Undertaking clinical skills is a central part of a nurse's professional role and successful clinical outcomes depend on the competent performance of technical procedures as well as an appropriate level of understanding and a professional attitude (McNett, 2012; Harmon et al, 2016). Therefore, clinical skills teaching is a vital part of the curriculum for pre-registration learners.
There is debate around whether skills teaching is the domain of universities or practice placement settings (Borneuf and Haigh, 2010). Francis (2018) suggests that, as curriculum and practice pressures have changed over time, questions have arisen over who is responsible for clinical skills teaching, with nurse educators not viewing it as their role and clinical staff having insufficient resources to deliver the teaching (Borneuf and Haigh, 2010). Tensions exist between the demands placed on nurse educators to demonstrate excellence in teaching, research and maintaining clinical credibility (Råholm et al, 2016). Leonard et al (2016) argue that nurse educators do not need to undertake regular clinical practice to demonstrate professional credibility in the teaching environment of a university. Although it is suggested that clinical skills should be taught by practitioners in the care setting, in practice the capacity for doing this has declined because of busier environments, increased patient complexity and a more risk-averse culture (Staykova et al, 2017).
The traditional approach to clinical skills acquisition—‘see one, do one, teach one'—is often questioned as it fails to check if the student has learnt a skill correctly and has gained the necessary understanding before practising on patients (Bradley, 2006; Staykova et al, 2017). Some argue that to reduce risk and maintain high standards and safe levels of care, clinical skills teaching should take place, at least in part, in a safe, simulated environment first (McCutcheon et al, 2014; Gonzalez and Kardong-Edgren, 2017).
The new Nursing and Midwifery Council (NMC) standards of proficiency for registered nurses place a significant emphasis on developing a broader range of clinical skills, with the aim of ensuring newly qualified nurses are confident and proficient at the point of registration (NMC, 2018a).
This article discusses some approaches and key concepts around teaching clinical skills.
Teaching clinical skills: context
Harmon et al (2016) state that teaching clinical skills is different from teaching by traditional lectures. To teach a skill, educators need to be competent at performing the skill themselves (Bland et al, 2011; McCutcheon et al, 2015). McNett (2012) highlights this is not always the case. Harmon et al (2016) suggest clinicians who are able to perform a complex clinical procedure routinely can still find it a challenge to move into the role of an educator. All registered nurses are required to support and facilitate learners to develop skills, knowledge and competence (NMC, 2018b), but not all are professionally developed or prepared for this role (Rebeiro et al, 2017).
Haraldseid et al (2015) say capable clinical skills educators are knowledgeable, organised and up to date. This can often make the less confident or less clinically current educators uncomfortable (Harmon et al, 2016; Aldridge, 2017). However, it is suggested that even the most clinically current and competent educators require clinical skills training to ensure their teaching and the demonstration of skills remain consistent (Durham and Baker, 2014). Care must be taken to ensure minimal didactic delivery, with plenty of time for learners to practise.
Herrmann-Werner et al's (2013) study demonstrated that, regardless of method chosen for teaching clinical skills, there is a direct correlation between learner retention and quality of performance in a simulated environment. Further exploration of how clinical skills teaching using simulation may affect service delivery and patient safety in clinical practice is recommended.
Stages of competence
Peyton (1998) advocates moving away from an ‘autopilot’ approach, which is often adopted for routine, day-to-day practice (where the expert is unconsciously competent) to an explicit awareness of precisely what elements of a skill are required to be able to execute a task (the expert becomes consciously competent). Similarly, a novice is often unaware of what they need to learn (they are unconsciously incompetent). Protecting patient safety and enabling learners to become conscious of their limitations to undertake skills (so they become consciously incompetent) is important, as this will make them aware of what they do not know and what they need to know to perform safely.
Dreyfus and Dreyfus (1986) and Benner (1984) describe the ‘novice to expert’ continuum as a framework to position developmental competence. They argue that, through instruction, practice and experience, skills can be mastered. Mastery of complex skills often requires regular practice and application of knowledge (Durham and Baker, 2014).
The novice to expert model identifies the novice learner as someone who has basic reference knowledge, which informs their practice when undertaking a skill, eg taking a set of vital signs and knowing when to escalate. This develops as they become a more advanced learner and their experience develops into coherent and context-specific knowledge eg understanding the underpinning physiology of vital signs and being able to recognise signs and symptoms. This then informs their ability to execute a skill or task with greater understanding.
Development evolves as experience grows and greater, detailed, functional knowledge is acquired, which support a level of competence and ability to think critically when undertaking skills eg taking vital signs while carrying out a more advanced assessment from which direct action can be initiated. When proficiency is achieved (usually within 3-5 years of exposure), learners can complete tasks and skills with ease and are able to apply a much higher level of analytical thinking that develops into expert practice (usually 5 years and longer of exposure) (Benner, 1984). Gobet and Chassy (2008), among others, are critical about the lack of solid evidence to support these stages of development, citing popularity rather than proof of their validity. Despite this, many institutions, academics and practitioners across the globe continue to use this framework to structure their clinical skills-based competency assessments (Gonzalez and Kardong-Edgren, 2017).
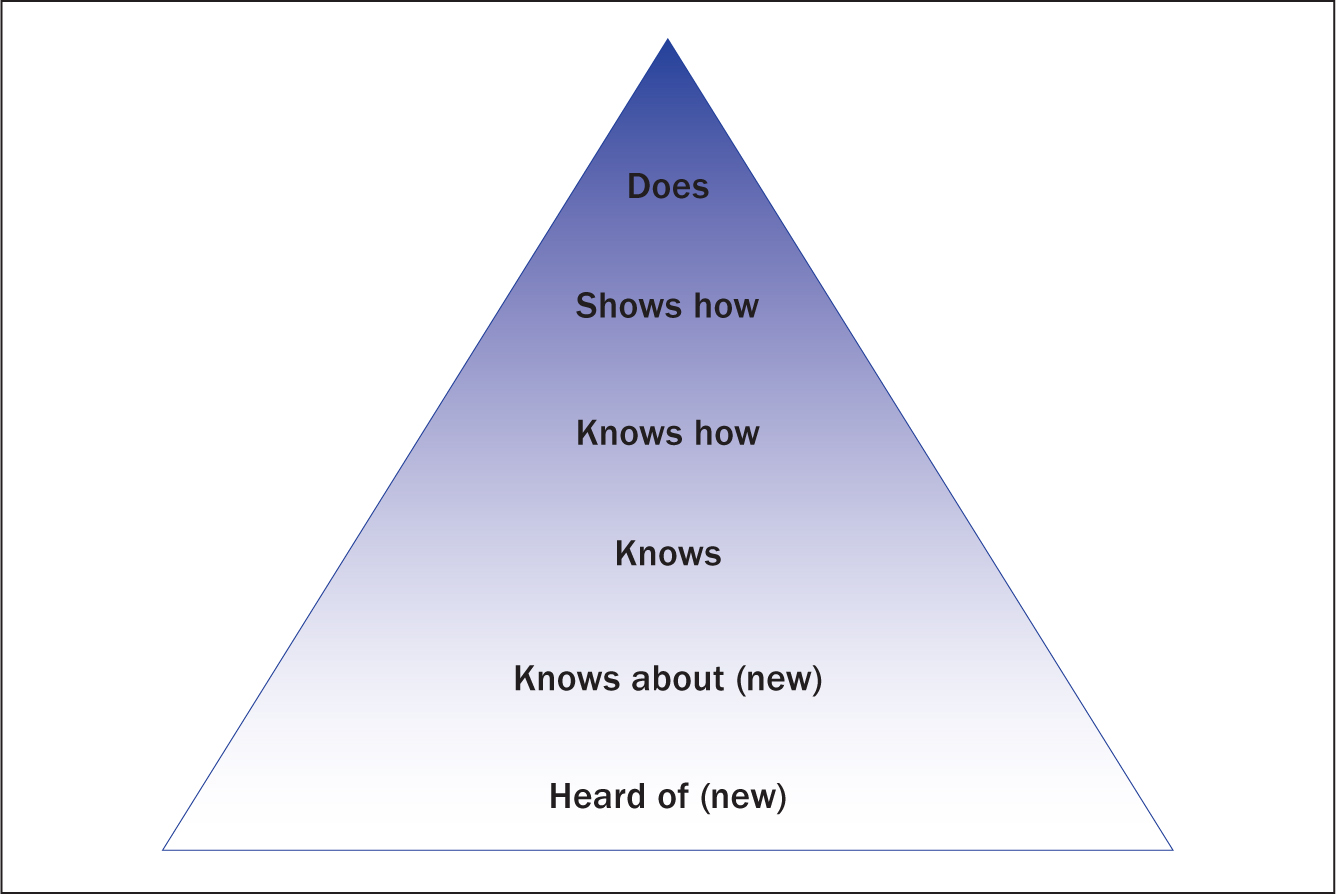
Miller (1990) proposed a pyramid model to determine clinical competency. This distinguishes between knowledge at the lower levels and action in the higher levels. It argues that environment and setting are key for practising and the assessment of skills. Recently, two further stages have been added below ‘knows’; these are ‘heard of’ and ‘knows about’, which help to identify where learners’ understanding starts (Mehay and Burns, 2009). Critics suggest that a superiority or hierarchy of knowledge is implied by this model and, as such, lower level knowledge or competence (such as ‘knows’ or ‘knows how’) could be viewed as inferior (Al-Eraky and Marei, 2016).
Approaches to teaching clinical skills
One standardised approach to teaching clinical skills is Peyton's four-step model (Peyton,1998). This takes a systematic approach to instruction that allows the student to become more familiar with the skill through observation, then listening, followed by talking through the steps and, finally, through practice. It is commonly used in the teaching of basic life support (McNett, 2012).
This model requires the trainer/educator to do the following:
Krautter et al (2011) found that this model was superior to standard instruction with regard to psychomotor skill performance and professionalism. Learners performed the skill to the required standard for the first time more quickly. Nikendei (2014) suggests that this approach is well structured for less confident educators and provides more clarity and opportunities for learners to engage in different ways. Munster et al (2016), however, found no measurable short- or medium-term differences between learners taught using this model and a traditional ‘see one, do one’ method of teaching.
Bradley (2006) suggests that a mixed approach can add value to skills teaching. Gonzalez and Kardong-Edgren (2017) advocate this to accommodate different learning styles and learner preferences. Biggs and Tang (2011) also suggest that watching a recording of a skill procedure can form part of the process. This would free the lecturer to spend time facilitating rather than demonstrating the skill (Rutt, 2017).
Debriefing and feedback are essential components of the learning experience and the acquisition of skills and knowledge (Shinnick et al, 2011). Debriefing is in itself is a form of clinical teaching whereby reflection can contextualise learning to prepare safe and knowledgeable learners (Dreifuerst, 2015; Voyer and Hatala, 2015). Providing feedback is a complex skill (Rush et al, 2012), which often poses challenges for educators (Voyer and Hatala 2015). Providing balanced structured feedback is important and helps to ensure learners feel supported then trusted and more confident to perform the skill independently or under supervision (Bland et al, 2010; McNett, 2012; Race, 2014).
Mentally rehearsing clinical skills, combined with physical practice and subsequent repetition, can increase the confidence, competence and consistency of those performing them (Harmon et al, 2016).
Bloomfield and Jones (2013) explore other ways in which skills are learnt; they describe the significance of using simulated patient scenarios to add context, including videos and manikins as well as virtual/augmented reality to support skills development. Sherwood and Francis (2018) emphasise the superiority of simulation over didactic instruction alone. Doolen et al (2016) suggest that technology alone is not the answer but how it is used in a wider context can contribute to achieving learning outcomes.
Other important factors for achieving learning outcomes include: a safe, non-threatening laboratory-learnt environment, where skills, knowledge and professional attitude can be developed to reach a certain level of competence before exposure to patients; and receiving structured, targeted feedback (Durham and Baker, 2014).
McCutcheon et al (2014) found such approaches strengthen face-to-face teaching of skills and help to provide a structure or ‘scaffold’ the learning for all levels of learner. Vygotsky (1978) defined the concept of the ‘zone of proximal development’ where the gap in knowledge between what the learner currently knows and what they need to know to be deemed competent is addressed. Scaffolding techniques, where the educator collaborates with, supports and guides the learner to achieve competency, can bridge this gap (Sanders and Sugg Welk, 2005). McNett (2012) suggests that competence has been achieved only when a learner can discuss their knowledge (indications, contraindications, complications and their prevention), demonstrate the skill (preparation, technique and dexterity) and consistently display a professional attitude and good communication skills (consent, comfort and dignity of patients, and escalation). Arguably, this suggestion does not discriminate between levels of competence in different levels of learners. Garside and Nhemachena (2011: 541) propose that determining levels of competency is ‘purely in the eye of the beholder’ and, as such, adds to the subjective nature of what competency really is.
Blended learning is defined as a combination of pedagogical approaches that can enhance the learning experience and academic achievement (Poon, 2013). It commonly comprises a combination of online learning and teaching activities including face-to-face methods (Poon, 2013). Blended learning is favoured for its student-centred approach to developing knowledge and understanding via independent learning (Power and Cole, 2017). It offers greater flexibility and has been found to improve learners' autonomy as well as reflection and research skills (Poon, 2013). Different pedagogical approaches are needed to develop the knowledge, skills, professional values and ethical considerations of the learner (Jokinen and Mikkonen, 2013).
The ‘flipped classroom’ learning approach is one such method to enable the learner to acquire and develop their knowledge outside the confines of the classroom or skills laboratory. It involves a reversal of traditional teaching methods where the learner is first exposed to content outside the classroom/skills laboratory (Betihavas et al, 2016). Knowledge gained is then brought into and applied in the educational setting, which allows the educator to spend time on higher-level application of knowledge and skills (El-Banna et al, 2017).
Preparatory work to develop knowledge, such as watching a video of the skill to be mastered, completing an activity such as a quiz or reading a journal article, can be done at a time and place that best suits the learner. Learners are then responsible for coming to class prepared with an understanding of the subject matter to enable them to engage in the class activity (McLaughlin et al, 2014). This has the potential to transform learning that is passive and teacher led to learning that is active and student centred (Reed et al, 2015). Learner knowledge, skills and attitude can then be applied and demonstrated in the safety of the clinical skills laboratory.
This student-centred approach is closely aligned to that of blended learning, where learning is brought to the student rather than the student being brought to the learning, as happens in the classroom (Kho et al, 2018). The flipped classroom approach acknowledges the concept of ‘adult learning’ or andragogy as espoused by Knowles (1975), where learners are active rather than passive participants in learning.
The theory–practice gap, defined as a mismatch between the theoretical content taught in university and the realities of clinical practice (Gardiner and Sheen, 2016), is another concept that can be addressed through simulated clinical skills instruction and learning. Bridging the theory-practice gap is an important aspect of robust pre-registration nurse education and, while enhancing learning, this approach also has the potential to positively affect the delivery of healthcare practice and skills required for lifelong learning (Telford and Senior, 2017).
Problems with skill acquisition
The role of the educator is to ensure an adequate description or demonstration of the task has been given, identifying all the elements of the task; however, learners may have difficulty learning a skill because they lack the physical ability or strength to undertake a task, or have a problem with hand-eye coordination (McNett, 2012; Ewertsson et al, 2015; Haraldseid et al, 2015). Additional time may be required if the learner experiences difficulties. Students may also learn the skill incorrectly in the first place.
They may experience barriers such as anxiety, intimidation or perceived irrelevancy (Harmon et al, 2016). Other issues might include size of the class, level of supervision and guidance and ability to practise the skill (Rutt, 2017).
Application in practice
The more practice a learner gets, the quicker competency is normally achieved (Krautter et al, 2011; Race, 2014). Bland et al (2011) observe that opportunities to practise skills in the current clinical climate can be ad hoc and rushed, and sometimes lack consistency.
The use of simulation to support skill performance in a range of real-time conditions and situations is an important aspect of current teaching and learning strategies (Kunst et al, 2018). Simulation can also help to support clinical skills learning by unpacking human factors eg lack of learner confidence or allowing more time for weaker or slower learners and non-technical skills, which are important in effective collaboration, communication and escalation of care (Bland et al, 2011; McNett, 2012; Ricketts et al, 2012; Merriman et al, 2014).
Kunst et al (2018) suggest that, depending on the learning outcomes, skills development may require a combination of integrated scenario activity, low and high-technology static models, and higher-fidelity simulation. This ensures that learners have the best opportunities to practise their standalone psychomotor skills and more complex activities in context as well as their communication skills in readiness for practice.
The pre-registration NMC (2018) standards of proficiency for registered nurses continue to recognise the importance of clinical skills development and the value of practice learning provided through simulation. Before the new standards were launched, up to 300 hours of clinical skills training could count towards practice hours (NMC, 2010). In the new standards, there is no limit; instead, a less prescriptive approach that will allow greater innovation and development of worthwhile learning experiences for students has been taken (NMC, 2018a). This will enable learners to develop skills necessary for safe and effective practice before they encounter difficult and unpredictable real-world scenarios (Williams and Song, 2016).
Francis (2018) argues that, to ensure robust clinical skills teaching that meets the requirements of the seven NMC platforms of proficiency (NMC, 2018a), educators should be clinically current and knowledgeable in the range of techniques that can be used to teach and facilitate skills development and simulation. This will likely mean more collaboration between higher education institutions and practice partners to achieve the correct balance of teaching and learning strategies, simulation training and real-world hands-on experience.
Conclusion
Clinical skills teaching is a fundamental part of professional pre-registration nursing programmes. Debate around whether skills practice is undertaken in a university, on a practice placement or a combination of both will no doubt continue. However, what is clear is that learners must be practically as well as theoretically prepared for their roles. Through a combination of approaches, it is crucial that clinical skills are robustly taught to ensure the correct levels of knowledge are acquired and practical skills are mastered to ensure patient safety. It is also vital that the right professional attitude is maintained to promote comfort and compassion in the care delivered to patients and clients. Learners should be encouraged to view their competence as a continuum where to maintain safe and informed practice they are required to perform and update their skills regularly.

