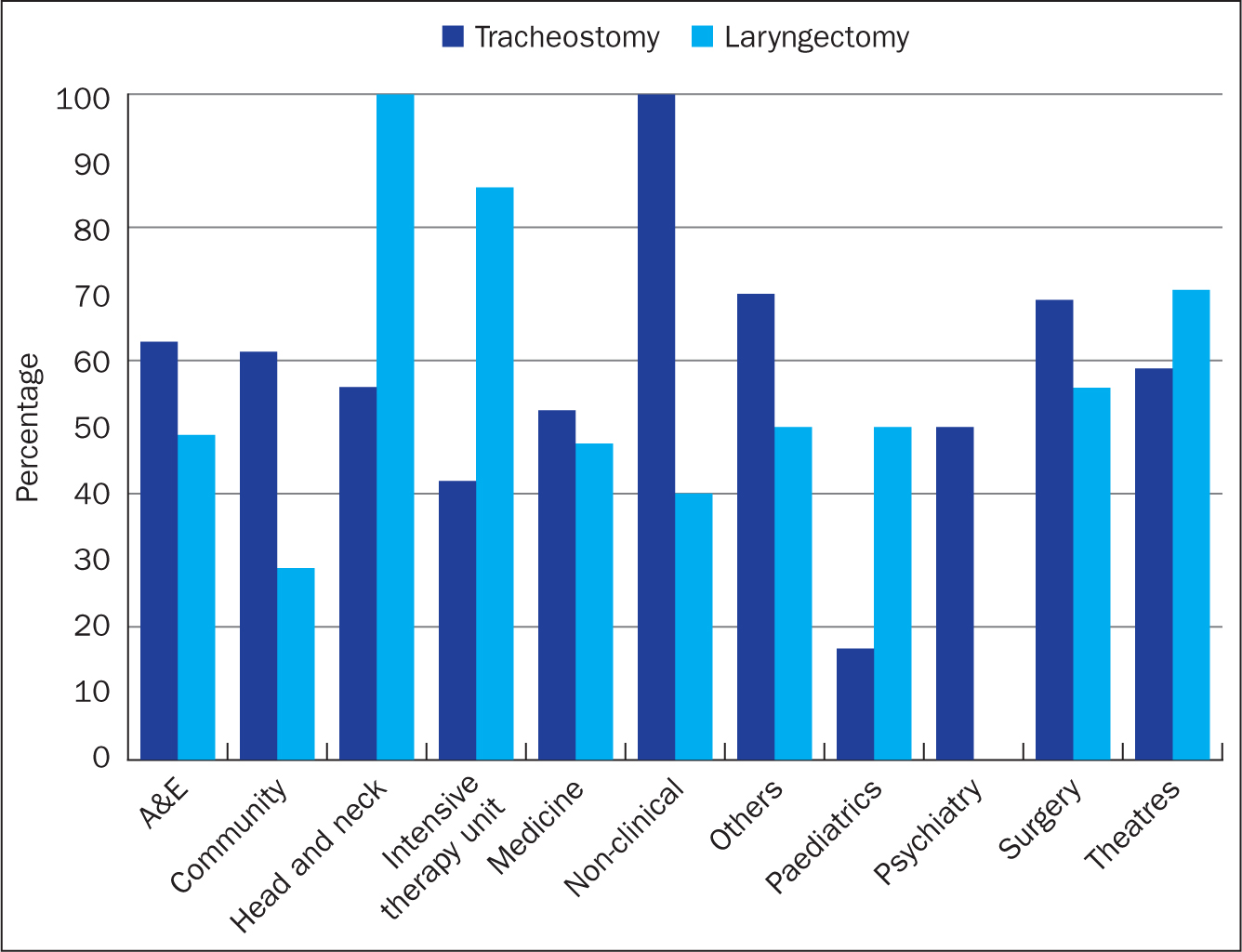 Figure 3. Knowledge scores on neck stoma management by specialty
Figure 3. Knowledge scores on neck stoma management by specialty
No correlation between knowledge and increased banding was identified within the various specialties evaluated.
Tracheostomy care
Overall, 57% (n=231) of respondents correctly identified the need to oxygenate tracheostomy patients over the mouth and nose and over the stoma. All assessed nurses (n=5) working in non-clinical roles identified the correct oxygenation method, while 56% (n=14) of head and neck nurses responded correctly. Conversely, only 16.7% of paediatric nurses identified the correct oxygenation method (Figure 4).
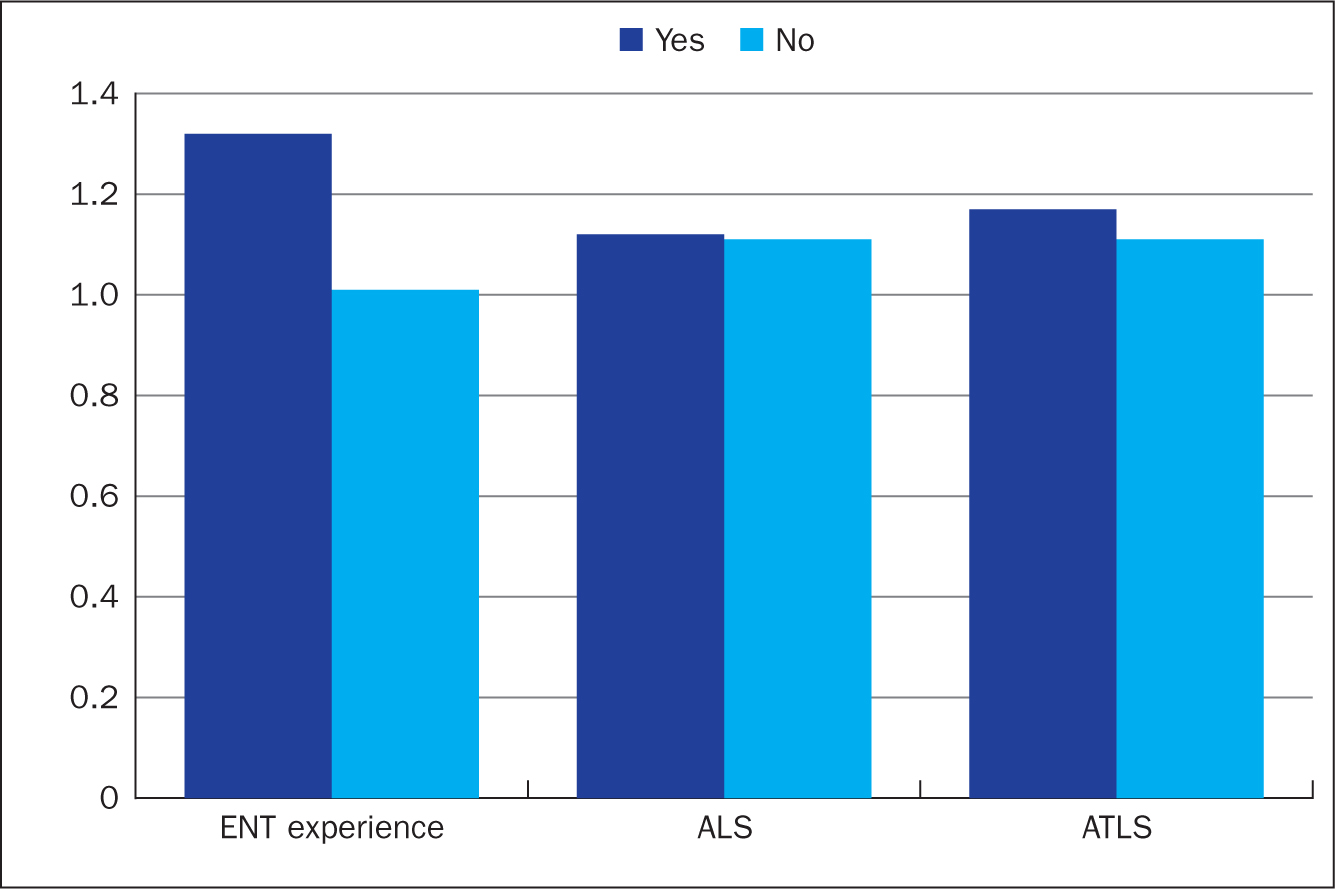 Figure 4. Average score for knowledge-based questions based on ENT experience, ALS and ATLS training
Figure 4. Average score for knowledge-based questions based on ENT experience, ALS and ATLS training
Laryngectomy care
Overall, 54% (n=217) of respondents correctly identified the need to oxygenate directly over the stoma only. In total, 100% of head and neck nurses provided the correct response, followed by 86% (n=37) of ITU nurses, 70.6% (n=12) of theatre nurses and 55.9% (n=38) of surgical nurses. None of the psychiatric nurses identified the correct oxygenation method (Figure 3).
ENT experience, ALS and ATLS training
On average, respondents who cited receiving post-qualification ENT training obtained higher scores (1.32) on the knowledge-based survey questions, in comparison to those who had not (1.01). Findings were similar in those who had received ALS and ATLS training (Figure 4).
Training on tracheostomy and laryngectomy patients
Sixty-five per cent (n=260) of the surveyed cohort cited inadequate training within the field of neck stomas. Twenty-nine per cent (n=118) felt they had received adequate training, while 5.97% were uncertain. Ninety-one per cent (n=365) of responders felt that integration of the subject within the core nursing curriculum would be beneficial.
Discussion
A wide array of complications may occur in the immediate and delayed postoperative period in patients with neck stomas (National Confidential Enquiry into Patient Outcome and Death (NCEPOD), 2014), with nurses invariably being the first responders to such patients. Serious, potentially life-threatening difficulties encountered in this particular patient group include tracheostomy tube displacement or decannulation, obstruction from mucous plugging, and haemorrhage (McGrath et al, 2012).
The recent COVID-19 pandemic has added a further dimension to the challenges encountered when undertaking emergency management of neck stoma patients. Concerns regarding personal safety, particularly given the aerosol-generating nature of managing such patients, have been superimposed on some staff's limited knowledge as a result of a lack of training and confidence (Tran, 2012; Hennessy et al, 2020). The concept of patient-centered care must be balanced against the safety of healthcare workers. Patients must be managed by experienced staff who are trained in the management of patients with altered airway anatomy, highlighting the importance of high-quality training to improve confidence levels (McDonough et al, 2016). Key principles include a focus on essential care, avoidance of unnecessary interventions that may lead to aerosolisation of tracheal secretions, early recognition of deterioration, and timely response to emergencies (McGrath et al, 2016). Airway interventions should be planned in advance, primarily to allow appropriate personal protective equipment (PPE) to be sourced, and to limit potential exposure to staff (Herron et al, 2020).
Difficulties in the management of neck stoma-related emergencies could in part be attributed to a lack of understanding of both normal and altered airway anatomy post-surgery (Darr et al, 2012), as well as a lack of exposure in training. Literature has previously cited variation in comprehension of airway anatomy amongst health professionals (El-Sayed et al, 2010; McDonough et al, 2016), a finding corroborated by the authors' study, with incorrect site of oxygenation reported among the nurse respondents in both tracheostomy (43%, n=171) and laryngectomy patients (46%, n=185). This deficit was, as expected, not as apparent in nurses working within fields of increased exposure to neck stomas, such as maxillofacial and ENT surgery, as well as theatres. The additional experience would simultaneously rationalise the increased knowledge-based scores in nurses working within an intensive care setting, given that the vast majority of acute airway interventions and elective major head and neck resections would have a planned period of observation within this setting. Lower knowledge-based scores within the paediatric nursing cohort would be explained primarily by reduced exposure to adult neck stoma patients, combined with the low numbers of tracheostomies undertaken within the paediatric population (<3% of ICU admissions).
Knowledge deficits will invariably impact on the perceived confidence in managing airway emergencies in neck stoma patients, which was clearly reflected in this survey with as few as 29% of community nurses expressing confidence in differentiating between a tracheostomy and a laryngectomy patient. Despite relatively increased clinical exposure with patients with altered airway anatomy, only 86% of ITU and 92% of head and neck nurses expressed confidence in managing the airway in such patients. It is therefore imperative that all nurses potentially involved in the care of neck stoma patients are confident in appreciating the fundamental anatomical differences (Table 1), to facilitate safe and effective management, while preventing morbidity and mortality (El-Sayed et al, 2010; Darr et al, 2012).
Table 1. Fundamental differences between a tracheostomy and a laryngectomy
| Tracheostomy | Laryngectomy | |
|---|---|---|
| Definition | Opening within trachea | Surgical removal of larynxPharynx anastomosed to oesophagusTrachea exteriorised to neck |
| Duration of use | Usually temporary | Permanent |
| Indications | Upper airway obstructionAirway protectionTracheal toiletAid weaning from ventilation | Advanced laryngeal malignancy |
| Speech | With fenestrated/uncuffed tube with tracheostomy valve | Creation of surgical trachea-oesophageal fistula (TOF)Oesophageal speech or use of electrolarynx |
| Site of oxygenation | Stoma or mouth/nose if non-obstructive pathology and uncuffed tube in situ | Only laryngectomy stoma as no upper airway remains |
Source: adapted from National Tracheostomy Safety Project, 2013; 2021
Finally, the survey demonstrated no additional benefit of increased banding on knowledge, probably because additional postgraduate experience does not necessarily correlate with increased exposure to neck stoma patients.
A multitude of barriers prevent nurses receiving high-quality neck stoma education. One such barrier is limited exposure to neck stomas. In England, a study from 2012 found that more than 5000 tracheostomies and nearly 600 laryngectomies were performed routinely annually (McGrath et al, 2012). In 2014, The Health Foundation stated that around 15 000 tracheostomies are performed each year in England and Wales. Anecdotally, in the authors' experience, the number of laryngectomies performed appears to be increasing. However, the number of procedures undertaken will vary significantly dependent on demographic as well as local factors, such as the size and expertise of the units. Results from this study have highlighted the absence of focused training on both the anatomical and emergency management aspects of neck stomas, with 65% of respondents citing inadequate training during their undergraduate and postgraduate education. Although ATLS courses incorporate the surgical airway, emergency management of neck stoma patients is omitted despite requests made directly to the Resuscitation Council (Darr et al, 2012). Solutions to address educational deficiencies include early exposure through integration of neck stoma care within the nursing undergraduate curriculum, with access to online National Tracheostomy Safety Project (NTSP) (2017) learning modules and practical reinforcement via direct clinical placements. Furthermore, due to the changing needs for COVID-19 patients, regular updates in training could be achieved through simulation training and online learning platforms (Darr et al, 2016).
Conclusion
Care of tracheostomy and laryngectomy patients within the immediate postoperative period requires a multidisciplinary approach, with input from several specialties and levels of expertise. Mortality and morbidity remains significantly high, with nurses often the frontline respondents to deteriorating patients. Safe and effective management requires concise and sustained education of the fundamental anatomical differences between the types of neck stomas, potential complications and their management. The recent COVID-19 pandemic has served to heighten pre-existing apprehension around the management of neck stoma patients, due to their associated aerosol-generating nature. Simulation, coupled with implementation of training modules within the healthcare undergraduate and postgraduate curriculum, may prove crucial in addressing confidence in treating these patients, while simultaneously reducing mortality and morbidity.
Key Points
- Both critical care and ward-based nurses are increasingly required to manage emergency neck stoma-related complications due to the increased incidence and prevalence of head and neck cancer, a higher throughput of cases and earlier de-escalation of neck stoma patients
- Clinical deficits identified by nurses can be attributed to a lack of confidence secondary to reduced clinical exposure and education around the management of neck stoma patients
- COVID-19 and the aerosol generating nature of managing neck stomas has compounded concerns around the management of neck stoma patients
- Integration of neck stoma care within the nursing undergraduate and postgraduate curriculum, coupled with simulation training may address concerns and limit morbidity and mortality
CPD reflective questions
- What factors would you consider to be the main failings in effective management of the neck stoma patient?
- Discuss some of the fundamental differences between a tracheostomy and laryngectomy patient and their stoma
- Describe some of the barriers and solutions to address educational deficiencies regarding neck stoma care


